Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Social support as a moderator between the perception of the disease and stress level in lung cancer patients
1
John Paul II Catholic University, Lublin, Poland
Ann Agric Environ Med. 2020;27(4):630-635
KEYWORDS
TOPICS
ABSTRACT
Introduction:
Many studies attempt to explain the relationship between living in highly industrialized societies and the development of various diseases among people. Nowadays, the incidence of lung cancer is increasing worldwide. This is a highly stressful situation, both psychologically and physically. The study investigates the variable of social support and its moderating role between stress level and the perception of the disease among patients diagnosed with lung cancer.
Objective:
The aim of the study was to verify the hypothesis that there is a correlation between the subjective appraisal of one’s disease and the level of stress, as well as the hypothesis that social support is a moderator between the perception of the disease and stress level in patients diagnosed with lung cancer.
Material and methods:
The study involved 97 respondents diagnosed with lung cancer – 50 men and 47 women. The following methods were used for the study: the Disease-Related Appraisals Scale, the Disease-Related Social Support Scale, and the Perceived Stress Scale. Socio-demographic data were also collected.
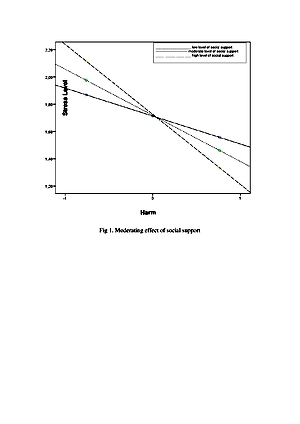
Results:
The results show that informational support may increase the level of perceived stress in lung cancer patients. It can be concluded that social support fulfils its moderating function in forming a stress response to cancer. A statistically significant moderating effect was observed of social support on the relationship between the appraisal of one’s disease as harmful and the stress level.
Conclusions:
The research findings demonstrate that social support plays a substantial role. It is important to diagnose the individual specific needs of lung cancer patients concerning the support they need.
Many studies attempt to explain the relationship between living in highly industrialized societies and the development of various diseases among people. Nowadays, the incidence of lung cancer is increasing worldwide. This is a highly stressful situation, both psychologically and physically. The study investigates the variable of social support and its moderating role between stress level and the perception of the disease among patients diagnosed with lung cancer.
Objective:
The aim of the study was to verify the hypothesis that there is a correlation between the subjective appraisal of one’s disease and the level of stress, as well as the hypothesis that social support is a moderator between the perception of the disease and stress level in patients diagnosed with lung cancer.
Material and methods:
The study involved 97 respondents diagnosed with lung cancer – 50 men and 47 women. The following methods were used for the study: the Disease-Related Appraisals Scale, the Disease-Related Social Support Scale, and the Perceived Stress Scale. Socio-demographic data were also collected.
Results:
The results show that informational support may increase the level of perceived stress in lung cancer patients. It can be concluded that social support fulfils its moderating function in forming a stress response to cancer. A statistically significant moderating effect was observed of social support on the relationship between the appraisal of one’s disease as harmful and the stress level.
Conclusions:
The research findings demonstrate that social support plays a substantial role. It is important to diagnose the individual specific needs of lung cancer patients concerning the support they need.
Poręba-Chabros A, Mamcarz P, Jurek K. Social support as a moderator between the perception of the disease and stress level in lung cancer
patients. Ann Agric Environ Med. 2020; 27(4): 630–635. doi: 10.26444/aaem/123099
REFERENCES (52)
1.
Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;.
2.
Zatoński WA, Sulkowska U, Didkowska J. Cancer epidemiology in Poland. Nowotwory J Oncol [Internet]. 2015; 65(3): 179–96. doi: 10.5603/NJO.2015.0041.
3.
Lin H-T, Liu F-C, Wu C-Y, Kuo C-F, Lan W-C, Yu H-P. Epidemiology and Survival Outcomes of Lung Cancer: A Population-Based Study. Domagala-Kulawik J, editor. Biomed Res Int [Internet]. 2019; 2019: 8148156. Available from: https://doi.org/10.1155/2019/8....
4.
