Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Relationship between SIBO and other bowel diseases and a common eating pattern for them. Part III
1
Department of Medical Anthropology, Institute of Rural Health, Lublin, Poland
2
Student of the Faculty of Medicine and Dentistry, Jagiellonian University Medical College, Kraków, Poland
3
Department of Epidemiology and Biostatistics, Institute of Rural Health, Lublin, Poland
4
Higher School of Health Promotion, Kraków, Poland
Corresponding author
Małgorzata Goździewska
Department of Medical Anthropology, Institute of Rural Health, Lublin, Jaczewskiego 2, 20-090, Lublin, Poland
Department of Medical Anthropology, Institute of Rural Health, Lublin, Jaczewskiego 2, 20-090, Lublin, Poland
Ann Agric Environ Med. 2024;31(3):322-328
KEYWORDS
therapyirritable bowel syndromeinflammatory bowel diseasessmall intestinal bacterial overgrowthdiet nutritional recommendations
TOPICS
ABSTRACT
Introduction and objective:
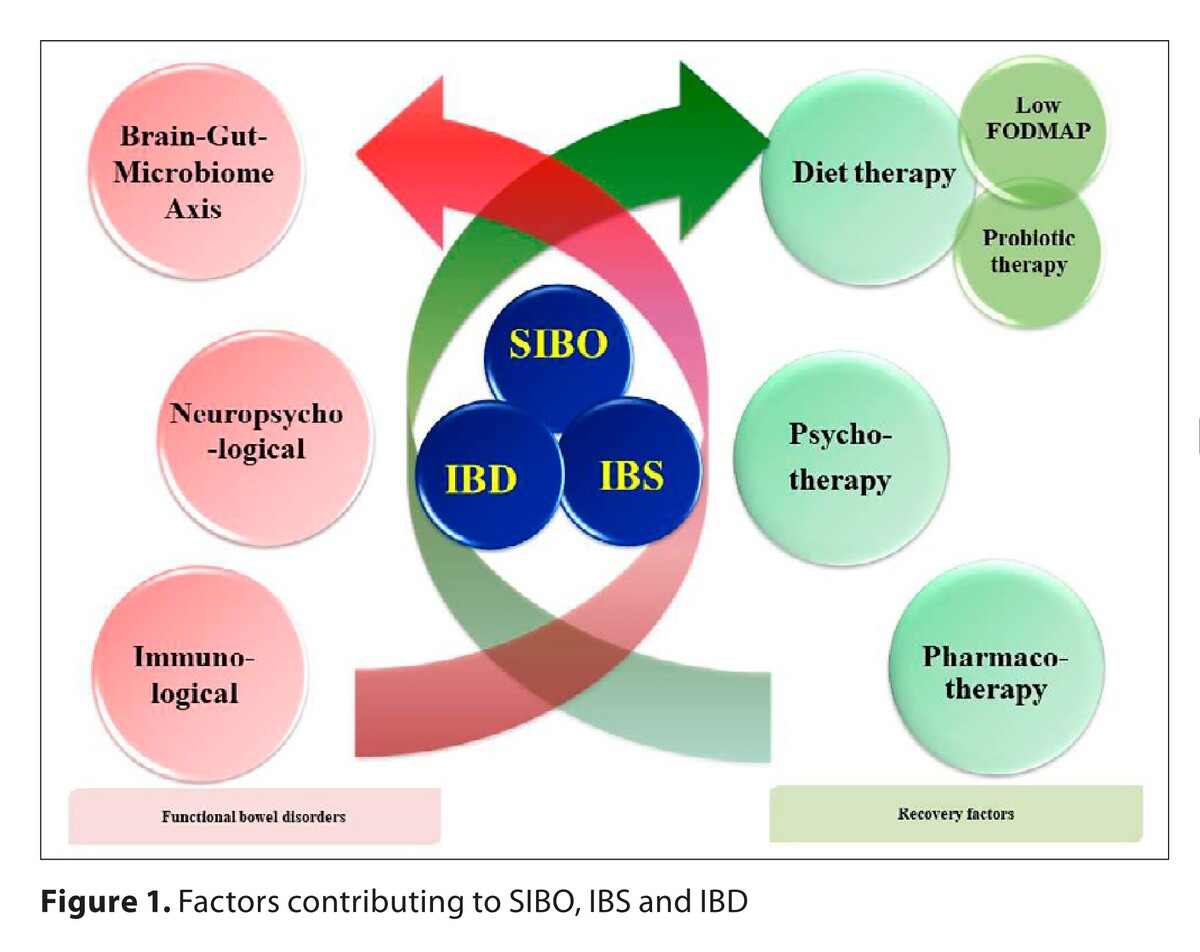
Conditions resulting from diseases of the brain-gut axis and gum-gut axis show many mutual, often bi-directional interrelationships. The accompanying quantitative and/or qualitative disorders of intestinal microflora may be effectively regulated by implementation of a properly adjusted diet therapy. The aim of the study is to investigate whether there is a relationship between small intestinal bacterial overgrowth (SIBO), and irritable bowel syndrome (IBS), and non-specific inflammatory bowel diseases (IBD), as well as indications for the mode of nutrition.
