Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Strategies for coping with stress, emotional control and occupational burnout among surgical nurses
1
Collegium Medicum, Jan Kochanowski University, Kielce, Poland
2
Health Care Unit, John Paul II District Hospital, Włoszczowa, Poland
3
Department of Public Health, International European University, Kyiv, Ukraine
4
Department of Medical Anthropology, Institute of Rural Health, Lublin, Poland
5
Faculty of Humanities, Jan Kochanowski University, Kielce, Poland
6
Medical University, Warsaw, Poland
7
National Medical Institute of the Ministry of Interior and Administration, Warsaw, Poland
Corresponding author
Ann Agric Environ Med. 2024;31(4):473-478
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Nursing staff constitute 59% of the total number of health care workers worldwide – a total of 27.9 million people. The aim of the study is assessment of the prevalence of stress, including strategies for coping with stress, emotional control, and occupational burnout syndrome, as well as the effect of chronic stress on occupational burnout among surgical nurses.
Material and methods:
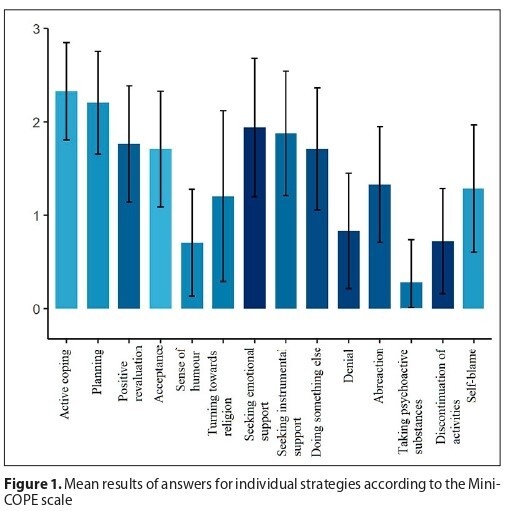
The study included 323 surgical nurses employed in hospitals in the Kielce Province, Poland. Applying the inclusion and exclusion criteria from the study, ultimately, 110 nurses participated in the project. The research tools were standardized questionnaires: PSS-10 (Scale of Experienced Stress), Mini-COPE (Coping Orientations to Problems Experienced), CECS (Courtauld Emotional Control Scale), and LBQ (Link Burnout Questionnaire).
Results:
The highest mean level of occupational burnout observed was related with the scale of psychophysical exhaustion (raw values: 17.49 ± 5.46, stens: 5.53 ± 1.53), whereas the lowest mean result was related with the scale of the feeling of the lack of professional effectiveness (raw values: 13.16 ± 3.82, stens: 5:52 ± 1.65). While analyzing the relationships between the results of LBQ concerning psychophysical exhaustion and the results according to the PSS-10 and Mini-Cope scales, a statistically significant correlation was observed with the result of the PSS-10 (p < 0.001), concerning both raw and sten results.
Conclusions:
Stress is an important factor in the occurrence of the symptoms of occupational burnout in the work of surgical nurses. Two-fifths of scrub nurses experienced a high level of stress. A relationship was found between the feeling of lack of professional effectiveness and anxiety control. Persons who experienced a low own effectiveness strongly suppressed the feeling of anxiety
Nursing staff constitute 59% of the total number of health care workers worldwide – a total of 27.9 million people. The aim of the study is assessment of the prevalence of stress, including strategies for coping with stress, emotional control, and occupational burnout syndrome, as well as the effect of chronic stress on occupational burnout among surgical nurses.
Material and methods:
The study included 323 surgical nurses employed in hospitals in the Kielce Province, Poland. Applying the inclusion and exclusion criteria from the study, ultimately, 110 nurses participated in the project. The research tools were standardized questionnaires: PSS-10 (Scale of Experienced Stress), Mini-COPE (Coping Orientations to Problems Experienced), CECS (Courtauld Emotional Control Scale), and LBQ (Link Burnout Questionnaire).
Results:
The highest mean level of occupational burnout observed was related with the scale of psychophysical exhaustion (raw values: 17.49 ± 5.46, stens: 5.53 ± 1.53), whereas the lowest mean result was related with the scale of the feeling of the lack of professional effectiveness (raw values: 13.16 ± 3.82, stens: 5:52 ± 1.65). While analyzing the relationships between the results of LBQ concerning psychophysical exhaustion and the results according to the PSS-10 and Mini-Cope scales, a statistically significant correlation was observed with the result of the PSS-10 (p < 0.001), concerning both raw and sten results.
Conclusions:
Stress is an important factor in the occurrence of the symptoms of occupational burnout in the work of surgical nurses. Two-fifths of scrub nurses experienced a high level of stress. A relationship was found between the feeling of lack of professional effectiveness and anxiety control. Persons who experienced a low own effectiveness strongly suppressed the feeling of anxiety
REFERENCES (25)
2.
Banasiewicz R, Antos E, Śniegocka M. Wypalenie zawodowe jako konsekwencja stresu w pracy pielęgniarek oddziałów zabiegowych. Pol Prz Nauk Zdr. 2017;4(53):488–495.
3.
