Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
The risk of blood-borne infections in Poland – opportunities and threats to public health, nationwide qualitative research
1
National Institute of Public Health, Warsaw, Poland
2
Collegium Medicum, Cardinal Stefan Wyszynski University in Warsaw, Poland
3
Higher School of Logistics, Warsaw, Poland
4
Department of Public Health, Medical University of Warsaw, Poland
Corresponding author
Ann Agric Environ Med. 2021;28(3):469-474
KEYWORDS
TOPICS
Biological agents posing occupational risk in agriculture, forestry, food industry and wood industry and diseases caused by these agents (zoonoses, allergic and immunotoxic diseases)Prevention of occupational diseases in agriculture, forestry, food industry and wood industry
ABSTRACT
Introduction:
The article presents the diagnosis of the problem of blood-borne infections in Poland from perspectives of experts’ opinions at the voivodship level. The evaluation became the basis for subsequent analysis, aimed at creating assumptions for the proposed strategies to prevent blood-borne infections in Poland.
Material and methods:
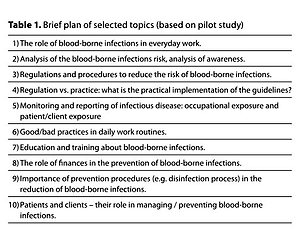
Diagnosis was based on the expertise of practitioners in epidemiology and service providers. Analysis covered assessment of service safety, examples, recommended practices, forms and scope of education. Also covered is information for the general public from different aspects: points of view of recipients and service providers, legislation, system organization, and finances. The SWOT method was used in analysis. The opportunities and threats concerning the risk of blood-borne diseases for the service sector are presented, as well as data gathered from 42 representative experts from across Poland.
Results:
Databases on health indicators, covered by the reporting obligation of all diagnosed cases, are a crucial element of the surveillance system in public health (e.g. sentinel). Additional information on health care management (risk management) is not a common and routine approach. The study fills a gap in knowledge about risk management in the medical and non-medical services sector. The information also enriches education programmes (e.g. http://www.hcv.pzh.gov.pl/).
Conclusions:
Currently, the evidence-based approaches in medicine and in public health are standard. Experts emphasize that the opportunities for the prevention of infection risk are linked to technological advances and innovations, while threats are seen in both financial and organizational constraints, and the non-normalized, dynamically developing service market.
The article presents the diagnosis of the problem of blood-borne infections in Poland from perspectives of experts’ opinions at the voivodship level. The evaluation became the basis for subsequent analysis, aimed at creating assumptions for the proposed strategies to prevent blood-borne infections in Poland.
Material and methods:
Diagnosis was based on the expertise of practitioners in epidemiology and service providers. Analysis covered assessment of service safety, examples, recommended practices, forms and scope of education. Also covered is information for the general public from different aspects: points of view of recipients and service providers, legislation, system organization, and finances. The SWOT method was used in analysis. The opportunities and threats concerning the risk of blood-borne diseases for the service sector are presented, as well as data gathered from 42 representative experts from across Poland.
Results:
Databases on health indicators, covered by the reporting obligation of all diagnosed cases, are a crucial element of the surveillance system in public health (e.g. sentinel). Additional information on health care management (risk management) is not a common and routine approach. The study fills a gap in knowledge about risk management in the medical and non-medical services sector. The information also enriches education programmes (e.g. http://www.hcv.pzh.gov.pl/).
Conclusions:
Currently, the evidence-based approaches in medicine and in public health are standard. Experts emphasize that the opportunities for the prevention of infection risk are linked to technological advances and innovations, while threats are seen in both financial and organizational constraints, and the non-normalized, dynamically developing service market.
ABBREVIATIONS
SWOT – Strengths, Weaknesses, Opportunities, Threats; WHO – World Health Organization; HCV – Hepatitis C Virus; HBV– Hepatitis B Virus; HIV – Human Immunodeficiency Virus; NGO – Non-Governmental Organization; NIPH-NIH – National Institute Public Health/National Institute of Hygiene; US CDC – Centers for Disease Control of United States
REFERENCES (37)
1.
WHO. Combating Hepatitis B and C to Reach Elimination by 2030. 2016 https://apps.who.int/iris/bits...; jsessionid=23CD570FA9986402B8961AC37A2C2E4B?sequence=1 (Accessed 07.06.2020).
2.
Chiu KP, Yu AL. Application of cell-free DNA sequencing in characterization of blood borne microbes and the study of microbe-disease interactions. Peer J. 2019; 7: e7426. Published 2019 Aug 6. doi: 10.7717/peerj.7426.
3.
Jaichenco AL, Lima LC. Infectious Disease Considerations for the Operating Room. A Practice of Anesthesia for Infants and Children. 2019; 1146–1160.e4. doi: 10.1016/B978-0-323-42974-0.00050-1.
4.
Mannucci PM. Viral safety of coagulation factor concentrates: memoirs from an insider. J Thromb Haemost. 2018; 16(4): 630–633. doi: 10.1111/jth.13963.
5.
CDC. General Resources on Bloodborne Pathogens. Bloodborne Infectious Diseases (HIV/AIDS, Hepatitis B & C). https://www.cdc.gov/niosh/topi... (Accessed 02.06.2020).AAEMAnnals of Agricultural and Environmental Medicine.
6.
Ogunremi T, Defalco K, Lynn Johnston B, et al. 1208. Preventing Transmission of Bloodborne Viruses from-Infected Healthcare Workers to Patients in Canadian Healthcare Settings: A National Guideline. Open Forum Infect Dis. 2019; 6 (Suppl 2): S434. Published 2019 Oct 23. doi: 10.1093/ofid/ofz360.1071.