Lee Y, Baek JM, Jeon YW, Im EO. Illness perception and sense of well-being in breast cancer patients. Patient Prefer Adherence. 2019; 13: 1557–1567. doi: 10.2147/PPA.S225561.
5.
Akbari S, Dortaj F, Ranjgar B, Akbari ME. The effect of personality, social support, and life events on overall survival in breast cancer. Int J Cancer Manag. 2019; 12(3): e83625. doi: 10.5812/ijcm.83625. doi: 10.4103/njcp.njcp_372_17.
6.
Ozbayir T, Gok F, Arican S, Koze B S, Uslu Y. Influence of demographic factors on perceived social support among adult cancer patients in Turkey. Niger J Clin Pract. 2019; 22: 1147–56.
7.
Leite MA, Nogueira DA, Terra Fde S. Evaluation of self-esteem in cancer patients undergoing chemotherapy treatment. Rev Lat Am Enfermagem. 2015; 23(6): 1082–1089. doi: 10.1590/0104-1169.0575.2652.
8.
Fitch MI. The Changing Face of Lung Cancer: Survivor Perspectives on Patient Engagement. Asia Pac J Oncol Nurs. 2019; 6(1): 17–23. doi: 10.4103/apjon.apjon_43_18.
9.
Applebaum AJ, Stein EM, Lord-Bessen J, Pessin H, Rosenfeld B, Breitbart W. Optimism, social support, and mental health outcomes in patients with advanced cancer. Psychooncology. 2014; 23(3): 299–306. doi: 10.1002/pon.3418.
10.
Daniela Berardo & Maria Valentina Mussa. Application of relational tool to support acute cardiac patients’ emotional recovery: analysis of effects during acute and follow-up care, International Journal of Qualitative Studies on Health and Well-being, 2019: 14: 1. doi: 10.1080/17482631.2019.1595957.
11.
Chan EA, Tsang PL, Ching SSY, Wong FY, Lam W. Nurses’ perspectives on their communication with patients in busy oncology wards: A qualitative study. PLoS ONE. 2019: 14(10): e0224178. doi: https://doi.org/10.1371/journa....
12.
Barre VP, Padmaja G, Saxena RK, Rana S. Impact of medical intervention on stress and quality of life in patients with cancer. Indian J Palliat Care. 2015; 21(2): 203–208. doi:10.4103/0973-1075.156503.
13.
Elsner K, Naehrig D, Halkett GKB, Dhillon HM. Reduced patient anxiety as a result of radiation therapist-led psychosocial support: a systematic review. J Med Radiat Sci. 2017; 64(3): 220–231. doi:10.1002/jmrs.208.
14.
Rizalar S, Ozbas A, Akyolcu N, Gungor B. Effect of perceived social support on psychosocial adjustment of Turkish patients with breast cancer. Asian Pacific Journal of Cancer Prevention: Apjcp. 2014; 15(8): 3429–3434. doi: 10.7314/APJCP.2014.15.8.3429.
15.
Peng X, Su Y, Huang W, Hu X. Status and factors related to posttraumatic growth in patients with lung cancer: A STROBE-compliant article. Medicine (Baltimore). 2019; 98(7): e14314. doi:10.1097/MD.0000000000014314.
16.
Trzmielewska W, Zięba M, Boczkowska M, Rak T, Wrześniowski S. Motivation of cancer patients to help others and the relation between posttraumatic growth and helping. Current Issues in Personality Psychology. 2019; 7(3): 232–241. doi: 10.5114/cipp.2019.86231.
17.
Yang N, Xiao H, Cao Y, Li S, Yan H, Wang Y. Influence of oncology nurses’ empathy on lung cancer patients’ cellular immunity. Psychol Res Behav Manag. 2018; 11: 279–287. Published 2018 Jul 31. doi: 10.2147/PRBM.S168649.
18.
Pourfallahi, Masoumeh, et al. The effect of informational-emotional support program on illness perceptions and emotional coping of cancer patients undergoing chemotherapy.” Supportive Care in Cancer. 2019: 1–11. doi: 10.1007/s00520-019-04842-w.
19.
