Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Surface electromyography vs clinical outcome measures after robot-assisted gait training in patients with spinal cord injury after post-acute phase of rehabilitation
1
Research Institute for Innovative Methods of Rehabilitation of Patients with Spinal Cord Injury in Kamień Pomorski, Health Resort Kamień Pomorski, Poland
2
Department of Rehabilitation, Medical University of Warsaw, Warsaw, Poland
3
EGZOTech Sp. z o.o., Gliwice, Poland
4
Faculty of Science and Technology, University of Silesia, Chorzów, Poland
Ann Agric Environ Med. 2024;31(4):599-608
KEYWORDS
TOPICS
Exposure to physical hazards associated with the use of machinery in agriculture and forestry: noise, vibration, dustWork-related accidents and injuries in agriculture, forestry, food industry and wood industry: incidence, causes, social aspects and prevention
ABSTRACT
Introduction and objective:
Surface electromyography (sEMG) measurements are a valid method for sublesional muscle activity following spinal cord injury (SCI). In the literature there are few reports evaluating the effect of robotic assisted gait training (RAGT) on the sEMG properties change in SCI patients. The aim of this study was to evaluate the influence of RAGT on observed change of sEMG, and in 64 incomplete SCI patients in the sub-acute stage in relation to functional scales.
Material and methods:
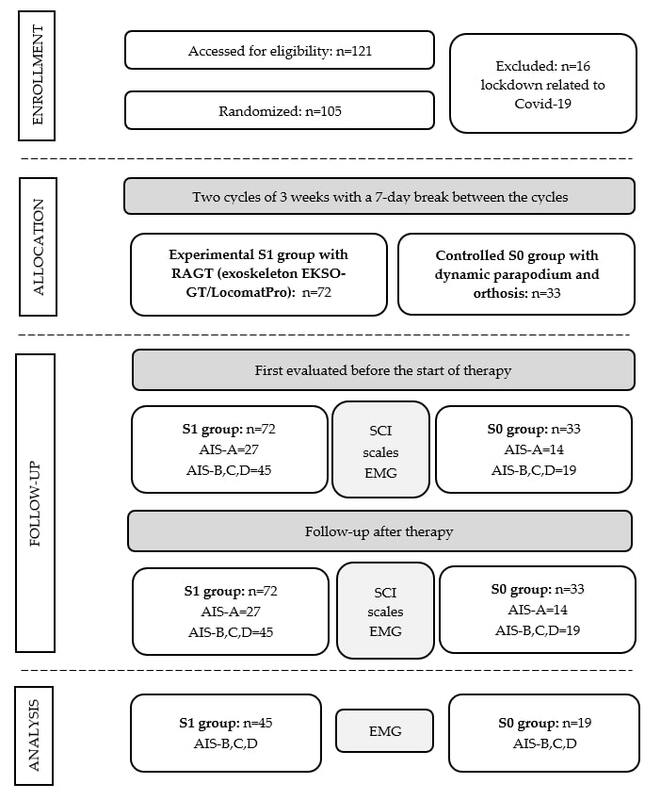
In the presented single-centre single arm, single-blinded study, the patients were divided into two groups: experimental group with RAGT (exoskeleton EKSO-GT or Locomat-Pro) and the control group with dynamic parapodium training (DPT). The therapy was conducted in two cycles of three weeks for six days a week, with a seven day break between cycles. Obtained measurements were averaged peak muscle amplitude (AMA) in sEMG and maximal torque (MT) on Luna apparatus (muscle strength testing) and functional scales.
Results:
Statistically significant differences between S0 and S1 were only observed for the change in MT values at the knee joint during extension, and positively correlated with American Spinal Injury Association Impairment Scale, lower limb motor score, and functional scales. A statistically increased value of the Walking Index for Spinal Cord Injury (WISCI-II) and motor score after rehabilitation relative to the initial value, was seen after RAGT in comparison to patients with DPT, but AMA did not differ between patients
Conclusions:
sEMG did not provide sufficient information about SCI outcome after RAGT rehabilitation.
Surface electromyography (sEMG) measurements are a valid method for sublesional muscle activity following spinal cord injury (SCI). In the literature there are few reports evaluating the effect of robotic assisted gait training (RAGT) on the sEMG properties change in SCI patients. The aim of this study was to evaluate the influence of RAGT on observed change of sEMG, and in 64 incomplete SCI patients in the sub-acute stage in relation to functional scales.
