Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Strategies for coping with stress used by nurses during the COVID-19 pandemic
1
Department of Internal Medicine and Internal Medicine in Nursing, Medical University of Lublin, Lublin, Poland
2
University of Siedlce, Faculty of Medical and Health Sciences, Siedlce, Poland
3
Department of Medical Informatics and Statistics with E-Health Lab, Medical University of Lublin, Lublin, Poland
4
Faculty of Health Sciences, Radom Higher School, Radom, Poland
5
Department of Orthodox Theology, The John Paul II Catholic University, Lublin, Poland
Corresponding author
Maria Malm
Department of Medical Informatics and Statistics with E-learning Lab, Medical University of Lublin, Jaczewskiego 4, 20-090, Lublin, Poland
Department of Medical Informatics and Statistics with E-learning Lab, Medical University of Lublin, Jaczewskiego 4, 20-090, Lublin, Poland
Ann Agric Environ Med. 2024;31(4):616-625
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The subject of the article are the strategies used by nurses working in COVID-19 hospital units for coping with stress. The aim of the study was to make a comparative analysis between the styles, strategies and behaviours practiced by nurses working in COVID units and the nurses working in conservative treatment and surgical units.
Material and methods:
For the study we used the Polish adaptation of Ch. S. Carver’s standardized “Inventory for Measuring Coping with Stress Mini-COPE” (Brief-COPE), created by Z. Juczyński and N. Ogińska-Bulik. The research was carried out in 2021 on a group of 225 nurses working in different hospital units.
Results:
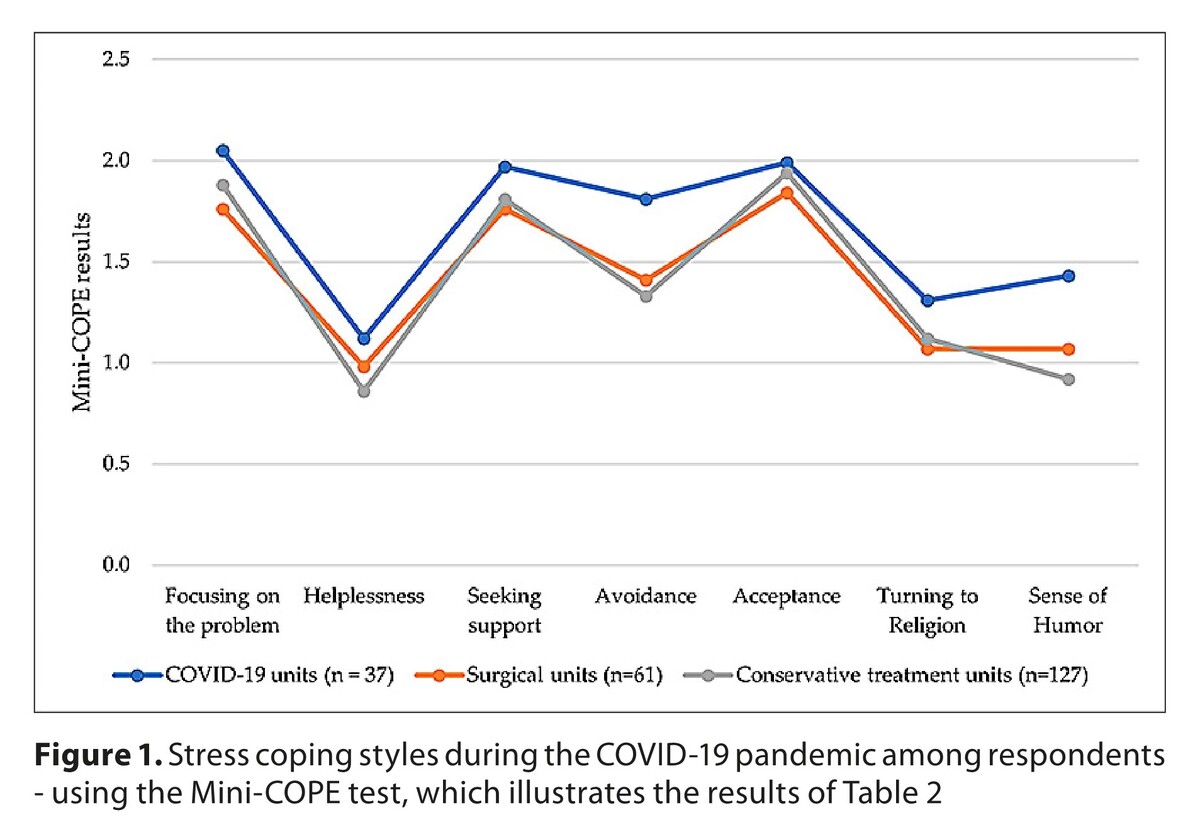
The results showed that in the COVID-19 units, avoidance and humor were used as coping strat-egies significantly more often than in the surgical and conservative treatments units. The observed strategies included planning, positive revaluation, use of psychoactive substances, preoccupation with other activities, denial, emotional discharge, and humor. Factors such as age, sex, marital status, education or place of residence turned out to have an influence on the ways of coping practiced by particular nurses.
