Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
The COVID-19 pandemic and epidemiology of the most common cancers in the Subcarpathian and Silesian Provinces of Poland
1
Department of Statistics, Medical Univeristy of Silesia, Katowice, Poland
2
Department of Nursing and Public Health, College of Medical Sciences, University of Rzeszów, Poland
3
Clinical Department of Internal Medicine and Oncological Chemotherapy, Faculty of Medical Sciences in Katowice,
Medical University of Silesia, Katowice, Poland
4
Health Promotion and Obesity Management Unit, Department of Pathophysiology, Faculty of Medical Sciences in Katowice, the Medical University of Silesia, Katowice, Poland
Corresponding author
Piotr Stanisław Choręza
Department of Statistics, Medical Univeristy of Silesia in Katowice, Ostrogórska Street 30, 41-200, Sosnowiec, Poland
Department of Statistics, Medical Univeristy of Silesia in Katowice, Ostrogórska Street 30, 41-200, Sosnowiec, Poland
Ann Agric Environ Med. 2023;30(1):90-104
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The study aimed to assess the effect of the COVID-19 pandemic and slow cancer burden on the healthcare system of the most frequent cancers in the Subcarpathien and Silesian Provinces of southern Poland in the period 2015–2020.
Material and methods:
Depersonalized, epidemiological data were obtained from the branches of the National Health Founf of Poland (NFZ) in the Subcarpathian and Silesian Province. The database contained 7,814,870 healthcare services granted to 385,845 patients with disease entities classified as C00–C97, according to the ICD-10.
Results:
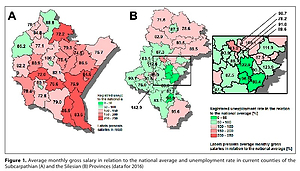
In the period 2015–2020, cancer diseases were diagnosed in 3,445 per 100,000 citizens of the Subcarpathian Province and 5248 per 100,000 citizens of the Silesian Province. The changes in SMR values due to cancer diseases found in the Subcarpathian Province were characterized by temporal and spatial differentiation. In the period 2016–2019, unencumbered by the COVID-19 pandemic, the SMR values had decreased on average by -13.2% in most counties of the Subcarpathian Province, but in 2020 the SMR values decreased by -14.7% compared to 2019. In the Silesian Province, similar to the Subcarpathian Province, the values of SMR decreased in the period 2016–2019 in all counties (with the exception of the town of Piekary Śląskie), on average, by -11.5%. Subsequently, in 2020, a significant reduction of SMR compared to 2019 was observed on average by -7.9%.
Conclusions:
In 2020, a significant reduction in the diagnosis of patients with cancer was found in the one-year perspective study in both Provinces, which suggests the limitation of availability of the specialistic oncologic healthcare services due to the fight against the COVID-19 pandemic. An increased burden of cancers shortly should be expected. Thus, regional and nationwide screening programmes should be introduced to enable diagnosis at the earliest possible stage.
The study aimed to assess the effect of the COVID-19 pandemic and slow cancer burden on the healthcare system of the most frequent cancers in the Subcarpathien and Silesian Provinces of southern Poland in the period 2015–2020.
Material and methods:
Depersonalized, epidemiological data were obtained from the branches of the National Health Founf of Poland (NFZ) in the Subcarpathian and Silesian Province. The database contained 7,814,870 healthcare services granted to 385,845 patients with disease entities classified as C00–C97, according to the ICD-10.
Results:
In the period 2015–2020, cancer diseases were diagnosed in 3,445 per 100,000 citizens of the Subcarpathian Province and 5248 per 100,000 citizens of the Silesian Province. The changes in SMR values due to cancer diseases found in the Subcarpathian Province were characterized by temporal and spatial differentiation. In the period 2016–2019, unencumbered by the COVID-19 pandemic, the SMR values had decreased on average by -13.2% in most counties of the Subcarpathian Province, but in 2020 the SMR values decreased by -14.7% compared to 2019. In the Silesian Province, similar to the Subcarpathian Province, the values of SMR decreased in the period 2016–2019 in all counties (with the exception of the town of Piekary Śląskie), on average, by -11.5%. Subsequently, in 2020, a significant reduction of SMR compared to 2019 was observed on average by -7.9%.
Conclusions:
In 2020, a significant reduction in the diagnosis of patients with cancer was found in the one-year perspective study in both Provinces, which suggests the limitation of availability of the specialistic oncologic healthcare services due to the fight against the COVID-19 pandemic. An increased burden of cancers shortly should be expected. Thus, regional and nationwide screening programmes should be introduced to enable diagnosis at the earliest possible stage.
ACKNOWLEDGEMENTS
The authors thank the Managements of the Podkarpackie and Silesian Voivodeship Branches of the National Health Fund of Poland and Mr. Tomasz Brud from the Podkarpackie Voivodeship Branch of NFZ and Mr. Damian Grund and Mr. Jacek Kielesz from the Silesian Voivodeship Branch of NFZ for data prociding.