Review methods:
A literature review was performed using the databases PubMed, Google Scholar and Web of Science. A short synthesis of the collected information was made by a non-systematic literature review.
Brief description of the state of knowledge:
From the clinical point of view, SIBO is most often associated with IBS. Both conditions have common symptoms, such as: abdominal pain, flatulence bloating and diarrhea, as well as similar neuropsychological disorders. In turn, IBS have so many characteristics in common with IBD that the term IBS in IBD has even been proposed. Concerning diet therapy, a low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) is the most recommended diet. However, probiotic therapy is recommended to restore microbiological balance.
Summary:
At present, an increasing number of studies indicate a close relationship between SIBO and IBD, with SIBO occurring more often in patients suffering from Crohn’s disease than those with ulcerative colitis. In order to achieve good outcomes of treatment and prevent the recurrence of these diseases, interdisciplinary and inter-professional cooperation is required in the area of skilful, individualized combination of pharmacotherapy, psychotherapy, probiotic therapy, and diet therapy.
Conditions resulting from diseases of the brain-gut axis and gum-gut axis show many mutual, often bi-directional interrelationships. The accompanying quantitative and/or qualitative disorders of intestinal microflora may be effectively regulated by implementation of a properly adjusted diet therapy. The aim of the study is to investigate whether there is a relationship between small intestinal bacterial overgrowth (SIBO), and irritable bowel syndrome (IBS), and non-specific inflammatory bowel diseases (IBD), as well as indications for the mode of nutrition.
Review methods:
A literature review was performed using the databases PubMed, Google Scholar and Web of Science. A short synthesis of the collected information was made by a non-systematic literature review.
Brief description of the state of knowledge:
From the clinical point of view, SIBO is most often associated with IBS. Both conditions have common symptoms, such as: abdominal pain, flatulence bloating and diarrhea, as well as similar neuropsychological disorders. In turn, IBS have so many characteristics in common with IBD that the term IBS in IBD has even been proposed. Concerning diet therapy, a low FODMAP (fermentable oligosaccharides, disaccharides, monosaccharides and polyols) is the most recommended diet. However, probiotic therapy is recommended to restore microbiological balance.
Summary:
At present, an increasing number of studies indicate a close relationship between SIBO and IBD, with SIBO occurring more often in patients suffering from Crohn’s disease than those with ulcerative colitis. In order to achieve good outcomes of treatment and prevent the recurrence of these diseases, interdisciplinary and inter-professional cooperation is required in the area of skilful, individualized combination of pharmacotherapy, psychotherapy, probiotic therapy, and diet therapy.
REFERENCES (64)
1.
Goździewska M, Łyszczarz A, Kaczoruk M, Kolarzyk E. Relationship between periodontal diseases and non-specific inflammatory bowel diseases – an overview. Part I. Ann Agric Environ Med. 2024;31(1):1–7. doi: https://doi.org/10.26444/aaem/....
2.
Goździewska M, Łyszczarz A, Kaczoruk M, Kolarzyk E. Role of diet in primary and secondary prevention of periodontitis and non-specific inflammatory bowel diseases. Part II. Ann Agric Environ Med. 2024;31(2):170–177.
