Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Temperature as a determining factor in the occurrence of Legionella sp. bacteria in hot water systems in hospitals and social welfare homes
1
Collegium Medicum, Jan Kochanowski University, Kielce, Poland
2
Collegium Medicum, Medical Academy of Applied and Holistic Sciences, Warsaw, Poland
3
Department of Medical Anthropology, Institute of Rural Health, Lublin, Poland
4
Internal Medicine Department, St. Alexander Hospital, Kielce, Poland
Corresponding author
Piotr Choina
Department of Medical Anthropology, Institute of Rural Health, Lublin, Poland, ul. Jaczewskiego 2, 20-090, Lublin, Poland
Department of Medical Anthropology, Institute of Rural Health, Lublin, Poland, ul. Jaczewskiego 2, 20-090, Lublin, Poland
Ann Agric Environ Med. 2024;31(4):485-491
KEYWORDS
TOPICS
- Biological agents posing occupational risk in agriculture, forestry, food industry and wood industry and diseases caused by these agents (zoonoses, allergic and immunotoxic diseases)
- State of the health of rural communities depending on various factors: social factors, accessibility of medical care, etc.
ABSTRACT
Introduction and objective:
Water in installations in hospitals and social welfare homes (SWHs) should meet the requirements of the Directive of the European Parliament and of the Council on the quality of water intended for human consumption and national regulations issued on its basis. At present, 60 species of bacteria of the genus Legionella sp. are known (of which 30 are considered as pathogenic for humans), and more than 80 serologic groups. The aim of the study was determination of the effect of temperature on contamination of hot water systems with Legionella sp. bacteria in buildings of hospitals and SWHs in the Kielce Province, Poland, based on measurement of the temperature of domestic hot water during the period 2014–2018.
Material and methods:
631 results of temperature measurements and examinations of the quality of hot water were analyzed for the presence of the occurrence of Legionella sp. bacteria, conducted in 30 buildings of hospitals and 32 buildings of social welfare homes.
Results:
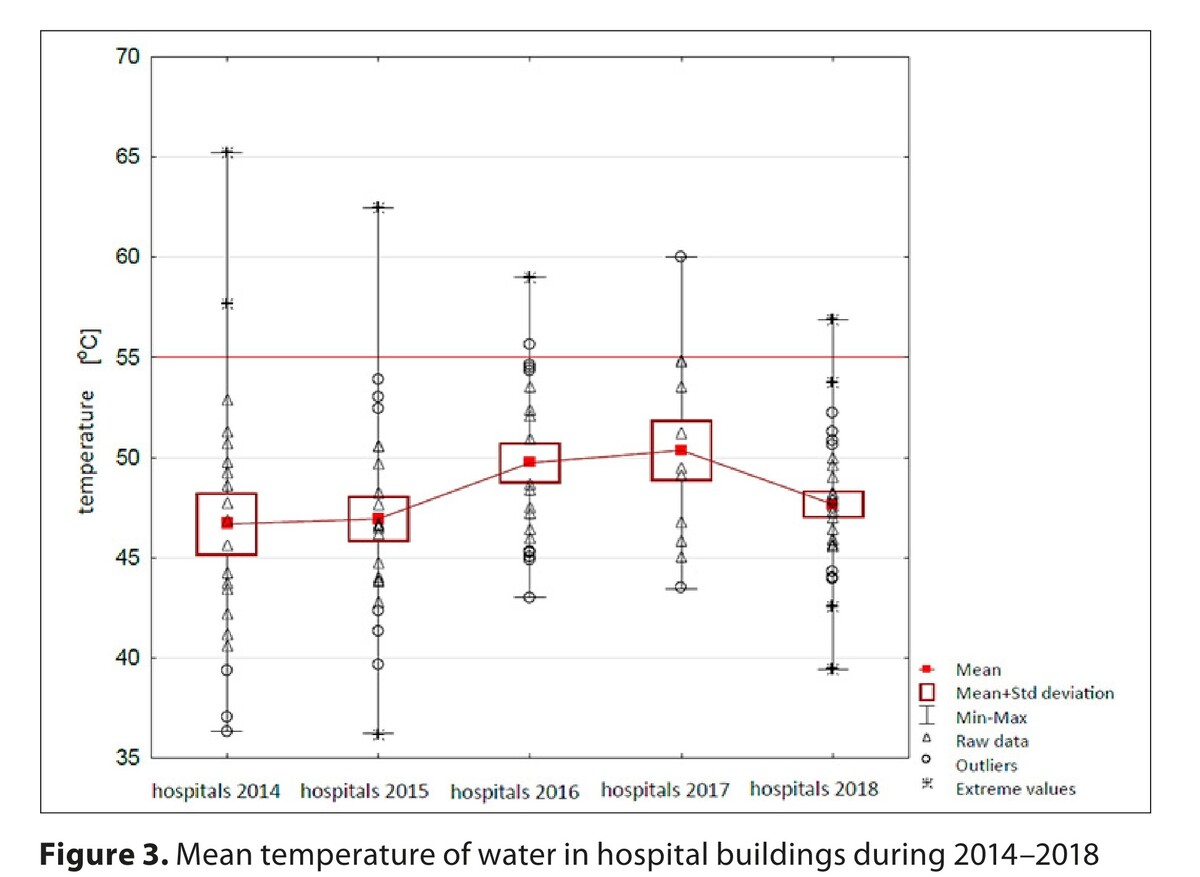
From among 581 samples, only 8.95% (n=52) had a temperature of ≥55°C. The mean temperature of water in the installations of buildings, calculated based on measurements carried out while collecting samples for the study, was 46°C in 2014, and up to 47°C in 2018. The allowable limit of bacteria was exceeded in 13.04% (n=69) of the samples at the temperature < 55°C, and in 3.85% (n=2) of the samples in which the temperature was higher or equal to 55°C.
