Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
The prevalence and significance of anti-PM/Scl antibodies in systemic sclerosis
1
Department of Rheumatology and Connective Tissue Diseases, Medical University, Lublin, Poland
Corresponding author
Ewa Wielosz
Department of Rheumatology and Connective Tissue Diseases, Medical University of Lublin, Jaczewskiego 8, 20-090, Lublin, Poland
Department of Rheumatology and Connective Tissue Diseases, Medical University of Lublin, Jaczewskiego 8, 20-090, Lublin, Poland
Ann Agric Environ Med. 2021;28(1):189-192
KEYWORDS
TOPICS
- Biological agents posing occupational risk in agriculture, forestry, food industry and wood industry and diseases caused by these agents (zoonoses, allergic and immunotoxic diseases)
- State of the health of rural communities depending on various factors: social factors, accessibility of medical care, etc.
ABSTRACT
Introduction:
Anti-PM/Scl (a-PM/Scl) antibodies are found in different systemic autoimmune diseases such as polymyositis, dermatomyositis, systemic sclerosis (SSc) and overlap syndromes. According to literature, they are detected in approx. 2% of SSc patients, but their presence is more common in SSc with myositis overlap.
Objective:
The aim of the study was to assess the prevalence of a-PM/Scl in patients with SSc and to identify differences in the clinical profile of the disease in patients with the presence of a-PM/Scl.
Material and methods:
The study was performed on 126 European Caucasian SSc patients (98 females and 28 males) hospitalized consecutively in the Department of Rheumatology and Connective Tissue Diseases. The study group was analyzed for the potential presence of a-PM/Scl using a commercial test – EUROLINE Systemic Sclerosis Profile. The detection and interpretation were carried out electronically using the specific Euroimmun – EUROLineScan programme. The subtype of SSc, incidence of internal organ involvement and serological profile were determined in the entire group. Due to the presence of a-PM/Scl, patients were divided into two groups: a-PM/Scl (+) SSc – 22 patients and a-PM/Scl (-) SSc – 104 patients.
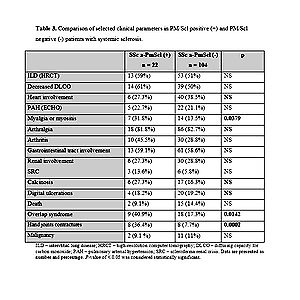
Results:
A-PM/Scl was detected in 22/126 patients with SSc (17.5%). A strong correlation was found between a-PM/Scl and myalgia or myositis (p = 0.0379), hand joints contractures (p = 0.0002) and the prevalence of overlap syndrome (p = 0.0142). There were no relationships between the presence of a-PM/Scl and subtypes of SSc, other organ involvement, digital ulcers or calcinosis.
Conclusions:
Anti-PM/Scl antibodies are fairly common in patients with systemic sclerosis. In SSc, anti-PM/Scl antibodies are frequently associated with myalgia or myositis, hand joint contractures and an overlap syndrome.
Anti-PM/Scl (a-PM/Scl) antibodies are found in different systemic autoimmune diseases such as polymyositis, dermatomyositis, systemic sclerosis (SSc) and overlap syndromes. According to literature, they are detected in approx. 2% of SSc patients, but their presence is more common in SSc with myositis overlap.
Objective:
The aim of the study was to assess the prevalence of a-PM/Scl in patients with SSc and to identify differences in the clinical profile of the disease in patients with the presence of a-PM/Scl.
Material and methods:
The study was performed on 126 European Caucasian SSc patients (98 females and 28 males) hospitalized consecutively in the Department of Rheumatology and Connective Tissue Diseases. The study group was analyzed for the potential presence of a-PM/Scl using a commercial test – EUROLINE Systemic Sclerosis Profile. The detection and interpretation were carried out electronically using the specific Euroimmun – EUROLineScan programme. The subtype of SSc, incidence of internal organ involvement and serological profile were determined in the entire group. Due to the presence of a-PM/Scl, patients were divided into two groups: a-PM/Scl (+) SSc – 22 patients and a-PM/Scl (-) SSc – 104 patients.
Results:
A-PM/Scl was detected in 22/126 patients with SSc (17.5%). A strong correlation was found between a-PM/Scl and myalgia or myositis (p = 0.0379), hand joints contractures (p = 0.0002) and the prevalence of overlap syndrome (p = 0.0142). There were no relationships between the presence of a-PM/Scl and subtypes of SSc, other organ involvement, digital ulcers or calcinosis.
