Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Viral, bacterial, and fungal contamination of Automated Teller Machines (ATMs)
1
Central Institute for Labour Protection – National Research Institute (CIOP-PIB), Warsaw, Poland
Corresponding author
Rafał L. Górny
Central Institute for Labour Protection – National Research Institute (CIOP-PIB), ul. Czerniakowska 16, 00-701, Warszawa, Poland
Central Institute for Labour Protection – National Research Institute (CIOP-PIB), ul. Czerniakowska 16, 00-701, Warszawa, Poland
Ann Agric Environ Med. 2022;29(3):383-393
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
While the qualitative information about bacterial and fungal pollution of automated teller machine (ATM) surfaces is available in the scientific literature, there are practically no studies precisely quantifying this type of contamination. Regarding viruses, such data in relation to ATM surfaces are not available at all.
Material and methods:
The quantitative and qualitative control of adeno- and coronaviruses, including SARS-CoV-2 (based on qPCR/RT-qPCR and v-qPCR/v-RT-qPCR), bacterial and fungal contaminants (based on morphological and biochemical characteristics followed by PCR/RAPD typing) deposited on internal and external ATM surfaces (swab sampling), as well as present in the air of premises housing the ATM machines (inertial impaction sampling) belonging to the network of one of the largest Polish banks was performed.
Results:
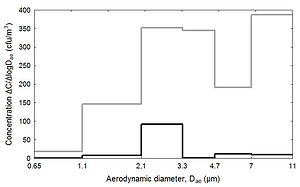
As the air of premises housing ATMs was relatively clean, the internal (i.e. safe boxes and cash dispenser tracks) and external (i.e. touch screens and keypads) ATM surfaces were heavily polluted, reaching 599 CFU/cm2, 522 CFU/cm2, 17288 gc/cm2 and 2512 gc/cm2 for bacterial, fungal, coronaviral and adenoviral contaminants, respectively. The application of propidium monoazide (PMA) dye pretreatment for v-qPCR/v-RT-qPCR allows detection of the potentially infectious SARS-CoV-2 and adenoviral particulates on ATM surfaces.
Conclusions:
The packaged banknotes and people involved in their distribution, as well as general population using ATMs, can be the sources of this type of contamination and its potential victims. Highly efficient hygienic measures should be introduced to prevent unwanted pollution of both the distributed means of payment and ATM surfaces, and to avoid subsequent dissemination of microbial contaminants.
While the qualitative information about bacterial and fungal pollution of automated teller machine (ATM) surfaces is available in the scientific literature, there are practically no studies precisely quantifying this type of contamination. Regarding viruses, such data in relation to ATM surfaces are not available at all.
Material and methods:
The quantitative and qualitative control of adeno- and coronaviruses, including SARS-CoV-2 (based on qPCR/RT-qPCR and v-qPCR/v-RT-qPCR), bacterial and fungal contaminants (based on morphological and biochemical characteristics followed by PCR/RAPD typing) deposited on internal and external ATM surfaces (swab sampling), as well as present in the air of premises housing the ATM machines (inertial impaction sampling) belonging to the network of one of the largest Polish banks was performed.
Results:
As the air of premises housing ATMs was relatively clean, the internal (i.e. safe boxes and cash dispenser tracks) and external (i.e. touch screens and keypads) ATM surfaces were heavily polluted, reaching 599 CFU/cm2, 522 CFU/cm2, 17288 gc/cm2 and 2512 gc/cm2 for bacterial, fungal, coronaviral and adenoviral contaminants, respectively. The application of propidium monoazide (PMA) dye pretreatment for v-qPCR/v-RT-qPCR allows detection of the potentially infectious SARS-CoV-2 and adenoviral particulates on ATM surfaces.
Conclusions:
The packaged banknotes and people involved in their distribution, as well as general population using ATMs, can be the sources of this type of contamination and its potential victims. Highly efficient hygienic measures should be introduced to prevent unwanted pollution of both the distributed means of payment and ATM surfaces, and to avoid subsequent dissemination of microbial contaminants.
REFERENCES (76)
1.
ATM Industry Association: Global ATM installed base to reach 4M by 2021. https://www.atmia.com/news/glo... (access: 2022.07.20).