Somasundaram RO, Devamani KA. A Comparative Study on Resilience, Perceived Social Support and Hopelessness Among Cancer Patients Treated with Curative and Palliative Care. Indian J Palliat Care. 2016; 22(2): 135–140. doi: 10.4103/0973-1075.179606.
20.
Leow, Kenneth, et al. Social Support, Basic Psychological Needs, and Social Well-Being Among Older Cancer Survivors. The International Journal of Aging and Human Development. Nov. 2019, doi: 10.1177/0091415019887688.
21.
Scrignaro M, Barni S, Magrin ME. The combined contribution of social support and coping strategies in predicting post-traumatic growth: a longitudinal study on cancer patients. Psycho-Oncology. 2011. 20(8): 823–831.
22.
Lee V, Cohen S, Edgar L. Meaning of making intervention during breast or colorectal cancer treatment improves self-esteem, optimism, and self-efficacy. Social Science & Medicine. 2006; 62(12): 3133–3145. https://doi.org/10.1016/j.socs....
23.
Hartley C, Coffee P. Perceived and Received Dimensional Support: Main and Stress-Buffering Effects on Dimensions of Burnout. Front Psychol. 2019; 10: 1724. Published 2019 Aug 2. doi: 10.3389/fpsyg.2019.01724.
24.
Lachowicz M, Raszeja S. Jakość życia pacjenta z rakiem płuc obiętych opieką paliatywną. Choroby XXI wieku – wyzwania w pracy fizjoterapeuty, edited by M. Podgórska. 2017; 233–251.
25.
Taniguchi A, Mizuno M. Psychological Stress and Coping in Recently Discharged Postsurgical Cancer Patients. Asia Pac J Oncol Nurs. 2016: 3(2): 176–182. doi: 10.4103/2347-5625.177394.
26.
Jafri SH, Ali F, Mollaeian A, et al. Major Stressful Life Events and Risk of Developing Lung Cancer: A Case-Control Study. Clin Med Insights Oncol. 2019; 13: 1179554919835798. Published 2019 May 1. doi: 10.1177/1179554919835798.
27.
Pękała M, Kozaka J. Jakość życia chorych na raka płuca. Psychoonkologia, 2016; 20(2): 90–97. doi: 10.5114/pson.2016.62058.
28.
Commodari E. Children staying in hospital: a research on psychological stress of caregivers. Ital J Pediatr. 2010; 36: 40. Published 2010 May 25. doi: 10.1186/1824-7288-36-40.
29.
Naughton MJ, Weaver KE. Physical and mental health among cancer survivors: considerations for long-term care and quality of life. N C Med J. 2014; 75(4): 283–286. doi:10.18043/ncm.75.4.283.
30.
Huss E, Samson T. Drawing on the Arts to Enhance Salutogenic Coping With Health-Related Stress and Loss. Front Psychol. 2018; 9: 1612. Published 2018 Sep 25. doi: 10.3389/fpsyg.2018.01612.
31.
Antoni MH. Psychosocial intervention effects on adaptation, disease course and biobehavioral processes in cancer. Brain Behav Immun. 2013; 30 Suppl(Suppl): S88–S98. doi: 10.1016/j.bbi.2012.05.009.
32.
Kupcewicz E, Olewińska J, Pikus H, Jóźwik M. Differentiating factors of mental adaptation to disease in women treated for gynaecological cancer. J Educ Heal Sport. 2017 Nov: 6;7. doi: 10.5281/zenodo.1041024.
33.
Shinan-Altman S, Werner P. Illness representations of dementia: a scoping review. Clin Interv Aging. 2019; 14: 179–193. Published 2019 Jan 18. doi: 10.2147/CIA.S193316.
34.
Janowski K, Steuden S, Kuryłowicz J, Nieśpiałowska-Steuden M. The Disease- Related Appraisals Scale: a tool to measure subjective perception of disease situation. In: K. Janowski, S. Steuden (ed.) Biopsychosocial Aspects of health and disease. Lublin. 2009; 1: 108–125. CPPP Scietific Press.
35.
Sirri L, Fava G, A, Sonino N: The Unifying Concept of Illness Behavior. Psychother Psychosom 2013; 82: 74–81. doi: 10.1159/000343508.