Conclusions:
Anti-PM/Scl antibodies are fairly common in patients with systemic sclerosis. In SSc, anti-PM/Scl antibodies are frequently associated with myalgia or myositis, hand joint contractures and an overlap syndrome.
REFERENCES (21)
1.
Boonstra M, Mertens BJA, Bakker JA, et al. To what extent do autoantibodies help to identify high-risk patients in systemic sclerosis? Clin Exp Rheumatol. 2018; 36: 109–117.
2.
Hamaguchi Y. Autoantibody profiles in systemic sclerosis: predictive value for clinical evaluation and prognosis. J Dermatol. 2010; 37: 42–53.
3.
Shanmugam VK, Frech TM, Steen VD, et al. Collaborative National Quality and Efficacy Registry (CONQUER) for Scleroderma: outcomes from a multicenter US-based systemic sclerosis registry. Clin Rheumatol. 2020; 39: 93–102.
4.
van den Hoogen F, Khanna D, Fransen J, et al. 2013 classification criteria for systemic sclerosis: an American college of rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis. 2013; 72: 1747–1755.
5.
Liaskos C, Marou E, Simopoulou T, et al. Disease-related autoantibody profile in patients with systemic sclerosis. Autoimmunity. 2017; 50: 414–421.
6.
Margot A, Smet J, Soyfoo S. Non-identified antinuclear antibodies in systemic sclerosis. Rev Med Brux. 2016; 37: 401–407.
7.
Wielosz E, Dryglewska M, Majdan M. Serological profile of patients with systemic sclerosis. Postępy Hig Med Dosw. 2014; 18; 68: 987–991.
8.
LeRoy EC, Black C, Fleishmajer R. Scleroderma (systemic sclerosis): classification, subsets and pathogenesis. J Rheumatol. 1988; 15: 202–204.
9.
Jaskowski TD, Wilson A, Hill HR, Tebo AE. Diagnostic assays for anti-PM/Scl IgG antibodies: heterogeneity in antibody response or lack of standardization? Clin Chim Acta. 2011; 12: 1100–1105.
10.
Kohara A, Yanaba K, Muro Y, et al. Anti-PM/Scl antibody-positive dermatomyositis in a Japanese patient: a case report and review of the literature. Int J Rheum Dis. 2017; 20: 2186–2189.
11.
Wodkowski M, Hudson M, Proudman S, et al. Clinical correlates of monospecific anti-PM75 and anti-PM100 antibodies in a tri-nation cohort of 1574 systemic sclerosis subjects. Autoimmunity. 2015; 48: 542–551.
12.
Stochmal A, Czuwara J, Trojanowska M, Rudnicka L. Antinuclear Antibodies in Systemic Sclerosis: an Update. Clin Rev Allergy Immunol. 2020; 58: 40–51.
13.
D’Aoust J, Hudson M, Tatibouet S, Wick J, et al. Clinical and serologic correlates of anti-PM/Scl antibodies in systemic sclerosis: a multicenter study of 763 patients. Arthritis Rheumatol. 2014; 66: 1608–1615.
14.
Mahler M, Greidinger EL, Szmyrka M, et al. Serological and clinical characterization of anti-dsDNA and anti-PM/Scl double-positive patients. Ann N Y Acad Sci. 2007; 1109: 311–321.
15.
Guillen-Del Castillo A, Pilar Simeón-Aznar C, et al. Good outcome of interstitial lung disease in patients with scleroderma associated to anti-PM/Scl antibody. Semin Arthritis Rheum. 2014; 44: 331–337.
16.
Valenzuela A, Song P, Chung L. Calcinosis in scleroderma. Curr Opin Rheumatol. 2018; 30: 554–561.
17.
Bernal-Bello D, de Tena JG, Guillén-Del Castillo A, et al. Novel risk factors related to cancer in scleroderma. Autoimmun Rev. 2017; 16: 461–468.
18.
Bruni.C, Lages A, Patel H, et al. Association of a-PM/Scl antibody with risk of malignancy in scleroderma. Rheumatol. 2015; 54: i60.
19.
Muro Y, Hosono Y, Sugiura K, et al. Anti-PM/Scl antibodies are found in Japanese patients with various systemic autoimmune conditions besides myositis and scleroderma. Arthritis Res Ther. 2015; 11: 17:57.
20.
Sada PR1, García LP, Rodrigo ME. Clinical heterogeneity of anti-PM/Scl positive conditions. Br J Hosp Med (Lond). 2018; 79: 532–533.
21.
Boonstra M, Huizinga TWJ. De Vries-Bouwstra JK. Auto-antibodies and cancer in systemic sclerosis. Autoimmun Rev. 2017; 16: 883–884.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.