Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
The relationship between COPD Assessment Test (CAT) scores and Distress Thermometer (DT) results in COPD patients
1
Department of Pulmonology, Oncology and Allergology, Medical University, Lublin, Poland
2
Department of Applied Psychology, Chair of Psychology, Medical University, Lublin, Poland
3
Department of Internal Medicine, Medical University of Lublin, Poland
Corresponding author
Joanna Milanowska
Department of Applied Psychology, Medical University of Lublin, Chodzki 7, 20-093, Lublin, Poland
Department of Applied Psychology, Medical University of Lublin, Chodzki 7, 20-093, Lublin, Poland
Ann Agric Environ Med. 2020;27(4):689-694
KEYWORDS
TOPICS
Health effects of chemical pollutants in agricultural areas , including occupational and non-occupational effects of agricultural chemicals (pesticides, fertilizers) and effects of industrial disposal (heavy metals, sulphur, etc.) contaminating the atmosphere, soil and waterExposure to physical hazards associated with the use of machinery in agriculture and forestry: noise, vibration, dustPrevention of occupational diseases in agriculture, forestry, food industry and wood industry
ABSTRACT
Introduction:
Chronic Obstructive Pulmonary Disease (COPD) is a condition that affects over 2 million adults in Poland. In recent years, increasing attention has been focused on improving the quality of life of patients with COPD, which includes alleviating their physical discomfort and relates to their mental health. It is therefore critically important to evaluate research tools that can accurately assess the relationship between the physical and mental health of patients with this disease.
Objective:
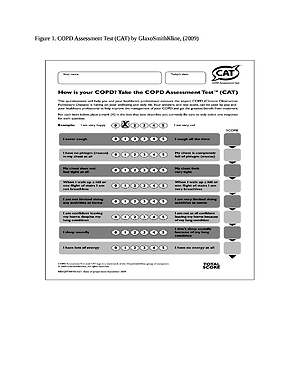
This aim of the study is to evaluate the relationship between the COPD Assessment Test (CAT) and the Distress Thermometer and Problem List results in COPD patients.
Material and methods:
The research evaluated 70 patients with COPD as defined by the Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD) criteria. Demographic data was obtained at baseline. Disease-specific quality of life was assessed using the CAT score, while overall distress was determined using the Distress Thermometer (DT) scale and a modified Problem List. The relationship between the CAT scores and the results of the Distress Thermometer and Problem List was statistically compared. The study was approved by the Bioethics Committee, and all patients provided written informed consent.
Results:
The mean ± SD age was 69.6±9.05 (range 47–90) years. The average distress level was 4.09±1.95. A significant relationship was established between the CAT score and the results of the Distress Thermometer Scale (p<0.001); patients with higher CAT scores showed the highest level of distress.
Conclusions:
CAT was shown to be a simple, fast and clear measurement of disease-specific quality of life and was correlated with levels of distress in patients with COPD. Every patient with COPD should be evaluated using a scale such as the DT to measure their level of psychological distress.
Chronic Obstructive Pulmonary Disease (COPD) is a condition that affects over 2 million adults in Poland. In recent years, increasing attention has been focused on improving the quality of life of patients with COPD, which includes alleviating their physical discomfort and relates to their mental health. It is therefore critically important to evaluate research tools that can accurately assess the relationship between the physical and mental health of patients with this disease.
Objective:
This aim of the study is to evaluate the relationship between the COPD Assessment Test (CAT) and the Distress Thermometer and Problem List results in COPD patients.
Material and methods:
The research evaluated 70 patients with COPD as defined by the Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD) criteria. Demographic data was obtained at baseline. Disease-specific quality of life was assessed using the CAT score, while overall distress was determined using the Distress Thermometer (DT) scale and a modified Problem List. The relationship between the CAT scores and the results of the Distress Thermometer and Problem List was statistically compared. The study was approved by the Bioethics Committee, and all patients provided written informed consent.
Results:
The mean ± SD age was 69.6±9.05 (range 47–90) years. The average distress level was 4.09±1.95. A significant relationship was established between the CAT score and the results of the Distress Thermometer Scale (p<0.001); patients with higher CAT scores showed the highest level of distress.
Conclusions:
CAT was shown to be a simple, fast and clear measurement of disease-specific quality of life and was correlated with levels of distress in patients with COPD. Every patient with COPD should be evaluated using a scale such as the DT to measure their level of psychological distress.