Conclusions:
There is a clear distinction between the strategies, styles and behaviours observed among nurses working in COVID-19 units, and the ways of coping practiced by nurses working in non-COVID-19 units (conservative treatment and surgical). Nurses working in COVID-19 units were more likely to deny facts, distract themselves with different activities, or downplay the seriousness of the situation by joking and treating the situation with fun and humor, but also to use planning and positive reevaluation to cope with stress.
The subject of the article are the strategies used by nurses working in COVID-19 hospital units for coping with stress. The aim of the study was to make a comparative analysis between the styles, strategies and behaviours practiced by nurses working in COVID units and the nurses working in conservative treatment and surgical units.
Material and methods:
For the study we used the Polish adaptation of Ch. S. Carver’s standardized “Inventory for Measuring Coping with Stress Mini-COPE” (Brief-COPE), created by Z. Juczyński and N. Ogińska-Bulik. The research was carried out in 2021 on a group of 225 nurses working in different hospital units.
Results:
The results showed that in the COVID-19 units, avoidance and humor were used as coping strat-egies significantly more often than in the surgical and conservative treatments units. The observed strategies included planning, positive revaluation, use of psychoactive substances, preoccupation with other activities, denial, emotional discharge, and humor. Factors such as age, sex, marital status, education or place of residence turned out to have an influence on the ways of coping practiced by particular nurses.
Conclusions:
There is a clear distinction between the strategies, styles and behaviours observed among nurses working in COVID-19 units, and the ways of coping practiced by nurses working in non-COVID-19 units (conservative treatment and surgical). Nurses working in COVID-19 units were more likely to deny facts, distract themselves with different activities, or downplay the seriousness of the situation by joking and treating the situation with fun and humor, but also to use planning and positive reevaluation to cope with stress.
REFERENCES (50)
1.
Biegańska-Banaś JM, Makara-Studzińska M. Coping strategies among nurses during the COVID-19 outbreak. Nursing Problems. 2020;28(1):1–11. https://doi.org/10.5114/ppiel.....
2.
Backer JH, Bakas T, Bennett SJ, et al. Coping with stress: Programs of nursing research. In: Rice VH, editor. Handbook of stress, coping, and health: Implication for nursing research, theory, and practice. Thousand Oaks, CA, USA: Sage Publications; 2000. p. 223–263.
3.
Demerouti E, Bakker AB, Nachreiner F, et al. The job demands-resources model of burnout. J Appl Psychol. 2001;86:499–512.
4.
Lazarus RS. Stress and Emotion: A New Synthesis. New York, NY, USA: Springer; 1999.
5.
Folkman S, Lazarus RS, Pimley S, et al. Age differences in stress and coping processes. Psychol Aging. 1987;2(2):171–184. http://dx.doi.org/10.1037/0882....
6.
Martínez JP, Méndez I, Ruiz-Esteban C, et al. Profiles of Burnout, Coping Strategies and Depressive Symptomatology. Front Psychol. 2020;11:591. https://doi.org/10.3389/fpsyg.....
7.
Munawar K, Choudhry FR. Exploring stress coping strategies of frontline emergency health workers dealing with Covid-19 in Pakistan: A qualitative inquiry. Am J Infect Control. 2020;49(3):286–292. https://doi.org/10.1016/j.ajic....
8.
Lazarus RS, Folkman S. Stress, appraisal, and coping. New York, NY, USA: Springer; 1984. (Available from: https://books.google.com/books...).
9.
Endler NS, Parker JDA. Coping Inventory for Stressful Situations (CISS): Manual. Toronto, Canada: Multi-Health Systems; 1990.
10.
Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–83. https://doi.org/10.1037/0022-3....
11.
Juczyński Z, Ogińska-Bulik N. Tools for Measuring Stress and Coping with Stress. Handbook. Warsaw, Poland: Psychological Testing Laboratory of the Polish Psychological Association; 2012.
12.
