Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
The response of primary care practices in rural and urban settings in Poland to the challenges of the COVID-19 pandemic
1
Department of Family Medicine, Jagiellonian University Medical College, Kraków, Poland
2
Department of Public Health and Primary Care, Ghent University, Belgium
Corresponding author
Katarzyna Nessler
The Department of Family Medicine, Jagiellonian University Medical College, Bocheńska 4, 31-061, Kraków, Poland
The Department of Family Medicine, Jagiellonian University Medical College, Bocheńska 4, 31-061, Kraków, Poland
Ann Agric Environ Med. 2022;29(4):575-581
KEYWORDS
quality of careinfectious diseasesfamily medicinegeneral practiceprimary healthcareCOVID-19PRICOV-19
TOPICS
ABSTRACT
Introduction:
In the wake of COVID-19 primary care practices have had to overcome and to adapt to several challenges in providing quality care. An international consortium led by Ghent University, Belgium, set up the PRICOV-19 project to study how primary care practices in 38 countries responded to the new challenges.
Objective:
The aim of the study was to describe how Covid-19 impacted the organisation of primary care practices in rural and urban environments in Poland, including the organisation of patient flows, infection prevention, information processing, and communication.
Material and methods:
This is cross-sectional questionnaire-based survey among primary care practices. In Poland, the survey was distributed among primary care practices in 16 Polish regions. 180 practices participated in the study. In the analysis of the data U-Mann Whitney or t-test for independent groups, and Wilcoxon test were used to compare the organisation of care before and since the pandemic.
Results:
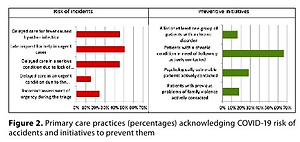
Over two-thirds of practices made considerable changes in their structure due to COVID-19; over three-quarters introduced security procedures for phone registrations, but only a quarter still offered consultations without a prior appointment. The use of video consultation quadrupled, and teleconsultations became almost universal. Rural practices were significantly more likely to offer active care for deprived patient groups. A significant increase in infection prevention measures occurred in both urban and rural practices.
Conclusions:
COVID-19 brought challenges that spurred changes to the organisation of primary care practices as they sought to continue offering quality care. Despite these hardships, new opportunities for effective changes to clinical operations and organization have emerged and will benefit global health systems in the face of new crises.
In the wake of COVID-19 primary care practices have had to overcome and to adapt to several challenges in providing quality care. An international consortium led by Ghent University, Belgium, set up the PRICOV-19 project to study how primary care practices in 38 countries responded to the new challenges.
Objective:
The aim of the study was to describe how Covid-19 impacted the organisation of primary care practices in rural and urban environments in Poland, including the organisation of patient flows, infection prevention, information processing, and communication.
Material and methods:
This is cross-sectional questionnaire-based survey among primary care practices. In Poland, the survey was distributed among primary care practices in 16 Polish regions. 180 practices participated in the study. In the analysis of the data U-Mann Whitney or t-test for independent groups, and Wilcoxon test were used to compare the organisation of care before and since the pandemic.
Results:
Over two-thirds of practices made considerable changes in their structure due to COVID-19; over three-quarters introduced security procedures for phone registrations, but only a quarter still offered consultations without a prior appointment. The use of video consultation quadrupled, and teleconsultations became almost universal. Rural practices were significantly more likely to offer active care for deprived patient groups. A significant increase in infection prevention measures occurred in both urban and rural practices.
Conclusions:
COVID-19 brought challenges that spurred changes to the organisation of primary care practices as they sought to continue offering quality care. Despite these hardships, new opportunities for effective changes to clinical operations and organization have emerged and will benefit global health systems in the face of new crises.
REFERENCES (26)
1.
Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak – an update on the status. Military Med Res. 2020;7(1):11. doi:10.1186/s40779-020-00240-0.
2.
COVID-19 Map. Johns Hopkins Coronavirus Resource Center. Accessed July 13, 2022. https://coronavirus.jhu.edu/ma....
3.
Thornton J. Covid-19: how coronavirus will change the face of general practice forever. BMJ. 2020;368:m1279. doi:10.1136/bmj.m1279.
4.
Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century. National Academies Press (US); 2001. Accessed December 18, 2021. http://www.ncbi.nlm.nih.gov/bo....
6.
Desborough J, Dykgraaf SH, Phillips C, Wright M, Maddox R, Davis S, Kidd M. Lessons for the global primary care response to COVID-19: a rapid review of evidence from past epidemics. Fam Pract. 2021 Nov 24;38(6):811–825.
7.
Van Poel E, Vanden Bussche P, Klemenc-Ketis Z, Willems S. How did general practices organize care during the COVID-19 pandemic: the protocol of the cross-sectional PRICOV-19 study in 38 countries. BMC Prim Care. 2022;23(1):11. Published 2022 Jan 15. doi:10.1186/s12875-021-01587-6.
8.
Ghent University PRICOV-19 Team. (n.d.). PRICOV-19 STUDY: A cross-sectional study in 38 countries on the organization of care in general practices during the COVID-19 pandemic. PRICOV-19 Study: Quality and Safety in Primary Care in Times of COVID-19. Retrieved June 6, 2022, from https://pricov19study.ugent.be....
9.