Makuch M, Milanowska J, Michnar M, Makuch M, Samardakiewicz M, Milanowski J. The relationship between COPD Assessment Test (CAT)
scores and Distress Thermometer (DT) results in COPD patients. Ann Agric Environ Med. 2020; 27(4): 689–694. doi: 10.26444/aaem/11410
REFERENCES (36)
1.
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis,management, and prevention of chronic obstructive pulmonarydisease. https://goldcopd.org/wp-conten... (access: 2018.11.13).
2.
Kim KU, Park HK, Jung HY, et al. Association of depression with disease severity inpatients with chronic obstructive pulmonary disease. Lung. 2014; 192: 243. doi:10.1007/s00408-013-9547-4.
3.
Montserrat-Capdevila J, Godoy P, Marsal JR, et al. Overview of the Impact ofDepression and Anxiety in Chronic Obstructive Pulmonary Disease. Lung 2017; 195: 77. doi: 10.1007/s00408-016-9966-0.
4.
Jones PW, Harding G, Berry P, et al. Development and first validation of the COPDAssessment Test. Eur Respir J. 2009; 34: 648. doi: 10.1183/09031936.00102509.
5.
NCCN practice guidelines for the management of psychosocial distress. National Comprehensive Cancer Network. Oncology (Williston Park). 1999 May; 13(5A): 113–47.
6.
Grassi L, Sabato S, Rossi E, et al. Affective syndromes and their screening in cancer patients with early and stable disease: Italian ICD-10 data and performance of the Distress Thermometer from the Southern European Psycho-Oncology Study (SEPOS). J Affect Disord. 2009; 114(1–3): 193–9.
7.
Śliwiński P, Górecka D, Jassem E, Pierzchała W. Polish Respiratory Society Guidelines for Chronic Obstructive Pulmonary Disease. Pneumonol Alergol Pol. 2014; 82; 3: 227–263.
8.
Meguro M, Barley EA, Spencer S, et al. Development and validation of an improved, COPD-specific version of the St. George Respiratory Questionnaire. Chest. 2007; 132: 456–463. doi:10.1378/chest.06-0702.
9.
Eisner MD, Blanc PD, Yelin EH, et al. Influence of anxiety on health outcomes in COPD. Thorax. 2010; 65(3): 229–34. doi: 10.1136/thx.2009.126201.
10.
Jones PW, Tabberer M, Chen WH. Creating scenarios of the impact of COPD and their relationship to COPD Assessment Test (CAT™) scores. BMC Pulm Med. 2011; 11: 42. doi: 10.1186/1471-2466-11-42.
12.
Życińska J, et al. Polska adaptacja skali DistressThermometer i Problem List. Badania walidacyjne wśród pacjentów onkologicznych. X Ogólnopolska Konferencja Psychoonkologiczna. 11—12 września 2009, Władysławowo. Abstrakt wystąpienia. Access mode: http://www.ptpo.org.pl/index/i... &id=151 (access: 2019.01.14).
13.
Gil F, Grassi L, Travado L, Tomamichel M, Gonzalez JR. Use of distress and depressionthermometers to measure psychosocial morbidity among southern European cancerpatients. Supportive Care In Cancer: Official Journal Of The Multinational Association Of Supportive Care In Cancer. 2005; 13: 600–606. doi: 10.1007/s00520-005-0780-0.
14.
Lynch J, Goodhart F, Saunders Y, O’Connor SJ. Screening for psychological distress inpatients with lung cancer: results of a clinical audit evaluating the use of the patientDistress Thermometer. Support Care Cancer. 2010; 19(2): 193–202. doi: 10.1007/s00520-014-2471-1.
15.
Holland JC, Bultz BD. National Comprehensive Cancer Network (NCCN). The NCCNguideline for distress management: a case for making distress the sixth vital sign. J Natl Compr Canc Netw. 2007; 5: 3–7.
16.
Omachi TA, Katz PP, Yelin EH, Gregorich SE, Iribarren C, Blanc PD, et al. Depressionand health-related quality of life in chronic obstructive pulmonary disease. Am JMed. 2009; 122(8): 778 e9–15. doi: 10.1016/j.amjmed.2009.01.036.
17.
The NCCN. Distress Management (Version 1.2008) National Comprehensive Cancer Network, Inc. 2007. http://www.nccn.org (access: 2019.01.14).
18.
Hill K, Geist R, Goldstein RS, Lacasse Y. Anxiety and depression in end-stageCOPD. EurRespir J. 2008; 31(3): 667–77. doi: 10.1183/09031936.00125707.