Gonzalez A, Cervoni C, Lochner M, et al. Supporting health care workers during the COVID-19 pandemic: Mental health support initiatives and lessons learned from an academic medical center. Psychol Trauma. 2020;12(1):168–170. https://doi.org/10.1037/tra000....
13.
McFadden P, Ross J, Moriarty J, et al. The Role of Coping in the Wellbeing and Work-Related Quality of Life of UK Health and Social Care Workers during COVID-19. Int J Environ Res Public Health. 2021;18(2):815. https://doi.org/10.3390/ijerph....
14.
Alnazly EK, Hjazeen AA. Psychological Distress and Coping Strategies among Nurses during the COVID-19 Pandemic: A Cross-Sectional Online Survey. Open Nurs J. 2021;1:262–272. https://doi.org/10.2174/187443....
15.
Ing EB, Xu QA, Salimi A, et al. Physician deaths from corona virus (COVID-19) disease. Occup Med (Lond). 2020;70(5):370–374. https://doi.org/10.1093/occmed....
16.
Chirico F, Nucera G, Magnavita N. Protecting the mental health of healthcare workers during the COVID-19 emergency. BJPsych International. 2020;18(1):1–2. https://doi.org/10.1192/bji.20....
17.
Htay MNN, Marzo RR, Bahari R, et al. How are healthcare workers coping with mental health challenges during COVID-19 pandemic? – A cross-sectional multi-countries study. Clin Epidemiol Glob Health. 2021;11:100759. https://doi.org/10.1016/j.cegh....
18.
Farquharson B, Bell C, Johnston D, et al. Nursing stress and patient care: real-time investigation of the effect of nursing tasks and demands on psychological stress, physiological stress, and job performance: studyprotocol. J Adv Nurs. 2013;69(10):2327–2335. https://doi.org/10.1111/jan.12....
19.
Mark G, Smith AP. Occupational stress, job characteristics, coping, and the mental health of nurses. Br J Health Psychol. 2012;17(3):505–521. https://doi.org/10.1111/j.2044....
20.
Keykaleh MS, Safarpour H, Yousefian S, et al. The Relationship between Nurse’s Job Stress and Patient Safety. Open Access Maced J Med Sci. 2018;6(11):2228–2232. https://doi.org/10.3889/oamjms....
21.
Lai J, Ma S, Wang Y, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3(3):e203976. https://doi.org/10.1001/jamane....
22.
Rowe J. The Suffering of the Healer. Nurs Forum. 2003;38:16–20. https://doi.org/10.1111/j.0029....
23.
Park YM, Kim SY. Impacts of Job Stress and Cognitive Failure on Patient Safety Incidents among Hospital Nurses. Saf Health Work. 2013;4(4):210–215. https://doi.org/10.1016/j.shaw....
24.
Rosenbaum L. Facing COVID-19 in Italy – ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med. 2020;382:1873–1875. https://doi.org/10.1056/NEJMp2....
25.
Karimi Z, Fereidouni Z, Behnammoghadam M, et al. The lived experience of nurses caring for patients with COVID-19 in Iran: a phenomenological study. Risk Manag Healthc Policy. 2020;13:1271–1278. https://doi.org/10.2147/RMHP.S....
26.
Beh LS, Loo LH. Job Stress and Coping Mechanisms among Nursing Staff in Public Health Services. Int J Acad Res Business Soc Sci. 2012;2:131–176.
27.
Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. https://doi.org/10.1016/S2215-....
28.
Chatzigianni D, Tsounis A, Markopoulos N, et al. Occupational Stress Experienced by Nurses Working in a Greek Regional Hospital: A Cross sectional Study. Iran J Nurs Midwifery Res. 2018;23(6):450–457. https://doi.org/10.4103/ijnmr.....
29.
Góral-Pólrola J, Kochańska E, Cielebąk K, et al. A new, neuromarker-based, form of combined neurofeedback EEG/tDCS training in the reduction of occupational burnout syndrome in an anaesthetic nurse working with COVID-19 patients. Acta Neuropsychol. 2024;22(3):301–330. https://doi.org/10.5604/01.300....
30.
Xu J, He Y. Psychological health and coping strategy among survivors in the year following the 2008 Wenchuan earthquake. Psychiatry Clin Neurosci. 2012;66(3):210–9. https://doi.org/10.1111/j.1440....
31.
Ursin H, Eriksen HR. The Cognitive Activation Theory of Stress. Psychoneuroendocrinol. 2004;29:567–592. https://doi.org/10.1016/S0306-....
32.
Carver CS. You want to measure coping but your protocol’s too long: consider the brief COPE. Int J Behav Med. 1997;4:92–100. https://doi.org/10.1207/s15327....