Conclusions:
Water temperature ≥55°C significantly reduced the occurrence of excessive contamination of samples with Legionella sp. bacteria. Proper temperature of domestic water in water systems in hospitals and SWHs is indispensable for the provision of health safety of the patients.
Water in installations in hospitals and social welfare homes (SWHs) should meet the requirements of the Directive of the European Parliament and of the Council on the quality of water intended for human consumption and national regulations issued on its basis. At present, 60 species of bacteria of the genus Legionella sp. are known (of which 30 are considered as pathogenic for humans), and more than 80 serologic groups. The aim of the study was determination of the effect of temperature on contamination of hot water systems with Legionella sp. bacteria in buildings of hospitals and SWHs in the Kielce Province, Poland, based on measurement of the temperature of domestic hot water during the period 2014–2018.
Material and methods:
631 results of temperature measurements and examinations of the quality of hot water were analyzed for the presence of the occurrence of Legionella sp. bacteria, conducted in 30 buildings of hospitals and 32 buildings of social welfare homes.
Results:
From among 581 samples, only 8.95% (n=52) had a temperature of ≥55°C. The mean temperature of water in the installations of buildings, calculated based on measurements carried out while collecting samples for the study, was 46°C in 2014, and up to 47°C in 2018. The allowable limit of bacteria was exceeded in 13.04% (n=69) of the samples at the temperature < 55°C, and in 3.85% (n=2) of the samples in which the temperature was higher or equal to 55°C.
Conclusions:
Water temperature ≥55°C significantly reduced the occurrence of excessive contamination of samples with Legionella sp. bacteria. Proper temperature of domestic water in water systems in hospitals and SWHs is indispensable for the provision of health safety of the patients.
REFERENCES (29)
2.
Zhu Y, Liu D. Legionella. Molecular Medical Microbiol. 2024:1547–1557. doi:10.1016/B978-0-12-818619-0.00071-X.
3.
Szczepanek A, Tyszko P, Kalinowski P, Chmielewski J, Choina P, Nowak-Starz G. Occurrence of Legionella sp. bacteria in hot water systems in hospitals and nursing homes in the Świętokrzyskie Province of south-eastern Poland. Ann Agric Environ Med. 2023;30(4):654–660. doi:10.26444/aaem/176501.
4.
Stojek NM, Dutkiewicz J. Legionella and other Gram-negative bacteria in potable water from various rural and urban sources. Ann Agric Environ Med. 2006;13:323–335.
5.
Stojek NM, Szymańska J, Dutkiewicz J. Gram-negative bacteria in water distribution systems of hospitals. Ann Agric Environ Med. 2008;15:135–142.
6.
Yang JL, Li D, Zhan XY. Concept about the Virulence Factor of Legionella. Microorganisms. 2022;11(1):74. Published 2022 Dec 27. doi:10.3390/microorganisms11010074.
7.
European Centre for Disease Prevention and Control. Legionnaires’ disease. In: ECDC. Annual Epidemiological Report for 2021. Stockholm: ECDC; 2023.
10.
Rakić A, Perić J, Foglar L. Influence of temperature, chlorine residual and heavy metals on the presence of Legionella pneumophila in hot water distribution systems. Ann Agric Environ Med. 2012;19(3):431–436.
11.
Hochstrasser R, Hilbi H. The Legionella Lqs-LvbR Regulatory Network Controls Temperature-Dependent Growth Onset and Bacterial Cell Density. Appl Environ Microbiol. 2022;88(5):e0237021. doi:10.1128/aem.02370-21.
12.
Quero S, Párraga-Niño N, Garcia-Núñez M, et al. The impact of pipeline changes and temperature increase in a hospital historically colonised with Legionella. Sci Rep. 2021;11(1):1916. Published 2021 Jan 21. doi:10.1038/s41598-021-81625-6.
13.