Material and methods:
In the presented single-centre single arm, single-blinded study, the patients were divided into two groups: experimental group with RAGT (exoskeleton EKSO-GT or Locomat-Pro) and the control group with dynamic parapodium training (DPT). The therapy was conducted in two cycles of three weeks for six days a week, with a seven day break between cycles. Obtained measurements were averaged peak muscle amplitude (AMA) in sEMG and maximal torque (MT) on Luna apparatus (muscle strength testing) and functional scales.
Results:
Statistically significant differences between S0 and S1 were only observed for the change in MT values at the knee joint during extension, and positively correlated with American Spinal Injury Association Impairment Scale, lower limb motor score, and functional scales. A statistically increased value of the Walking Index for Spinal Cord Injury (WISCI-II) and motor score after rehabilitation relative to the initial value, was seen after RAGT in comparison to patients with DPT, but AMA did not differ between patients
Conclusions:
sEMG did not provide sufficient information about SCI outcome after RAGT rehabilitation.
REFERENCES (51)
1.
GBD Spinal Cord Injuries Collaborators. Global, regional, and national burden of spinal cord injury, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2023 Nov;22(11):1026–1047. doi:10.1016/S1474-4422(23)00287-9. Erratum in: Lancet Neurol. 2024 Apr;23(4):e8. PMID: 37863591; PMCID: PMC10584692.
2.
Tarnacka B, Korczyński B, Frasuńska J. Long-term complications following spinal cord injury and aging. Adv Psychiatry Neurol. 2020;29(4):234–245. doi:10.5114/ppn.2020.103635.
3.
Budd MA, Gater DRJr, Channell I. Psychosocial Consequences of Spinal Cord Injury: A Narrative Review. J Pers Med. 2022;12(7):1178. doi:10.3390/jpm12071178.
4.
Aarabi B, Albrecht JS, Simard JM, et al. Trends in demographics and markers of injury severity in traumatic spinal cord injury. J Neurotraum. 2021;38(6):756–764. doi:10.1089/neu.2020.7415.
5.
Kirshblum S, Snider B, Eren F, et al. Characterizing Natural Recovery after Traumatic Spinal Cord Injury. J Neurotrauma. 2021;38(9):1267–1284. doi:10.1089/neu.2020.7473.
6.
Edwards DJ, Forrest G, Cortes M, et al. Walking improvement in chronic incomplete spinal cord injury with exoskeleton robotic training (WISE): a randomized controlled trial. Spinal Cord. 2022;60(6):522–532. doi:10.1038/s41393-022-00751-8.
7.
Duan R, Qu M, Yuan Y, et al. Clinical benefit of rehabilitation training in spinal cord injury. Spine. 2021;46(6):398–410. doi:10.1097/BRS.0000000000003789.
8.
Mekki M, Delgado AD, Fry A, et al. Robotic rehabilitation and spinal cord injury: a narrative review. Neurotherapeutics. 2018;15:604–617. doi:10.1007/s13311-018-0642-3.
9.
Holanda LJ, Silva PMM, Amorim TC, et al. Robotic assisted gait as a tool for rehabilitation of individuals with spinal cord injury: a systematic review. J Neuroeng Rehabil. 2017;14:126–132. doi:10.1186/s12984-017-0338-7.
10.
Nam KY, Kim HJ, Kwon BS, et al. Robot-assisted gait training (Lokomat) improves walking function and activity in people with spinal cord injury: a systematic review. J Neuroeng Rehabil. 2017;14(1):24. doi:10.1186/s12984-017-0232-3.
11.
Tamburella F, Lorusso M, Tramontano M, et al. Overground robotic training effects on walking and secondary health conditions in individuals with spinal cord injury: systematic review. J Neuroeng Rehabil. 2022;19(1):27. doi:10.1186/s12984-022-01003-9.
12.
Cappellini G, Sylos-Labini F, Assenza C, et al. Clinical Relevance of State-of-the-Art Analysis of Surface Electromyography in Cerebral Palsy. Front Neurol. 2020;11:583296. doi: 10.3389/fneur.2020.583296.
13.
Alamro RA, Chisholm AE, Williams AMM, et al. Overground walking with a robotic exoskeleton elicits trunk muscle activity in people with high-thoracic motor-complete spinal cord injury. J Neuroeng Rehabil. 2018;15(1):109. doi:10.1186/s12984-018-0453-0.
14.
Borin JS, Capelari TV, Goldhardt MG, et al. Advantage in muscle activation in gait with support of body weight in spinal cord injury. Fisioter Mov. 2018;31:e003129. doi:10.1590/1980-5918.031.ao29.
15.