33.
Ali H, Cole A, Ahmed A, et al. Major stressors and coping strategies of frontline nursing staff during the outbreak of coronavirus disease 2020 (COVID-19) in Alabama. J Multidiscip Healthc. 2020;13:2057. https://doi.org/10.2147/JMDH.S....
34.
Sheroun D, Wankhar D, Devrani A, et al. A study to assess the perceived stress and coping strategies among BSc nursing students of selected colleges in Pune during COVID-19 pandemic lockdown. Int J Sci Healthcare Res. 2020;5(2):280–288.
35.
McFadden P, Ross J, Moriarty J, et al. The Role of Coping in the Wellbeing and Work-Related Quality of Life of UK Health and Social Care Workers during COVID-19. Int J Environ Res Public Health. 2021;18(2):81.
36.
Bartzik M, Aust F, Peifer C. Negative effects of the COVID-19 pandemic on nurses can be buffered by a sense of humor and appreciation. BMC Nurs. 2021;20:1–12. https://doi.org/10.1186/s12912....
37.
Yubonpunt P, Kunno J, Supawattanabodee B, et al. Prevalence of perceived stress and coping strategies among healthcare workers during the COVID-19 outbreak at Bangkok metropolitan, Thailand. PLoS One. 2022;17(7):e0270924. https://doi.org/10.1371/journa....
38.
Hobfoll SE. Stress, culture, and community: the psychology and philosophy of stress. New York, NY, USA: Springer Science & Business Media; 2004.
39.
Kandeğer A, Aydın M, Altınbaş K, et al. Evaluation of the relationship between perceived social support, coping strategies, anxiety, and depression symptoms among hospitalized COVID-19 patients. Int J Psychiatry Med. 2021;56(4):240–254. https://doi.org/10.1177/009121....
40.
Liang Y, Chen M, Zheng X, et al. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J Psychosom Res. 2020;133:110102. https://doi.org/10.1016/j.jpsy....
41.
Flesia L, Monaro M, Mazza C, et al. Predicting Perceived Stress Related to the Covid-19 Outbreak through Stable Psychological Traits and Machine Learning Models. J Clin Med. 2020;9(10):3350. https://doi.org/10.3390/jcm910....
42.
Babore A, Lombardi L, Viceconti ML, et al. Psychological effects of the COVID-2019 pandemic: Perceived stress and coping strategies among healthcare professionals. Psychiatry Res. 2020;293:113366. https://doi.org/10.1016/j.psyc....
43.
Huang L, Lei W, Xu F, et al. Emotional responses and coping strategies in nurses and nursing students during Covid-19 outbreak: A comparative study. PLoS One. 2020;15(8):e0237303. https://doi.org/10.1371/journa....
44.
Rose S, Hartnett J, Pillai S. Healthcare worker’s emotions, perceived stressors and coping mechanisms during the COVID-19 pandemic. PLoS One. 2021;16(7):e0254252. https://doi.org/10.1371/journa....
45.
Hammami AS, Jellazi M, Mahjoub L, et al. Psychological Impact of the COVID-19 Pandemic on Healthcare Professionals in Tunisia: Risk and Protective Factors. Front Psychol. 2021;12:754047. https://doi.org/10.3389/fpsyg.....
46.
Park CL, Russell BS, Fendrich M, et al. Americans’ COVID-19 stress, coping, and adherence to CDC guidelines. J Gen Intern Med. 2020;35(8):2296–2303. https://doi.org/10.1007/s11606....
47.
Yoshida E, Yamada K, Morioka I. Sense of coherence (SOC), occupational stress reactions, and the relationship of SOC with occupational stress reactions among male nurses working in a hospital. Sangyo Eiseigaku Zasshi. 2014;56(5):152–61. https://doi.org/10.1539/sangyo....
48.
Wilczek-Rużyczka E. Empathy and resilience in health care professionals. Acta Neuropsychol. 2023;21(4):395–410. https://doi.org/10.5604/01.300....
49.
Aknin L, De Neve J, Dunn E, et al. The neurological consequences of contracting COVID-19. Acta Neuropsychol. 2021;19(3):301–305. https://doi.org/10.5604/01.300....
50.
Pąchalska M. Goal-oriented neuropsychological rehabilitation with EEG-neurofeedback for a visual artist with PTSD resulting from SARS-CoV-2 infection, followed by a severe course of neuroCOVID and the sequelae of long term pharmacologically-induced coma. Acta Neuropsychol. 2022;20(4):485–514. https://doi.org/10.5604/01.300....
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.