2.
Banque de France Bulletin no. 232: Article 4. Despite the decline in the use of cash, it remains the most widely used means of payment in France. https://publications.banque-fr... (access: 2022.07.20).
3.
Barbosa JIB, Albano HDCP, Silva F, et al. Microbial contamination of main contact surfaces of Automated Teller Machines from Metropolitan Area of Porto. Int J Environ Stud. 2020;77:208–221. https://doi.org/10.1080/002072....
4.
Özkan VK. Determination of microfungal contamination on automated teller machines and bank cards in Marmaris, Turkey. J Pharm Chem Biol Sci. 2016;3:528–534.
5.
Bik HM, Maritz JM, Luong A, et al. Microbial community patterns associated with automated teller machine keypads in New York City. mSphere 2016;1:e00226–16. https://doi.org/10.1128/mSpher....
6.
Aquino S, de Lima JEA, da Silva MO, et al. Detection of pathogenic bacteria and fungi on biometric surface of Automated Teller Machines located in Brazilian public hospital. Afr J Microbiol Res. 2019;13:219–231. https://doi.org/10.5897/AJMR20....
7.
Dawodu OG, Akanbi RB. Isolation and identification of microorganisms associated with automated teller machines on Federal Polytechnic Ede campus. PLoS ONE 2021;16:e0254658. https://doi.org/10.1371/journa....
8.
Okoro J, Oloninefa SD, Ojonigu AF, et al. Assessment of some selected automated teller machines in Kaduna metropolis for pathogenic bacteria contamination. Br J Environ Stud. 2018;6:19–35.
9.
Allemailem K, Alrasheedi D, Joseph R, et al. A prevalence study of microbial contamination on the surfaces of Automated Teller Machines (ATMs) in Qassim region, Saudi Arabia. J Infect Publ Health 2020;13:338–339. https://doi.org/10.1016./j.jip....
10.
Mahmoudi H, Arabestani MR, Alikhani MY, et al. Antibiogram of bacteria isolated from automated teller machines in Hamadan, West Iran. GMS Hyg Infect Control 2017;12:1–6. https://doi.org/10.3205/dgkh00....
11.
Nagajothi J, Jeyakumari D, Vigneshwaran S, et al. Study of prevalence of microbial contamination with its antibiotic resistance pattern in automated teller machine in and around Puducherry, India. Int J Earth Environ Health Sci. 2015;1:27–31. https://doi.org/10.4103/2423-7....
12.
Hassan M, Honua M. The hygienic and microbial status of Sudanese banknotes, Khartoum state, Sudan. Int J Community Med Pub Health 2017;4:923–927. https://doi.org/10.18203/2394-....
13.
Pereira de Fonseca T, Pessoa R, Sanabani SS. Molecular analysis of bacterial microbiota on Brazilian currency notes surfaces. Int J Environ Res Pub Health 2015;12:13276–13288. https://doi.org/10.3390/ijerph....
14.
Sucilathangam G, Reventh AM, Valvizhi G, et al. Assessment of microbial contamination of paper currency notes in circulation. Int J Current Microbiol Appl Sci. 2016;5:735–741. https://doi.org/10.20546/ijcma....
15.
Snehalatha V, Malashree R, Soni P. Isolation, enumeration and antimicrobial susceptibility of predominant microbes associated with currency notes. Int J Curr Microbiol Appl Sci. 2016;5:650–657. https://doi.org/10.20546/ijcma....
16.
Górny RL, Gołofit-Szymczak M, Wójcik-Fatla A, et al. Microbial contamination of money sorting facilities. Ann Agric Environ Med. 2021;28(1):61–71. https://doi.org/10.26444/aaem/...).
17.
Park GW, Chhabra P, Vinje J. Swab sampling method for the detection of human norovirus on surfaces. J Visual Exp. 2017;120:e55205. https://doi.org/10.3791/55205.
18.
Sánchez-Romero MI, García-Lechuz Moya JM, González López JJ, et al. Collection, transport and general processing of clinical specimens in microbiology laboratory. Enferm Infecc Microbiol Clin. 2019;37:127–134. https://doi.org/10.1016/j.eimc....