19.
Kim KU, Park HK, Jung HY, et al. Association of depression with disease severity inpatients with chronic obstructive pulmonary disease. Lung 2014; 192: 243.
20.
Ghobadi H, Ahari SS, Kameli A, Lari SM. The Relationship between COPD AssessmentTest (CAT) Scores and Severity of Airflow Obstruction in Stable COPD Patients, Tanaffos. 2012; 11(2): 22–26.
21.
Shim EJ, Shin YW, Jeon HJ, Hahm BJ. Distress and its correlates in Koreancancer patients: pilot use of the distress thermometer and the problem list. Psycho-Oncology 2008; 17(6): 548–555. doi: 10.1002/pon.1275.
22.
Clover K, Carter G, Mackinnon A, Adams C. Is my patient suffering clinicallysignificant emotional distress? Demonstration of a probabilities approach to evaluatingalgorithms for screening for distress. Support Care Cancer. 2009; 17: 1455–1462. doi:10.1007/s00520-009-0606-6.
23.
Lim HA, Mahendran R, Chua J, et al. The Distress Thermometer as an ultra-short screening tool: a first validation study for mixed-cancer outpatients in Singapore. Compr Psychiatry 2014; 55: 1055.
24.
Panagioti M, Charlotte Scott C, Blakemore A, Coventry P. Overview of the prevalence,impact, and management of depression and anxiety in chronic obstructive pulmonarydisease. Int J Chron Obstruct Pulmon Dis. 2014; 9: 1289–1306. doi:10.2147/COPD.S72073.
25.
Eisner M, Blanc P, Yelin E, Katz P, Sanchez G, Iribarren C, Omachi T. The influence of anxiety on health outcomes in COPD. Thorax. 2010 Mar; 65(3): 229–234. doi:10.1136/thx.2009.126201.
26.
Jing L, Guangju M, Yi M, Xia Z, Dongmei C, Mengting C. Influence of COPD Assessment Text (CAT) evaluation and rehabilitation education guidance on therespiratory and motor functions of COPD patients, Open Med (Wars). 2015; 10(1): 394–398.
27.
Iskandarsyah A, Klerk C, Suardi D, Soemitro M, Sadarjoen S. The Distress Thermometerand Its Validity: A First Psychometric Study in Indonesian Women with Breast Cancer. PLoS One. 2013; 8(2): e56353. doi: 10.1371/journal.pone.0056353.
28.
Hughes K, Sargeant H, Hawkes A. Acceptability of the Distress Thermometer andProblem List to community-based telephone cancer helpline operators, and to cancerpatients and carers.BMC Cancer. 2011; 11: 46. doi: 10.1186/1471-2407-11-46.
29.
Ryan H, Schofield P, Cockburn J, et.al. How to recognize and manage psychologicaldistress in cancer patients. Eur J Cancer Care (Engl). 2005 Mar; 14(1): 7–15. doi:10.1111/j.1365-2354.2005.00482.x.
30.
Donovan KA, Grassi L, McGinty HL, Jacobsen PB. Validation of the distress thermometer worldwide: state of the science. Psychooncology 2014; 23: 241.
31.
Chiou YJ, Lee CY, Li SH, et al. Screening for Psychologic Distress in Taiwanese Cancer Inpatients Using the National Comprehensive Cancer Network Distress Thermometer: The Effects of Patients’ Sex and Chemotherapy Experience. Psychosomatics 2017; 58: 496.
32.
Bidstrup PE, Mertz BG, Dalton SO, et al. Accuracy of the Danish version of the ‘distress thermometer’. Psychooncology 2012; 21: 436.
33.
Tang LL, Zhang YN, Pang Y, et al. Validation and reliability of distress thermometer in chinese cancer patients. Chin J Cancer Res. 2011; 23: 54.
34.
Chambers SK, Zajdlewicz L, Youlden DR, et al. The validity of the distress thermometer in prostate cancer populations. Psychooncology 2014; 23: 195.
35.
San Giorgi MR, Aaltonen LM, Rihkanen H, et al. Validation of the Distress Thermometer and Problem List in Patients with Recurrent Respiratory Papillomatosis. Otolaryngol Head Neck Surg. 2017; 156: 180.
36.
Ma X, Zhang J, Zhong W, et al. The diagnostic role of a short screening tool--the distress thermometer: a meta-analysis. Support Care Cancer 2014; 22: 1741.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.