7.
Ogunremi T, Defalco K, Johnston BL, et al. Preventing transmission of bloodborne viruses from infected healthcare workers to patients: Summary of a new Canadian Guideline. Can Commun Dis Rep. 2019; 45(12): 317–322. Published 2019 Dec 5. doi: 10.14745/ccdr.v45i12a03.
8.
Verbeek J, Basnet P. Incidence of sharps injuries in surgical units, a meta-analysis and meta-regression. Am J Infect Control. 2019; 47(4): 448–455. doi: 10.1016/j.ajic.2018.10.003.
9.
Bouya S, Balouchi A, Rafiemanesh H, et al. Global Prevalence and Device Related Causes of Needle Stick Injuries among Health Care Workers: A Systematic Review and Meta-Analysis. Ann Glob Health. 2020; 86(1): 35. Published 2020 Apr 6. doi: 10.5334/aogh.2698.
10.
Public Health England Health and Justice Review 2017/18. https://assets.publishing.serv... (Accessed 02.06.2020).
11.
WHO. Progress report on access to hepatitis C treatment. Geneva: World Health Organization; 2018. https://apps.who.int/iris/bits... (Accessed 02.06.2020).
12.
WHO. Global health estimates 2016. Geneva: World Health Organization; 2016. https://www.who.int/healthinfo... (Accessed 02.06.2020).
14.
Nicholson F. Infectious Diseases: The Role of the Healthcare Professional. Clin Forensic Med. 2020; 343–392. Published 2020 Jan 2. doi: 10.1007/978-3-030-29462-5_10.
15.
Stockdale AJ, Kreuels B, Henrion MYR, et al. The global prevalence of hepatitis D virus infection: systematic review and metaanalysis. J Hepatol. 2020. doi: https://doi.org/10.1016/j.jhep....
17.
Carter M. HIV and Chronic HCV co-infection prevalence in England highest with MSM. 2018 https://www.aidsmap.com/news/a... (Accessed 02.06.2020).
18.
UK Cresswell F, Waters L, Briggs E, et al. UK guideline for the use of HIV Post-Exposure Prophylaxis Following Sexual Exposure, 2015. Int J Std AIDS. 2016; 27(9): 713–738. doi: 10.1177/0956462416641813.
19.
Hawkins DA, Asboe D, Barlow K, Evans B. Seroconversion to HIV-1 following a needlestick injury despite combination post-exposure prophylaxis. J Infect. 2001; 43(1): 12–15. doi: 10.1053/jinf.2001.0811.
20.
Razavi H, El Khoury AC, Elbasha E, et al. Chronic hepatitis C virus (HCV) disease burden and cost in the United States. Hepatology 2013; 57: 2164 –70.
22.
Hagan H, Jordan AE, Neurer J, Cleland CM. Incidence of sexually transmitted hepatitis C virus infection in HIV-positive men who have sex with men. AIDS. 2015; 29: 2335–45.
23.
WHO, Progress report on HIV, viral hepatitis and sexually transmitted infections, Accountability for the global health sector strategies, 2016–2021, 2019. https://www.who.int/publicatio... (accessed 03.06.2020).
24.
WHO, Global health sector strategy on viral hepatitis 2016–21, 2016 https://apps.who.int/iris/bits....
25.
Fitz Simons D, Francois G, De Carli G, et al. Hepatitis B virus, hepatitis C virus and other blood-borne infections in healthcare workers: guidelines for prevention and management in industrialized countries. Occup Environ Med. 2008; 65: 446–51.
26.
Rice BD, Tomkins SE, Ncube FM. Sharp truth: health care workers remain at risk of bloodborne infection. Occup Med. (Lond). 2015; 65: 210 –14.
27.
Rybacki M, Piekarska A, Wiszniewska M, Walusiak-Skorupa J. Hepatitis B and C infection: is it a problem in Polish healthcare workers? Int J Occup Med Environ Health 2013; 26: 430–39.
28.
Winchester SA, Tomkins S, Cliffe S, Batty L, Ncube F, Zuckerman M. Healthcare workers’ perceptions of occupational exposure to blood-borne viruses and reporting barriers: a questionnaire-based study. J Hosp Infect. 2012; 82: 36–39.
29.
Wakefield MA, Loken B, Hornik RC. Use of mass media campaigns to change health behaviour. Lancet 2010; 376: 1261–71.
30.
McLean HS, Carriker C, Bordley WC. Good to Great: Quality-Improvement Initiative Increases and Sustains Pediatric Health Care Worker Hand Hygiene Compliance. Hosp Pediatr. 2017; 7: 189–96.
31.
Chen MF, Hung SL, Chen SL. Empowerment Program for People With Prediabetes: A Randomized Controlled Trial. J Nurs Res. 2017; 25: 99–111.
33.
Arora P, Kumari S, Sodhi J, et al. Gloves Reprocessing: Does It Really Save Money? Indian J Surg. 2015; 77 (Suppl 3): 1291–94.
34.
Larose E. Legal implications of single-use medical device reprocessing. Health Q 2013; 16: 48–52.
36.
Sukhera J, Miller K, Milne A, et al. Watling C. Labelling of mental illness in a pediatric emergency department and its implications for stigma reduction education. Perspect Med Educ. 2017; 6: 165–72.
37.
Hamilton JB, Worthy VC, Moore AD, et al. Messages of Hope: Helping Family Members to Overcome Fears and Fatalistic Attitudes Toward Cancer. 2017; 32: 190–97.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.