19.
Silvestri E, Hall K, Chambers-Velarde Y, et al. Sampling, laboratory and data considerations for microbial data collected in the field. Cincinnati (OH), U.S. Environmental Protection Agency, 2018.
20.
Hong W, Xiong J, Nyaruaba R, et al. Rapid determination of infectious SARS-CoV-2 in PCR-positive samples by SDS-PMA assisted RT-qPCR. Sci Total Environ. 2021;797:149085. https://doi.org/10.1016/j.scit....
21.
Leifels M, Cheng D, Sozzi E, et al. Capsid integrity quantitative PCR to determine virus infectivity in environmental and food applications – A systematic review. Water Res. 2021;11:100080. https://doi.org/10.1016/j.wroa....
22.
Chung YS, Lee NJ, Woo SH, et al. Validation of real-time RT-PCR for detection of SARS-CoV-2 in the early stages of the COVID-19 outbreak in the Republic of Korea. Sci Rep. 2021;11:14817. https://doi.org/10.1038/s41598....
23.
Moreno T, Pintó RM, Bosch A, et al. Tracing surface and airborne SARS-CoV-2 RNA inside public buses and subway trains. Environ Int. 2021;147:106326. https://doi.org/10.1016/j.envi....
24.
Borchardt MA, Boehm AB, Salit M, et al. The Environmental Microbiology Minimum Information (EMMI) guidelines: qPCR and dPCR quality and reporting for environmental microbiology. Environ Sci Technol. 2021;55:10210–10223. https://doi.org/10.1021/acs.es....
25.
Reponen T, Willeke K, Grinshpun SA, et al. Biological particle sampling. In: Kulkarni P, Baron PA, Willeke K, editors. Aerosol Measurements: Principles, Techniques, and Applications. Hoboken; 2011. p. 549–570.
26.
Lagier J-C, Edouard S, Pagnier I, et al. Current and past strategies for bacterial culture in clinical microbiology. Clin Microbiol Rev. 2015;28:208–236. https://doi.org/10.1128/CMR.00....
27.
Fischer G, Dott W. Relevance of airborne fungi and their secondary metabolites for environmental, occupational and indoor hygiene. Arch Microbiol. 2003;179:750–782. https://doi.org/10.1007/s00203....
28.
Domsch KH, Gams W, Anderson TH. Compendium of soil fungi. Eching, IHV Verlag; 1993.
29.
Fisher F, Cook NB. Fundamentals of diagnostic mycology. Philadelphia: Saunders Company; 1998.
30.
Murray PR, Rosenthal KS, Pfaller MA. Medical microbiology. 7th ed. Philadelphia: Elsevier Saunders; 2013.
31.
Samson RA, Hoekstra ES, Frisvad JC. Introduction to food- and airborne fungi. 7th ed. Utrecht: Centraalbureau voor Schimmelcultures; 2004.
32.
St-Germain G, Summerbell R. Identifying fungi: a clinical laboratory handbook. Belmont: Star Publishing; 2011.
33.
Frank JA, Reich CI, Sharma S, et al. Critical evaluation of two primers commonly used for amplification of bacterial 16S rRNA genes. Appl Environ Microbiol. 2008;7:2461–2470. https://doi.org/10.1128/aem.02....
34.
Biasin M, Bianco A, Pareschi G, et al. UV-C irradiation is highly effective in inactivating SARS-CoV-2 replication. Sci Rep. 2021;11:6260. https://doi.org/10.1038/s41598....
35.
Freeman S, Kibler K, Lipsky Z, et al. Systematic evaluating and modeling of SARS-CoV-2 UVC disinfection. Sci Rep. 2022;12:5869. https://doi.org/10.1038/s41598....
36.
Gidari A, Sabbatini S, Bastianelli S, et al. SARS-CoV-2 survival on surfaces and the effect of UV-C light. Viruses 2021;13:408. https://doi.org/10.3390/v13030....
37.
Sobotka P, Przychodzki M, Uściło K, et al. Effect of ultraviolet light C (UV-C) radiation generated by semiconductor light sources on human beta-coronaviruses’ inactivation. Materials. 2022;15:2302. https://doi.org/10.3390/ma1506....