3.
Barbara G, Cremon C, Stanghellini V. Inflammatory Bowel Disease and Irritable Bowel Syndrome: Similarities and Differences. Curr Opin Gastroenterol. 2014;30:352–358. doi: 10.1097/MOG.0000000000000070.
4.
Ghoshal UC, Nehra A, Mathur A, Rai S. A meta-analysis on small intestinal bacterial overgrowth in patients with different subtypes of irritable bowel syndrome. J Gastroenterol Hepatol. 2020;35(6):922–931.
5.
Shah A, Talley NJ, Jones M, Kendall BJ, et al. Small Intestinal Bacterial Overgrowth in Irritable Bowel Syndrome: A Systematic Review and Meta-Analysis of Case-Control Studies. Am J Gastroenterol. 2020;115(2):190–201. doi: 10.14309/ajg.00000000000005042.
6.
Quigley EMM, Murray JA, Pimentel M. AGA Clinical Practice Update on Small Intestinal Bacterial Overgrowth: Expert Review. Gastroenterol. 2020;159:1526–1532.
7.
Ginnebaugh B, Chey WD, Saad R. Small intestinal bacterial overgrowth: how to diagnose and treat (and then treat again). Gastroenterol Clin North Am. 2020;49:571–587.
8.
Gomaa EZ. Human Gut Microbiota/Microbiome in Health and Diseases: A Review. Antonie Van Leeuwenhoek. 2020;113:2019–2040.
9.
Sroka N, Rydzewska-Rosołowska A, Kakareko K, Rosołowski M, Głowińska I, Hryszko T. Show Me What You Have Inside–The Complex Interplay between SIBO and Multiple Medical Conditions–A Systematic Review. Nutrients. 2022 Dec 24;15(1):90. doi:10.3390/nu15010090. PMID: 36615748; PMCID: PMC9824151.
10.
Losurdo G, Salvatore D’Abramo F, Indellicati G, Lillo C, Ierardi E, Di Leo A. The Influence of small intestinal bacterial overgrowth in digestive and extra-intestinal disorders. Int J Mol Sci. 2020;16:3531.
11.
Rao SSC, Bhagatwala J. Small Intestinal bacterial overgrowth: clinical features and therapeutic management. Clin Transl Gastroenterol. 2019;10:e00078.
12.
Oana K, Shimizu K, Takada T, Makino H, Yamazaki M, Katto M, et al. Manipulating the growth environment through co-culture to enhance stress tolerance and viability of probiotic strains in the gastrointestinal tract. Appl Environ Microbiol. 2023;89:e0150223. doi:10.1128/aem.01502-23.
13.
Daniluk J. Postępowanie w zespole rozrostu bakteryjnego jelita cienkiego. Omówienie wytycznych American College of Gastroenterology. 2020. Med Prakt. 2020;9:39–47.
14.
Goldenberg J, Nevitt B, Wentz A, Bradley R, Siebecker A. Hydrogen sulfide small intestinal bacterial overgrowth case registry. medRxiv. 2023–03.doi: https://doi.org/10.1101/2023.0....
15.
Khan MZ, Lyu R, McMichael J, Gabbard S. Chronic Intestinal Pseudo-Obstruction Is Associated with Intestinal Methanogen Overgrowth. Digestive Dis Sci. 2022;67(10):4834–4840. doi:10.1007/s10620-021-07343-1.
16.
Banaszak M, Górna I, Woźniak D, Przysławski J, Drzymała-Czyż S. Association between Gut Dysbiosis and the Occurrence of SIBO, LIBO, SIFO and IMO. Microorganisms, 2023;11(3):573.
17.
Tansel A, Levinthal DJ. Understanding our tests: hydrogen-methane breath testing to diagnose small intestinal bacterial overgrowth. Clin Translational Gastroenterol. 2022;10–14309.
18.
Kossewska J, Bierlit K, Trajkovski V. Personality, Anxiety, and Stress in Patients with Small Intestine Bacterial Overgrowth Syndrome. The Polish Preliminary Study. Int J Environ Res Public Health. 2022;20(1):93.