Grossman Z, Chodick G, Reingold SM, Chapnick G, Ashkenazi S. The future of telemedicine visits after COVID-19: perceptions of primary care pediatricians. Isr J Health Policy Res. 2020 Oct 20;9(1):53. doi: 10.1186/s13584-020-00414-0. PMID: 33081834; PMCID: PMC7573530.
10.
Saint-Lary O, Gautier S, Le Breton J, Gilberg S, Frappé, Schuers M, Bourgueil Y, Renard V. How GPs adapted their practices and organisations at the beginning of COVID-19 outbreak: a French national observational survey. BMJ Open 2020;10:e042119. doi:10.1136/bmjopen-2020-042119.
11.
Groenewegen P, van den Muijsenbergh M, Batenburg R, Van Poel E, van den Broek S, Bussche PV, Willems S. Snelle aanpassing praktijkorganisatie tijdens de coronapandemie. Huisarts Wet. 2022;65(5):16–20. Dutch. doi:10.1007/s12445-022-1439-5. Epub 2022 Apr 1. PMID: 35400733; PMCID: PMC8976212.
12.
Gomez T, Anaya YB, Shih KJ, Tarn DM. A Qualitative Study of Primary Care Physicians’ Experiences With Telemedicine During COVID-19. J Am Board Fam Med. 2021 Feb;34(Suppl):S61-S70. doi:10.3122/jabfm.2021.S1.200517. PMID: 33622820.
13.
Verhoeven V, Tsakitzidis G, Philips H, Van Royen P. Impact of the COVID-19 pandemic on the core functions of primary care: will the cure be worse than the disease? A qualitative interview study in Flemish GPs. BMJ Open. 2020 Jun 17;10(6):e039674. doi:10.1136/bmjopen-2020-039674. PMID: 32554730; PMCID: PMC7306272.
14.
Haldane V, Zhang Z, Abbas RF, Dodd W, Lau LL, Kidd MR, Rouleau K, Zou G, Chao Z, Upshur REG, Walley J, Wei X. National primary care responses to COVID-19: a rapid review of the literature. BMJ Open. 2020 Dec 8;10(12):e041622. doi: 10.1136/bmjopen-2020-041622. PMID: 33293398; PMCID: PMC7725079.
15.
Gray R, Sanders C. A reflection on the impact of COVID-19 on primary care in the United Kingdom. J Interprof Care. 2020 Sep-Oct;34(5):672–678. doi: 10.1080/13561820.2020.1823948. Epub 2020 Sep 22. PMID: 32962462.
16.
Greenberg N, Docherty M, Gnanapragasam S, Wessely S. Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ. 2020 Mar; 26;368:m1211. doi:10.1136/bmj.m1211. PMID:32217624.
17.
Baird B, Reeve H, Ross S, Homeyman M, Nosa-Ehima M, Sahib B, Omojomolo D (2018). Innovative models of general practice. London: The King’s Fund. Available online: https://committees.parliament.... writtenevidence/41913/pdf/ (accessed on 14 September 2022).
18.
Anderson E, Sandars J, Kinnair D. The nature and benefits of teambased reflection on a patient death by healthcare professionals: a scoping review. J Interprof Care. 2019 Jan-Feb;33(1):15–25. doi: 10.1080/13561820.2018.1513462. Epub 2018 Sep 24. PMID: 30247946.
19.
World Health Organization. Strengthening in Primary Care: A Collection of Existing Standards, Measurement and Implementation Resources; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publicatio... item/9789240035249 (accessed on 14 July 2022).
20.
World Health Organization. Hand Hygiene. Technical Reference Manual; World Health Organization: Geneva, Switzerland, 2009; ISBN 9789241598606. Available online: http://apps.who.int/iris/bitst... handle/10665/44196/9789241598606_eng.pdf? sequence=1 (accessed on 14 July 2022).
21.
Phiri MM, MacPherson EE, Panulo M, Chidziwisano K, Kalua K, Chirambo CM, Kawalazira G, Gundah Z, Chunda P, Morse T. Preparedness for and impact of COVID-19 on primary health care delivery in urban and rural Malawi: a mixed methods study. BMJ Open. 2022 Jun 10;12(6):e051125
22.
Lai X, Wang X, Yang Q, Xu X, Tang Y, Liu C, Tan L, Lai R, Wang H, Zhang X, Zhou Q, Chen H. Will healthcare workers improve infection prevention and control behaviors as COVID-19 risk emerges and increases, in China? Antimicrob Resist Infect Control. 2020 Jun 11;9(1):83. doi:10.1186/s13756-020-00746-1. PMID: 32527300; PMCID: PMC7289224.
23.
Wong TW, Tam WW. Handwashing practice and the use of personal protective equipment among medical students after the SARS epidemic in Hong Kong. Am J Infect Control. 2005;33(10):580–6.
24.
Loh LC, Chelliah A, Ang TH, Ali A. Mohd. Change in infection control practices and awareness of hospital medical staff in the aftermath of SARS. Med J Malaysia. 2004;59(5):659–64.
25.
Eggleton K, Bui N, Goodyear-Smith F. COVID-19 impact on New Zealand general practice: rural-urban differences. Rural Remote Health. 2022 Feb;22(1):7185.
26.
Tham R, Humphreys J, Kinsman L, Buykx P, Asaid A, Tuohey K, Riley K. Evaluating the impact of sustainable comprehensive primary health care on rural health. Aust J Rural Health. 2010 Aug;18(4):166–72. doi: 10.1111/j.1440-1584.2010.01145.x. PMID: 20690913.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.