38.
Kemp P, Neumeister-Kemp H. Australian mould guideline. Osborne Park: Enviro Trust; 2010.
39.
Pośniak M, Skowroń J. Harmful agents in working environment. Limit values. Warsaw: CIOP; 2020.
40.
Górny RL. Microbial aerosols: sources, properties, health effects, exposure assessment – a review. KONA Powder Particle J. 2020;37:64–84. https://doi.org/10.14356/kona.....
41.
McCullough NV, Brosseau LM, Vesley D. Collection of three bacterial aerosols by respirator and surgical mask filters under varying conditions of flow and relative humidity. Ann Occup Hyg. 1997;41:6777–6790. https://doi.org/10.1016/S0003-....
42.
Reponen T, Willeke K, Ulevicius V, et al. Effect of relative humidity on the aerodynamic diameter and respiratory deposition of fungal spores. Atmos Environ. 1996;30:3967–3974.
43.
Simon X, Duquenne P. Feasibility of generating peaks of bioaerosols for laboratory experiments. Aerosol Air Quality Res. 2013;13:877–886. https://doi.org/10.4209/aaqr.2....
44.
Abirami B, Kumar T, Saravanamuthu R. Studies on the fungal flora of Indian currency. Asian J Res Pharm Sci. 2012;2:33–36. https://doi.org/10.52711/2231-....
45.
Alwakeel SS, Naseer AL. Bacterial and fungal contamination of Saudi Arabian paper currency and cell phones. Asian J Biol Sci. 2011;4:556–562. https://doi.org/10.3923/ajbs.2....
46.
Ayandele AA, Adeniyi SA. Prevalence and antimicrobial resistance pattern of microorganisms isolated from Naira notes in Ogbomoso North, Nigeria. J Res Biol. 2011;8:587–593.
47.
Dehghani M, Dehghani V, Estakhr J. Survey of microbial contamination of Iranian currency papers. Res J Pharm Biol Chem Sci. 2011;2:242–248.
48.
Flannigan B, Samson R, Miller JD, editors. Microorganisms in home and indoor work environments: diversity, health impacts, investigation and control. 2nd ed. Boca Raton: CRC Press – Taylor and Francis; 2011.
49.
Kumar P, Singh AB, Singh R. Comprehensive health risk assessment of microbial indoor air quality in microenvironments. PLoS ONE 2022;17:e0264226. https://doi.org/10.1371/journa....
50.
Ławniczek-Wałczyk A, Górny RL. Endotoxins and ß-glucans as markers of microbiological contamination – characteristics, detection, and environmental exposure. Ann Agric Environ Med. 2010;17:193–208.
51.
Amanah A, Apriyanto DR, Fitriani H. Isolation of surveillance pathogenic fungal microbial contaminant on mobile phone. Open Access Maced J Med Sci. 2019;7:3493–3496. https://doi.org/10.3889/oamjms....
52.
Kordecka A, Krajewska-Kułak E, Łukaszuk C, et al. Isolation frequency of Candida present on the surfaces of mobile phones and hands. BMC Infect Dis. 2016;16:238. https://doi.org/10.1186/s12879....
53.
Krzyściak P, Skóra M, Macura AB. Atlas of human pathogenic fungi. Wrocław: Medpharm; 2011.
54.
Chiller K, Selkin BA, Murakawa GJ. Skin microflora and bacterial infections of the skin. J Investig Dermatol Symp Proc. 2001;6:170–174. https://doi.org/10.1046/j.0022....
56.
Commission Directive (EU) 2019/1833 of 24 October 2019 amending Annexes I, III, V and VI to Directive 2000/54/EC of the European Parliament and of the Council as regards purely technical adjustments. OJ. 2019;L 279:54–79.
57.
Commission Directive (EU) 2020/739 of 3 June 2020 amending Annex III to Directive 2000/54/EC of the European Parliament and of the Council as regards the inclusion of SARS-CoV-2 in the list of biological agents known to infect humans and amending Commission Directive (EU) 2019/1833. OJ. 2020;L 175:11–14.
58.