19.
Zafar H, Jimenez B, Schneider A. Small intestinal bacterial overgrowth: Current update. Curr Opinion Gastroenterol. 2023;39(6):522–528.
20.
Skrzydło-Radomańska B, Cukrowska B. How to Recognize and Treat Small Intestinal Bacterial Overgrowth? J Clin Med. 2022 Oct 12;11(20):6017. doi:10.3390/jcm11206017. PMID: 36294338; PMCID: PMC9604644.
21.
Redondo-Cuevas L, Belloch L, Martín-Carbonell V, Nicolás A, Alexandra I, Sanchis L, et al. Do Herbal Supplements and Probiotics Complement Antibiotics and Diet in the Management of SIBO? A Randomized Clinical Trial. Nutrients. 2024 Apr 7;16(7):1083. doi:10.3390/nu16071083. PMID: 38613116; PMCID: PMC11013329.
22.
Sorathia SJ, Chippa V, Rivas JM. Small Intestinal Bacterial Overgrowth. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/b....
23.
Mayer EA, Ryu HJ, Bhatt RR. The neurobiology of irritable bowel syndrome. Mol Psychiatry. 2023 Apr;28(4):1451–1465. doi:10.1038/s41380-023-01972-w. Epub 2023 Feb 2. PMID: 36732586; PMCID: PMC10208985.
24.
Szczepanek M, Goncerz G, Strzeszyński Ł. Choroby czynnościowe układu pokarmowego – wytyczne rzymskie IV (2016). Część III: Choroby czynnościowe jelit. Med Prakt. 2018;6:18–29.
25.
Hu Z, Li M, Yao L, Wang Y, Wang E, Yuan J, et al. The level and prevalence of depression and anxiety among patients with different subtypes of irritable bowel syndrome: a network meta-analysis. BMC Gastroenterol. 2021;21(1):1–18.5.
26.
Pimentel M, Lembo A. Microbiome and its role in irritable bowel syndrome. Digestive Dis Sci. 2020;65:829–839.
27.
Ndong PO, Boutallaka H, Marine-Barjoan E, Ouizeman D, Mroue R, et al. Prevalence of small intestinal bacterial overgrowth in irritable bowel syndrome (IBS): Correlating H2 or CH4 production with severity of IBS. JGH Open: an Open Access J Gastroenterol Hepatol. 2023;7(4):311.
28.
X.-W. DING, Y.-X. LIU, X.-C. FANG, K. LIU, Y.-Y. WEI, M.-H. SHAN. The relationship between small intestinal bacterial overgrowth and irritable bowel syndrome. Eur Rev Med Pharmacol Sci. 2017;21:5191–5196.
29.
Chuah KH, Wong MS, Tan PO, Lim SZ, Beh KH, Chong SCS, et al. Small Intestinal Bacterial Overgrowth In Various Functional Gastrointestinal Disorders: A Case-Control Study. Dig Dis Sci. 2022 Aug;67(8):3881–3889. doi:10.1007/s10620-021-07227-4. Epub 2021 Aug 21. PMID: 34417923.
30.
Petagna L, Antonelli A, Ganini C, Bellato V, Campanelli M, Divizia A, et al. Pathophysiology of Crohn’s disease inflammation and recurrence. Biology Direct. 2020;15(1):1–10.
31.
Segal JP, LeBlanc JF, Hart AL. Ulcerative colitis: an update. Clin Med. 2021;21(2):135.
32.
Andrei M, Gologan Ş. Small Intestinal Bacterial Overgrowth Syndrome Prevalence in Romanian Patients with Inflammatory Bowel Disease. Curr Health Sci J. 2016:151–156.
33.
Wanzl J, Gröhl K, Kafel A, Nagl S, Muzalyova A, Gölder SK. Impact of Small Intestinal Bacterial Overgrowth in Patients with Inflammatory Bowel Disease and Other Gastrointestinal Disorders—A Retrospective Analysis in a Tertiary Single Center and Review of the Literature. J Clin Med. 2023;12(3):935.
34.