Girolamini L, Salaris S, Pascale MR, et al. Dynamics of Legionella Community Interactions in Response to Temperature and Disinfection Treatment: 7 Years of Investigation. Microb Ecol. 2022;83:353–362. https://doi.org/10.1007/s00248....
14.
Carlson KM, Boczek LA, Chae S, Ryu H. Legionellosis and Recent Advances in Technologies for Legionella Control in Premise Plumbing Systems: A Review. Water (Basel). 2020;12(3):1–676. doi:10.3390/w12030676.
15.
European Technical Guidelines for the Prevention, Control and Investigation, of Infections Caused by Legionella Species. ECDC 2017.
16.
Matuszewska R, Stankiewicz A. Metody dezynfekcji stosowane do usuwania zanieczyszczenia pałeczkami Legionella z instalacji wodociągowych w zakładach opieki zdrowotnej. Hygeia Public Health 2017;52(3):226–233.
17.
Girolamini L, Dormi A, Pellati T, et al. Advances in Legionella Control by a New Formulation of Hydrogen Peroxide and Silver Salts in a Hospital Hot Water Network. Pathogens. 2019;8(4):209. Published 2019 Oct 29. doi:10.3390/pathogens8040209.
18.
Ji P, Rhoads WJ, Edwards MA, Pruden A. Effect of heat shock on hot water plumbing microbiota and Legionella pneumophila control. Microbiome. 2018;6(1):30. Published 2018 Feb 9. doi:10.1186/s40168-018-0406-7.
19.
Rhoads WJ, Ji P, Pruden A, Edwards MA. Water heater temperature set point and water use patterns influence Legionella pneumophila and associated microorganisms at the tap. Microbiome. 2015;3:67. Published 2015 Dec 1. doi:10.1186/s40168-015-0134-1.
20.
Kruse EB, Wehner A, Wisplinghoff H. Prevalence and distribution of Legionella spp in potable water systems in Germany, risk factors associated with contamination, and effectiveness of thermal disinfection. Am J Infect Control. 2016;44(4):470–474. doi:10.1016/j.ajic.2015.10.025.
21.
Deiana G, Arghittu A, Dettori M, Masia MD, Deriu MG, Piana A, Muroni MR, Castiglia P, Azara A. Environmental Surveillance of Legionella spp. in an Italian University Hospital Results of 10 Years of Analysis. Water. 2021;13(16):2304. https://doi.org/10.3390/w13162....
22.
Zborowska-Dobosz R, Kuziemski A, Maron M, Bahn D, Owczarek A. Kolonizacja szpitalnych sieci wody ciepłej Legionella sp. w świetle badań prowadzonych w latach 2008–2010 w ramach nadzoru przez Państwowego Powiatowego Inspektora Sanitarnego w Bydgoszczy. Przegl Epidemiol. 2011;65(3):441–5.
23.
Sikora A, Wójtowicz-Bobin M, Kozioł-Montewka M, Magryś A, Gładysz I. Prevalence of Legionella pneumophila in water distribution systems in hospitals and public buildings of the Lublin region of eastern Poland. Ann Agric Environ Med. 2015;22(2):195–201. doi:10.5604/12321966.1152064.
24.
Fragou K, Kokkinos P, Gogos C, Alamanos Y, Vantarakis A. Prevalence of Legionella spp. in water systems of hospitals and hotels in South Western Greece. Int J Environ Health Res. 2012;22(4):340–354. doi:10.1080/09603123.2011.643229.
25.
Wojtyła-Buciora P, Chrzanowska E, Marcinkowski JT. Występowanie pałeczek Legionella sp. w instalacjach ciepłej wody użytkowej w zakładach opieki zdrowotnej oraz budynkach użyteczności publicznej Hygeia Public Health 2013;48(3):327–332.
26.
Gavaldà L, Garcia-Nuñez M, Quero S, Gutierrez-Milla C, Sabrià M. Role of hot water temperature and water system use on Legionella control in a tertiary hospital: An 8-year longitudinal study. Water Res. 2019;149:460–466. doi:10.1016/j.watres.2018.11.032.
27.
Godič-Torkar K, Oder M. The influence of temperature, disinfection and water softening of drinking water on the multiplication of Legionella pneumophila. Inter J Sanitary Engin Res. 2018;12(1):34–42.
28.
Sawczyn-Domańska A. Detection of Legionella spp. and occurrence of virulence genes: lvh, rtxA and enhC in water samples from artificial water systems. Ann Agric Environ Med. 2021;28(4):617–620. doi:10.26444/aaem/143745.
29.
Gładysz I, Sikora A, Wójtowicz-Bobin M, Szepeluk A, Matuszewska R, Bartosik M, Karczewski J. Antibiotic sensitivity of environmental Legionella pneumophila strains isolated in Poland. Ann Agric Environ Med. 2023;30(4):602–605. doi: https://doi.org/10.26444/aaem/....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.