36.
Cipora E, Konieczny M, Sobieszczański J. Acceptance of illness by women with breast cancer. Ann Agric Environ Med. 2018; 25(1): 167–171. doi: 10.26444/aaem/75876.
37.
Smoleń E, Hombek K, Jarema M, Słysz M, Kalita K. Factors determining the acceptance of the disease in patients treated oncologically. Med Og Nauk Zdr. 2018; 24(1): 37–43. doi: 10.26444/monz/86142.
38.
Mazurek J, Lurbiecki J. Skala Akceptacji Choroby i jej znaczenie w praktyce klinicznej. Pol Merk Lek. 2014; 36(212): 106–108.
39.
Szymona-Pałkowska K, Janowski K, Pedrycz A, et al. Knowledge of the Disease, Perceived Social Support, and Cognitive Appraisals in Women with Urinary Incontinence. Biomed Res Int. 2016; 2016: 3694792. doi: 10.1155/2016/3694792.
40.
Amirifard N, Payandeh M, Aeinfar M, Sadeghi M, Sadeghi E, Ghafarpor S. A Survey on the Relationship between Emotional Intelligence and Level of Depression and Anxiety among Women with Breast Cancer. Int J Hematol Oncol Stem Cell Res. 2017; 11(1): 54–57.
41.
Janowski K, Tatala M, Jedynak T, Wałachowska K. Social support and psychosocial functioning in women after mastectomy. Palliative and Supportive Care. Cambridge University Press. 2019: 1–8. https://doi.org/10.1017/S14789....
42.
Ravindran OS, Shankar A, Murthy T. A Comparative Study on Perceived Stress, Coping, Quality of Life, and Hopelessness between Cancer Patients and Survivors. Indian J Palliat Care. 2019; 25(3): 414–420. doi: 10.4103/IJPC.IJPC_1_19.
43.
Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper].2012. Retrieved from http://www.afhayes.com/ public/process2012.pdf.
44.
Lauriola M, Tomai M. Biopsychosocial Correlates of Adjustment to Cancer during Chemotherapy: The Key Role of Health-Related Quality of Life. Merrick J, editor. Sci World J [Internet]. 2019; 2019: 9750940. https://doi.org/10.1155/2019/9....
45.
Shiozaki M, Hiraib K, Koyamac A, Inuid H, Yoshidae R, Tokorof A. Negative support of significant others affects psychological adjustment in breast cancer patients. Psychology and Health. 2011; 26(11): 1540–1551. doi: 10.1080/08870446.2010.551211.
46.
Perloff T, King JC, Rigney M, Ostroff JS, Johnson Shen M. Survivor guilt: The secret burden of lung cancer survivorship. J Psychosoc Oncol [Internet]. 2019 Sep 3; 37(5): 573–85. Available from: https://doi.org/10.1080/073473....
47.
Flanagan J, Holmes S. Social perceptions of cancer and their impacts: Implications for nursing practice arising from the literature. J Adv Nurs. 2000 Sep 1; 32: 740–9. doi: 10.1046/j.1365-2648.2000.01535.x.
48.
Song L, Son J, Lin N. Social Support. In: Handbook of Social Network Analyses. 2011. p. 116–28. doi: 10.4135/9781446294413.n9.
49.
Coob S. Social support as a moderator of life stress. Psychosomatic Medicine. 1976; 38: 300–314.
50.
Wu SM, Yang HC, Thayer JF, Andersen BL. Association of the physiological stress response with depressive symptoms in patients with breast cancer. Psychosom Med. 2014; 76(4): 252–256. doi: 10.1097/PSY.0000000000000060.
51.
Chou AF, Stewart SL, Wild RC, Bloom JR. Social support and survival in young women with breast carcinoma. Psychooncology. 2012; 21(2): 125–133. doi: 10.1002/pon.1863.
52.
Finck C, Barradas S, Zenger M, Hinz A. Quality of life in breast cancer patients: Associations with optimism and social support. Int J Clin Health Psychol. 2018; 18(1): 27–34. doi: 10.1016/j.ijchp.2017.11.002.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.