Ghoshal UC, Yadav A, Fatima B, Agrahari AP, Misra A. Small intestinal bacterial overgrowth in patients with inflammatory bowel disease: A case-control study. Indian J Gastroenterol. 2022 Feb;41(1):96–103. doi:10.1007/s12664-021-01211-6. Epub 2021 Aug 14. PMID: 34390471.
35.
Bertges ER, Chebli JMF. Prevalence and factors associated with small intestinal bacterial overgrowth in patients with Crohn’s disease: a retrospective study at a referral center. Arq Gastroenterol. 2020;57:283–8.
36.
Pimentel M, Saad RJ, Long MD, et al. ACG Clinical Guideline: Small Intestinal Bacterial Overgrowth. Am J Gastroenterol. 2020;115:165–78.
37.
Wei J, Feng J, Chen L, Yang Z, Tao H, Li L, et al. Small intestinal bacterial overgrowth is associated with clinical relapse in patients with quiescet Crohn’s disease: a retrospective cohort study. Ann Transl Med. 2022;10(14):784. doi:10.21037/atm-22-3335.
38.
Yang C, Zhang X, Wang S, Huo X, Wang J. Small Intestinal Bacterial Overgrowth and Evaluation of Intestinal Barrier Function in Patients with Ulcerative Colitis. Am J Transl Res. 2021;13:6605–6610.
39.
Morrison M, Burger D, Martin N, Rich J, Jones M, Koloski N, et al. Systematic review with meta-analysis: the prevalence of small intestinal bacterial overgrowth in inflammatory bowel disease. Aliment Pharmacol Ther. 2019 Mar;49(6):624–635.
40.
Cohen-Mekelburg S, Tafesh Z, Coburn E, et al. Testing and Treating Small Intestinal Bacterial Overgrowth Reduces Symptoms in Patients with Inflammatory Bowel Disease. Dig Dis Sci. 2018;63:2439–2444. https://doi.org/10.1007/s10620....
41.
Ricci JER Júnior, Chebli LA, Ribeiro TCDR, et al. Small-Intestinal Bacterial Overgrowth is Associated With Concurrent Intestinal Inflammation But Not With Systemic Inflammation in Crohn’s Disease Patients. J Clin Gastroenterol. 2018;52:530–6.
42.
Kikut J, Konecka N, Ziętek M, et al. Diet supporting therapy for inflammatory bowel diseases. Eur J Nutr. 2021; 60: 2275–2291. https://doi.org/10.1007/s00394....
43.
Levine A, Rhodes JM, Lindsay JO, et al. Dietary Guidance From the International Organization for the Study of Inflammatory Bowel Diseases. Clin Gastroenterol Hepatol. 2020;18(6):1381–1392. doi:10.1016/j.cgh.2020.01.046.
44.
Gravina AG, Dallio M, Romeo M, et al. Adherence and effects derived from FODMAP diet on irritable bowel syndrome: a real life evaluation of a large follow-up observation. Nutrients. 2020;12:928. doi:10.3390/nu12040928.
45.
Pimentel M, Saad RJ, Long MD, Rao SSC, ACG Clinical Guideline: Small Intestinal Bacterial Overgrowth. Offcial J Am College Gastroenterol. 2020;115(2).
46.
Prince AC, Myers CE, Joyce T, Irving P, Lomer M, Whelan K. Fermentable Carbohydrate Restriction (Low FODMAP Diet) in Clinical Practice Improves Functional Gastrointestinal Symptoms in Patients with Inflammatory Bowel Disease. Inflamm Bowel Dis. 2016;22:1129–1136. doi:10.1097/MIB.0000000000000708.
47.
Bodini G, Zanella C, Crespi M, Lo Pumo S, Demarzo MG, Savarino E, et al. A randomized, 6-wk trial of a low FODMAP diet in patients with inflammatory bowel disease. Nutrition. 2019;67–68:110542. doi:10.1016/j.nut.2019.06.023.
48.
Melgaard D, Sørensen J, Riis J, Ovesen TS, Leutscher P, Sørensen S, et al. Efficacy of FODMAP Elimination and Subsequent Blinded Placebo-Controlled Provocations in a Randomised Controlled Study in Patients with Ulcerative Colitis in Remission and Symptoms of Irritable Bowel Syndrome: A Feasibility Study. Nutrients. 2022;14:1296. doi:10.3390/nu14061296.