The authors thank the Mrs. Elżbieta Chełmecka PhD, Head of the Department os Statistics for the help in data obtaining.
The project was funded by the Medical University of Silesia grants no. PCN-1-103/N/1/F and PCN-1-068/N/2/Z
REFERENCES (43)
1.
Arnold M, Karim-Kos HE, Coebergh JW, et al. Recent trends in incidence of five common cancers in 26 European countries since 1988: Analysis of the European Cancer Observatory. Eur J Cancer. 2015; 51(9): 1164–1187. doi: 10.1016/j.ejca.2013.09.002.
2.
Demko P. Health care spending again accelerating. Politico https://www.politico.com/story... (access: 30.03.2022).
3.
Bradley CJ. Economic burden associated with cancer caregiving. Semin Oncol Nurs. 2019; 35(4): 333–336.
4.
Dyba T, Randi G, Bray F, et al. The European cancer burden in 2020: incidence and mortality estimates for 40 countries and 25 major cancers. Eur J Cancer. 2021; 157: 308–347. doi: 10.1016/j.ejca.2021.07.039.
5.
Tweed Ej, Allardice GM, McLoone P, Morrison DS. Socio-economic inequalities in the incidence of four common cancers: a population-based registry study. Public Health. 2018; 154: 1–10. doi: 10.1016/j.puhe.2017.10.005.
6.
Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382: 727–733. doi: 10.1056/NEJMoa2001017.
7.
Didler MM, Bray F. Global cancer inequalities. Front Oncol. 2018; 8: 293. doi: 10.3389/fonc.2018.00293.
8.
Xie Q, Shi L, He X, Luo Y. Gastrointestinal cancers in China, the USA and Europe. Gastroenterol Rep. 2021; 9(2): 91–104. doi: 10.1093/gastro/goab010.
9.
Wild CP, Espina C, Bauld L, et al. Cancer Prevention Europe. Mol Oncol. 2019; 13(3): 528–534. doi: 10.1002/1878-0261.12455.
11.
Kobza J, Geremek M, Dul L. Characteristics of air quality and sources affecting high levels of PM 10 and PM 2.5 in Poland, Upper Silesia urban area. Environ Monit Assess. 2018; 190(9):515. doi: 10.1007/s10661-018-6797-x.
12.
Dziubanek G, Spychała A, Marchwińska-Wyrwał E, et al. Long-term exposure to urban air pollution and the relationship with life expectancy in cohort of 3.5 million people in Silesia. Sci Total Environ. 2017; 580: 1–8. doi: 10.1016/j.scitotenv.2016.11.217.
13.
Huang Y, Zhu M, Ji M, et al. Air Pollution, Genetic Factors, and the Risk of Lung Cancer: A Prospective Study in the UK Biobank. Am J Respir Crit Care Med. 2021; 204(7): 817–825. doi: 10.1164/rccm.202011-4063OC.
14.
Turner MC, Anderson ZJ, Baccarelli A, et al. Outdoor Air Pollution and Cancer: An Overview of the Current Evidence and Public Health Recommendations. CA Cancer J Clin. 2020; 10.3322/caac.21632. doi: 10.3322/caac.21632.
15.
Augustynowicz A, Czerw A, Borowska M, Fronczak A, Deptała A. Breast cancer and cervical cancer prevention programmes carried out by local government units in Poland in 2009–2014. Oncotarget. 2018; 9(31): 21943–21949. doi: 10.18632/oncotarget.24513.
16.
Chakalova G, Dimitrova N, Gavrilov I, Valerianova Z. Cancer burden of breast and gynaecological cancers in Bulgaria: epidemiology and clinical aspects. JBUN 2013; 18(4): 1038–1044.
17.
Lundqvist A, Andersson E, Ahlberg I, Nilbert M, Gerdtham U. Socioeconomic inequalities in breast cancer incidence and mortality in Europe – a systematic review and meta-analysis. Eur J Public Health. 2016; 26(5): 804–813. doi: 10.1093/eurpub/ckw070.
18.
Ginsburg O, Bray F, Coleman MP, et al. The global burden of women’s cancers: an unmet grand challenge in global health. Lancet. 2017; 389(10071): 847–860. doi: 10.1016/S0140-6736(16)31392-7.
19.
Walsh PM, Byrne J, Kelly M, McDevitt J, Comber H. Socioeconomic disparity in survival after breast cancer in Ireland: observational study. PLoS One. 2014; 9(11): e111729 doi: 10.1371/journal.pone.0111729.
20.
Wojtyla C, Bertuccio P, Wojtyla A, La Vecchia C. European trends in breast cancer mortality, 1980–2017 and predictions to 2025. Eur J Cancer. 2021; 152: 4–17. doi: 10.1016/j.ejca.2021.04.026.