Ordinance of the Minister of Health of 11 December 2020 amending ordinance on hazardous biological agents in the work environment and the protection of health of workers occupationally exposed to them. Law Gazette 2020, pos. 2234.
59.
Di Bella M, Randazzo D, Di Carlo E, et al. Monitoring biological damage on paper-based documents in the historical archive of the Palermo astronomical observatory. In: Conservation Science in Cultural Heritage; 2015. p. 85–94.
60.
Hagaggi NSA. Biodegradation of cellulosic raw materials by extracellular carboxymethyl cellulose produced by Exiguobacterium aurantiacum. Egypt J Exp Biol (Bot). 2018;14:11–18. https://doi.org/10.5455/egyjeb....
61.
Kwaśna H, Karbowska-Berent J, Behnke-Borowczyk J. Effect of fungi on the destruction of historical parchment and paper documents. Pol J Environ Stud. 2020;29:2679–2695. https://doi.org/10.15244/pjoes....
62.
Sterflinger K. Fungi: their role in deterioration of cultural heritage. Fungal Biol Rev. 2010;24:47–55. https://doi.org/10.1016/j.fbr.....
63.
Strzelczyk-Brąszkiewicz AB. Biodeterioration of historic objects by microorganisms and insects. Toruń: Wydawnictwo Adam Marszałek; 2012.
64.
Urzi C, de Leo F. Biodeterioration of Cultural Heritage in Italy: State of Art. Proceedings of ARIADNE 8 Workshop; 2001; Prague, Czech Republic. Prague: Academy of Sciences of the Czech Republic; 2001.
65.
Zyska B. Fungi isolated from library materials: A review of the literature. Int Biodeterior Biodegrad. 1997;40:43–51. https://doi.org/10.1016/S0964-....
66.
Samson RA. Ecology and general characteristics of indoor fungi. In: Adan OCG, Samson RA, editors. Fundamentals of Mold Growth in Indoor Environments and Strategies for Healthy Living. Wageningen; 2011. p. 101–116.
67.
Mandrioli P, Caneva G, Sabbioni C. Cultural heritage and aerobiology. Methods and measurement techniques for biodeterioration monitoring. Dordrecht: Kluwer Academic Publishers; 2003.
69.
Riddell S, Goldie S, Hill A, et al. The effect of temperature on persistence of SARS-CoV-2 on common surfaces. Virol J. 2020;17:145. https://doi.org/10.1186/s12985....
70.
Zayas G, Chiang MC, Wong E, et al. Cough aerosol in healthy participants: fundamental knowledge to optimize droplet-spread infectious respiratory disease management. BMC Pulm Med. 2012;12:11. https://doi.org/10.1186/1471-2....
71.
Li H, Leong FY, Xu G, et al. Airborne dispersion of droplets during coughing: a physical model of viral transmission. Sci Rep. 2021;11:4617. https://doi.org/10.1038/s41598....
72.
Stobnicka-Kupiec A, Gołofit-Szymczak M, Górny RL, et al. Prevalence of Bovine Leukemia Virus (BLV) and Bovine Adenovirus (BAdV) genomes among air and surface samples in dairy production. J Occup Environ Hyg. 2020;17:312–323. https://doi.org/10.1080/154596....
73.
Kramer A, Schwebke I, Kampf G. How long do nosocomial pathogens persist on inanimate surfaces? A systematic review. BMC Infect Dis. 2006;6:130. https://doi.org/10.1186/1471-2....
74.
Dutkiewicz J, Mackiewicz B, Lemieszek MK, et al. Pantoea agglomerans: a mysterious bacterium of evil and good. Part III. Deleterious effects: infections of humans, animals and plants. Ann Agric Environ Med. 2016;23:197–205. https://doi.org/10.5604/123219....
75.
Brisebois E, Veillette M, Dion-Dupont V, et al. Human viral pathogens are pervasive in wastewater treatment center aerosols. J Environ Sci. 2018;67:45–53. https://doi.org/10.1016/j.jes.....
76.
Hung L-L, Miller JD, Dillon K, editors. Field guide for the determination of biological contaminants in environmental samples. 2nd ed. Fairfax: AIHA; 2005.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.