49.
Szałwińska P, Włodarczyk J, Spinelli A, Fichna J, Włodarczyk, M. IBS-symptoms in IBD patients—Manifestation of concomitant or different entities. J Clin Med. 2020;10(1):31.
50.
Gibson PR, Halmos EP, So D, et al. Diet as a therapeutic tool in chronic gastrointestinal disorders: Lessons from the FODMAP journey. J Gastroenterol Hepatol. 2022;022. doi:https://doi.org/10.1111/jgh.15....
51.
McIntosh K, Reed DE, Schneider T, et al. FODMAPs alter symptoms and the metabolome of patients with IBS: A randomised controlled trial. Gut. 2017;66:1241–51.
52.
Chey WD, Hashash JG, Manning L, Chang L. AGA Clinical Practice Update on the Role of Diet in Irritable Bowel Syndrome: Expert Review. Gastroenterology 2022;22:S0016–5085(21)04084–1. doi:10.1053/j.gastro.2021.12.248.
53.
Simons M, Taft TH, Doerfler B, et al. Narrative review: Risk of eating disorders and nutritional deficiencies with dietary therapies for irritable bowel syndrome. Neurogastroenterol Motil. 2022;34(1):e14188. doi:10.1111/nmo.14188.
54.
Varney J, Barrett J, Scarlata K, et al. FODMAPs: food composition, defining cutoff values and international application. J Gastroenterol Hepatol. 2017;32 Suppl 1:53–61. doi:10.1111/jgh.13698.
55.
Wielgosz-Grochowska JP, Domanski N, Drywień ME. Efficacy of an Irritable Bowel Syndrome Diet in the Treatment of Small Intestinal Bacterial Overgrowth: A Narrative Review. Nutrients. 2022;14(16):3382. Published 2022 Aug 17. doi:10.3390/nu14163382.
56.
Vannoy J, Lucente M. Small Intestinal Bacterial Over-growth–Concepts and Considerations. Nutrit Foundations. 2021;1:1–7.
57.
Teigen LM, Geng Z, Sadowsky MJ, Vaughn BP, Hamilton MJ, Khoruts A. Dietary factors in sulfur metabolism and pathogenesis of ulcerative colitis. Nutrients. 2019;11(4):931.
58.
Ya WU, Jun YIN. Research progress of ketogenic diet regulating intestinal microbiome in the treatment of diseases. J Shanghai Jiao Tong University (Med Sci.), 2022;42(4):545.
59.
Hill C, Guarner F, Reid G, et al. Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11:506–514.
60.
So D, Quigley EMM, Whelan K. Probiotics in irritable bowel syndrome and inflammatory bowel disease: review of mechanisms and effectiveness. Curr Opinion Gastroenterol. 2023;39(2):103–109. doi:10.1097/MOG.0000000000000902.
61.
Staniszewski A, Kordowska-Wiater M. Probiotic Yeasts and How to Find Them—Polish Wines of Spontaneous Fermentation as Source for Potentially Probiotic Yeasts. Foods. 2023;12:3392. https://doi.org/10.3390/foods1....
62.
García-Collinot G, Madrigal-Santillán EO, Martínez-Bencomo MA, Carranza-Muleiro RA, Jara LJ, Vera-Lastra O, et al. Effectiveness of Saccharomyces Boulardii and Metronidazole for Small Intestinal Bacterial Overgrowth in Systemic Sclerosis. Dig Dis Sci. 2020;65:1134–1143. doi:10.1007/s10620-019-05830-0.
63.
Wielgosz-Grochowska JP, Domanski N, Drywień ME. Efficacy of an Irritable Bowel Syndrome Diet in the Treatment of Small Intestinal Bacterial Overgrowth: A Narrative Review. Nutrients. 2022;14(16):338.
64.
Satish Kumar L, Pugalenthi LS, Ahmad M, Reddy S, Barkhane Z, Elmadi J. Probiotics in irritable bowel syndrome: a review of their therapeutic role. Cureus. 2022;14:0.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.