22.
GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016; 388:1459–1544. doi: 10.1016/S0140-6736(16)31012-1.
23.
Paciej-Gołębiowska P, Pikala M, Maniecka-Bryła I. Years of life lost due to malignant neoplasms of the digestive system in Poland during 10 years of socioeconomic transformation. Eur J Cancer Prev. 2020; 29(5): 388–399. doi: 10.1097/CEJ.0000000000000574.
24.
Drygas W, Bielecki W, Kozakiewicz K, et. al. Wieloośrodkowe Ogólnopolskie Badanie Stanu Zdrowia Ludności – WOBASZ. In: Kopeć G, Jankowski P, Pająk A, Drygas W, editors. Epidemiologia i prewencja chorób krążenia. Kraków; 2015. p. 41–55.
25.
Wojciechowska U, Czaderny K, Ciuba A, Olasek P, Didkowska J. Cancer in Poland in2016. Warsaw: Polish National Cancer Registry; 2018.
26.
Didkowska J, Wojciechowska U, Olasek P, Caentano dos Santos F, Michałek I. Cancer in Poland in 2019. Warsaw: Polish National Cancer Registry; 2021.
27.
Kaczmarek T, Marcinkowski J, Szozda R, Ziemska B, Wiśniewska-Śliwińska H. The quality of the medical records seen from the perspective of needs of the Institution of Social Securities. Orzecznictwo Lek. 2010; 7(1):66–73. [Polish].
28.
Clynch N, Kellett J. Medical documentation: Part of the solution, or part of the problem? A narrative review of the literature on the time spent on and value of medical documentation. Int J Med Inform. 2015; 84(4): 221–8. doi: 10.1016/j.ijmedinf.2014.12.001.
29.
Supreme Audit Office of Poland. Report: Tworzenie i udostępnianie dokumentacji medycznej. Warsaw; 2016. [Polish].
30.
Marmot M, Bell R. Social inequalities in health: a proper concern of epidemiology. Ann Epidemiol. 2016; 26(4): 238–240. doi: 10.1016/j.annepidem.2016.02.003.
31.
Onesti CE, Rugo HS, Generali D, et al. Oncological care organisation during COVID-19 outbreak. ESMO Open. 2020; 5(4): e000853. doi: 10.1136/esmoopen-2020-000853.
32.
Czarkowski M, Staszwska-Jakubik E, Wielgosz U. Infectious diseases and poisonings in Poland in 2020. National Institute of Public Health NIH – National Research Institute & Chief Sanitary; 2021.
33.
Ministry of Health of the Republic of Poland. Response to the Authors’ request for public information of September 8, 2022 (sign: ASP.0164.215.2022.AK).
34.
Bank Danych Lokalnych/ Local Data Bank. URL: https://bdl.stat.gov.pl/BDL/st... (access: 09.09.2022).
35.
Maluchnik M, Podwójcic K, Więckowska B. Decreasing access to cancer diagnosis and treatment during the COVID-19 pandemic in Poland. Acta Oncol. 2021; 60(1): 28–31. doi: 10.1080/0284186X.2020.1837392.
36.
Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. 2020; 74(11): 964–968. doi: 10.1136/jech-2020-214401.
37.
Brunetti O, Derakhshani A, Baradaran B, et al. COVID-19 Infection in Cancer Patients: How Can Oncologists Deal With These Patients. Front Oncol. 2020; 10: 734. doi: 10.3389/fonc.2020.00734.
38.
Shirke MM, Shaikh SA, Harky A. Implications of Telemedicine in Oncology during the COVID-19 Pandemic. Acta Biomed. 2020; 91(3): e2020022. doi: 10.23750/abm.v91i3.9849.
39.
Bardet A, Fraslin AM, Marghadi J, et al. Impact of COVID-19 on healthcare organisation and cancer outcomes. Eur J Cancer. 2021; 153:123–132. doi: 10.1016/j.ejca.2021.05.012.
40.
Smolić Š, Čipin I, Međimurec P. Access to healthcare for people aged 50+ in Europe during the COVID-19 outbreak. Eur J Ageing. 2021; 1–17. doi: 10.1007/s10433-021-00631-9.
41.
World Health Organisation (WHO). Pulse survey on continuity of essential health services during the COVID-19 pandemic: interim report, 27 August 2020. World Health Organization. https://apps.who.int/iris/hand....
42.
Ledford L, Lockwood S. Scope and epidemiology of gynecologic cancers: an overview. Scope and Epidemiology of Gynecologic Cancers: An Overview. Semin Oncol Nurs. 2019; 35(2): 147–150. doi: 10.1016/j.soncn.2019.03.002.
43.
Núnez A, Sreeganga SD, Ramaprasad A. Access to healthcare during COVID-19. Int J Environ Res Public Health. 2021; 18(6): 2980. doi: 10.3390/ijerph18062980.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.