Afsharipour B, Sandhu MS, Rasool G, et al. Using surface electromyography to detect changes in innervation zones pattern after human cervical spinal cord injury. Annu Int Conf IEEE Eng Med Biol Soc. 2016;2016:3757–3760. doi:10.1109/EMBC.2016.7591545.
16.
Knox J, Gupta A, Banwell HA, et al. Comparison of EMG signal of the flexor hallucis longus recorded using surface and intramuscular electrodes during walking. J Electromyogr Kines. 2021;60:102574. doi:10.1016/j.jelekin.2021.
17.
Smith LH, Hargrove LJ. Comparison of surface and intramuscular EMG pattern recognition for simultaneous wrist/hand motion classification. Annu Int Conf IEEE Eng Med Biol Soc. 2013;2013:4223–4226. doi:10.1109/EMBC.2013.6610477.
18.
Hargrove LJ, Englehart K, Hudgins B. A comparison of surface and intramuscular myoelectric signal classification. IEEE Trans Biomed Eng. 2007;54(5):847–853. doi:10.1109/TBME.2006.889192.
19.
American Spinal Injury Association. International Standards for Neurological Classification of Spinal Cord Injury, 2002 Revision. Chicago, IL: American Spinal Injury Association; 2002.
20.
Itzkovich M, Gelernter I, Biering-Sorensen F, et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil. 2007;29:1926–33. doi:10.1080/09638280601046302.
21.
Ditunno JF, Scivoletto G, Patrick M, et al. Validation of the walking index for spinal cord injury in a US and European clinical population. Spinal Cord. 2008;46:181–8. doi:10.1038/sj.sc.3102071.
22.
Collin C, Wade DT, Davies S, et al. The Barthel ADL index: a reliability study. Int Disabil Stud. 1988;2:61–63. doi:10.3109/09638288809164103.
23.
Harb A, Kishner S. Modified Ashworth Scale. 2023 May 1. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. https://www.ncbi.nlm.nih.gov/b....
24.
Hermens HJ, Freriks B, Merletti R, et al. SENIAM 8: European Recommendations for Surface Electromyography. RoessinghResearch and Development. Enschede, The Netherlands: Roess-ingh Research and Development; 1999. http://www.seniam.org/pdf/cont....
25.
Lewandowska-Sroka P, Stabrawa R, Kozak D, et al. The Influence of EMG-Triggered Robotic Movement on Walking, Muscle Force and Spasticity after an Ischemic Stroke. Medicina (Kaunas). 2021;57(3):227. doi:10.3390/medicina57030227.
26.
Oleksy Ł, Królikowska A, Mika A, et al. A Reliability of Active and Passive Knee Joint Position Sense Assessment Using the Luna EMG Rehabilitation Robot. Int J Env Res Pub He. 2022;19(23):15885. doi:10.3390/ijerph192315885.
27.
Stańczyk K, Poświata A, Roksela A, et al. Assessment of Muscle Fatigue, Strength and Muscle Activation During Exercises with the Usage of Robot Luna EMG, Among Patients with Multiple Sclerosis. In: Pietka E, Badura P, Kawa J, Wieclawek W, editors. Information Technology in Biomedicine. ITIB 2019. Advances in Intelligent Systems and Computing, vol 1011. Springer, Cham. doi:10.1007/978-3-030-23762-2_11.
28.
Olczak A, Truszczyńska-Baszak A, Gniadek-Olejniczak K. The Relationship between the Static and Dynamic Balance of the Body, the Influence of Eyesight and Muscle Tension in the Cervical Spine in CAA Patients-A Pilot Study. Diagnostics (Basel). 2021;11(11):2036. doi:10.3390/diagnostics11112036.
29.
Olczak A, Truszczyńska-Baszak A. Influence of the Passive Stabilization of the Trunk and Upper Limb on Selected Parameters of the Hand Motor Coordination, Grip Strength and Muscle Tension, in Post-Stroke Patients. J Clin Med. 2021;10(11):2402. doi:10.3390/jcm10112402.
30.
Olczak A. Importance of core stability for coordinated movement of the human body in stroke rehabilitation. Neurol Res. 2022;44(1):7–13. doi:10.1080/01616412.2021.1950952.
31.
Zasadzka E, Tobis S, Trzmiel T, et al. Application of an EMG-Rehabilitation Robot in Patients with Post-Coronavirus Fatigue Syndrome (COVID-19)-A Feasibility Study. Int J Env Res Pub He. 2022;19(16):10398. doi:10.3390/ijerph191610398.
32.