Bakker AB, Killmer CH, Siegrist J, et. al. Effort-reward imbalance and burnout among nurses. J Adv Nurs. 2000;31(3):884–891. doi:10.1046/j.1365-2648.2000.01361.x.
4.
Schulz M, Damkroger A, Heins C, et al. Effort – reward imbalance and burnout among German nurses in medical compared with psychiatric hospital settings. J Psychiatr Ment Health Nurs. 2009;16(3):225–315. doi:10.1111/j.1365-2850.2008.01355.x.
5.
World Health Organization. International classification of diseases for mortality and morbidity statistics (11th Revision). 2018. https://icd.who.int/browse11/l.... – 2020.10.20.
6.
Teraoka M, Kyougoku M. Structural relationships among occupational dysfunction, stress coping, and occupational participation for healthcare workers. Work. 2019;64(4):833–841. doi:10.3233/WOR-193045.
7.
Bean M. World may be short 5.7M nurses by 2030: 4 report takeaways. Becker’s Hospital Review. 2020. Retrieved from https://www.beckershospitalrev... orld-may-be-short-5–7m-nurses-by-2030-4-report-takeaways.html.
8.
Juczyński Z, Ogińska-Bulik N. Narzędzia pomiaru stresu i radzenia sobie ze stresem. Warszawa: Pracownia Testów Psychologicznych PTP; 2012.
9.
Juczyński Z. Narzędzia pomiaru w promocji psychologii zdrowia. Warszawa: Pracownia Testów Psychicznych PTP; 2012.
10.
Jaworowska A. LBQ kwestionariusz wypalenia zawodowego Massimo Satinello. Warszawa: Pracownia Testów Psychologicznych PTP; 2014.
11.
Humphries N, Morgan K, Conry MC, et al. Quality of care and health professional burnout: narrative literature review. Int J Health Care Qual Assur. 2014;27(4):293–307. doi:10.1108/IJHCQA-08-2012-0087.
12.
Gonczaryk A, Chmielewski JP, Strzelecka A, et al. Effect of selected factors related to emotions and general health on the health behaviours of paramedics. Ann Agric Environ Med. 2022;29(3):424–432. doi:10.26444/aaem/151531.
13.
Fuchs S, Endler PC, Mesenholl E, Paß P, Frass M. Burnout bei niedergelassenen Ärztinnen und Ärzten für Allgemeinmedizin. Wien Med Wochenschr. 2009;159(7–8):188–191. doi:10.1007/s10354-009-0669-5.
14.
Marques MM, Alves E, Queiros C, et al. The effect of profession on burnout in hospital staff. Occup Med. 2018;68(3):207–210. doi:10.1093/occmed/kqy039.
15.
Moukarzel A, Michalet P, Durand A-C, et al. Burnout Syndrome among Emergency Department Staff: Prevalence and Associated Factors. Biomed Res Int. 2019;2019:6462472. doi:10.1155/2019/6462472. eCollection 2019.
16.
Tarcan M, Hikmet N, Schooley B, et al. An analysis of the relationship between burnout, sociodemographic and workplace factors and job satisfaction among emergency department health professionals. Appl Nurs Res. 2017;34:40–47. doi:10.1016/j.apnr.2017.02.011. Epub 2017 Feb 3.
17.
Sende J, Jbeili C, Schvahn S. Facteurs de stress et consequences du stress en médecine d’urgence: enquête nationale. Ann Fr Med Urgence. 2012;2(4):224–231.
18.
Khireddine-Medouni I, Lemaître A, Homere J. La soufrance psychique en lien avec le travail chez les salariés actifs en France entre 2007 et 2012, à partir du programme MCP. Bull Epidémiol Hebd. 2015;23:431.
19.
Maslach C. Wypalenie w perspektywie wielowymiarowej. In: Sęk H, editor. Wypalenie zawodowe. Przyczyny i zapobieganie. Warszawa: Wydawnictwo Naukowe PWN; 2010.
21.
Makara-Studzińska M, Wontorczyk A, Izydorczyk B. Stress and occupational burnout in a population of Polish doctors – Organizationalprofessional and non-professional-social predictors. Ann Agric Environ Med. 2020;27(3):456–468. doi:10.26444/aaem/110846.
22.
Westbrook JI, Raban MZ, Walter SR, et al. Task errors by emergency physicians are associated with interruptions, multitasking, fatigue and working memory capacity: a prospective, direct observation study. BMJ Qual Saf. 2018;27(8):655–663. doi:10.1136/bmjqs-2017-007333.
23.
Gonczaryk A, Chmielewski JP, Strzelecka A, et al. Occupational hazards in the consciousness of the paramedic in emergency medical service. Disaster Emerg Med J. 2022;7(3):182–190. doi:10.5603/DEMJ.a2022.0031.
24.
Darban F, Balouchi A, Shahdadi H. Effect of communication skills training on the burnout of nurses: A cross-sectional study. J Clin Diagn Res. 2018;10(4):IC01–IC04. doi:10.7860/JCDR/2016/19312.7667.
25.
Saparniene D, Strukcinskiene B, Mineviciute G, et al. Working environment of health care professionals – focus on occupational stress. Ann Agric Environ Med. 2023;30(4):721–728. doi:10.26444/aaem/172116.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.