Trzmiel T, Marchewka R, Pieczyńska A, et al. The Effect of Using a Rehabilitation Robot for Patients with Post-Coronavirus Disease (COVID-19) Fatigue Syndrome. Sensors (Basel). 2023;23(19):8120. doi:10.3390/s23198120.
33.
Wickham H, Bryan J. (2019). readxl: Read Excel Files. R package version 1.3.1. https://CRAN.R-project.org/pac....
34.
Wickham H. (2016). ggplot2: Elegant Graphics for Data Analysis. Springer-Verlag New York. ISBN 978-3-319-24277-4. http://ggplot2.org.
35.
DeWitt P. (2021). qwraps2: Quick Wraps 2. R package version 0.5.2. https://CRAN.R-project.org/pac....
36.
Allaire J, Xie Y, McPherson J, et al (2022). rmarkdown: Dynamic Documents for R. R package version 2.14. https://github.com/rstudio/rma....
37.
Kassambara A. (2018). ggpubr: “ggplot2” Based Publication Ready Plots. https://cran.r-project.org/pac....
38.
Hugh-Jones D. huxtable: Easily Create and Style Tables for ## LaTeX, HTML and Other Formats. R package version 5.4.0; 2021. https://CRAN.R-project.org/pac....
39.
Wickham H, et al. Welcome to the tidyverse. J Open Source Soft. 2019;4(43):1686. https://doi.org/10.21105/joss.....
40.
Silverman JD, Balbinot G, Masani K, et al. Validity and Reliability of Surface Electromyography Features in Lower Extremity Muscle Contraction in Healthy and Spinal Cord-Injured Participants. Top Spinal Cord Inj Rehabil. 2021;27(4):14–27. doi:10.46292/sci20-00001.
41.
Calancie B, Molano MR, Broton JG. EMG for assessing the recovery of voluntary movement after acute spinal cord injury in man. Clin Neurophysiol. 2004;115(8):1748–1759. doi:10.1016/j.clinph.2004.03.002.
42.
Dorneles JR, Neto FR, Gonçalves CW, et al. Does prolonged walking cause greater muscle fatigability in individuals with incomplete spinal cord injury compared with matched-controls? Gait Posture. 2020;78:65–71. doi:10.1016/j.gaitpost.2020.03.014.
43.
Gollie JM. Fatigability during volitional walking in incomplete spinal cord injury: cardiorespiratory and motor performance considerations. Neural Regen Res. 2018;13(5):786–790. doi:10.4103/1673-5374.232461.
44.
Hussey RW, Stauffer ES. Spinal cord injury: requirements for ambulation. Arch Phys Med Rehab. 1973;54(12):544–547.
45.
Cheung EYY, Yu KKK, Kwan RLC, et al. Effect of EMG-biofeedback robotic-assisted body weight supported treadmill training on walking ability and cardiopulmonary function on people with subacute spinal cord injuries – a randomized controlled trial. BMC Neurol. 2019;19(1):140. doi:10.1186/s12883-019-1361-z.
46.
Zieriacks A, Aach M, Brinkemper A, et al. Rehabilitation of Acute Vs. Chronic Patients With Spinal Cord Injury With a Neurologically Controlled Hybrid Assistive Limb Exoskeleton: Is There a Difference in Outcome? Front Neurorobotics. 2021;15:728327. doi:10.3389/fnbot.2021.728327.
47.
Benito-Penalva J, Edwards DJ, Opisso E, et al. Gait training in human spinal cord injury using electromechanical systems: effect of device type and patient characteristics. Arch Phys Med Rehab. 2012;93:404–412. doi:10.1016/j.apmr.2011.08.028.
48.
Fang CY, Tsai JL, Li GS, et al. Effects of Robot-Assisted Gait Training in Individuals with Spinal Cord Injury: A Meta-analysis. Biomed Res Int. 2020;2020:2102785.
49.
Agostini V, Ghislieri M, Rosati S, et al. Surface Electromyography Applied to Gait Analysis: How to Improve Its Impact in Clinics? Front Neurol. 2020;11:994. doi:10.3389/fneur.2020.00994.
50.
Balbinot G, Li G, Wiest MJ, et al. Properties of the surface electromyogram following traumatic spinal cord injury: a scoping review. J Neuroeng Rehabil. 2021;18(1):105. doi:10.1186/s12984-021-00888-2.
51.
Pilkar R, Momeni K, Ramanujam A, et al. Use of Surface EMG in Clinical Rehabilitation of Individuals With SCI: Barriers and Future Considerations. Front Neurol. 2020;11:578559. doi:10.3389/fneur.2020.578559.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.