Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
CASE REPORT
RAEB II type of myelodysplastic syndrome associated with axillary abscesses – Case Report
1
Department of Haematooncology and Bone Marrow Transplantation, Medical University, Lublin, Poland
Corresponding author
Adrian Juda
Department of Haematooncology and Bone Marrow Transplantation, Medical University in Lublin, Aleje Racławickie 1, 20-059, Lublin, Poland
Department of Haematooncology and Bone Marrow Transplantation, Medical University in Lublin, Aleje Racławickie 1, 20-059, Lublin, Poland
Ann Agric Environ Med. 2021;28(4):733-736
KEYWORDS
TOPICS
ABSTRACT
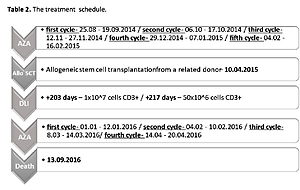
Myelodysplastic syndromes (MDS) are clonal haematopoetic stem cells disorders, characterized by bone marrow dysplasia, ineffecitive haematopoesis and cytopenias. Due to neutropenia, infections are common. A case is presented of a patient with high-risk myelodysplastic syndrome (MDS) complicated by hidradenitis suppurativa that developed in both axillae. Abscesses required multiple incisions and drainage. After five cycles of treatment with azacitidine, the patient underwent allogenic bone marrow transplantation. Unfortunately, six months after the procedure, the patient lost post-transplant chimerism.Treatment with azacitidine was re-started. After the subsequent ten months, blast transformation was observed. Skin lesions in the course of hidradenitis suppurative persisted and were still considerably active.
REFERENCES (19)
1.
Dwilewicz-Trojaczek J. Zespoły mielodysplastyczne (MDS). In: Interna Szczeklika. Mały podręcznik. 2017/2018 pod redakcją Piotra Gajewskiego. Kraków: Medycyna Praktyczna; 2017. 951–954.
2.
Leone G, Pagano L. Infections in Myelodysplastic Syndrome in relation to Stage and Therapy. Mediterr J Hematol Infect Dis. 2018; 10(1): e2018039.
3.
Dayyani F, Conley AP, Strom SS, et al. Cause of death in patients with lower – risk myelodysplastic syndrome. Cancer. 2010; 116(9): 2174–9.
4.
Greenberg PL, Stone RM, Al-Kali A, et al. Myelodysplastic Syndromes, Version 2. 2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc. 2017; 15(1): 60–67.
5.
Toma A, Fenaux P, Dreyfus F, Cordonnier C. Infections in Myelo–dysplastic Syndromes. Haematologica. 2012; 97: 1459–1470.
6.
Acquaviva C, Gelsi-Boyer V, Birnbaum D. Myelodysplastic syndromes: lost between two states? Leukemia. 2010; 24(1): 1–5.
7.
Magalhäes RF, Rivitti-Machedo MC, Duarte GV, et al. Consensus on the treatment of hidradenitis suppurativa-Brazilian Society of Dermatology. An Bras Dermatol. 2019 Mar-Apr; 94(2 Suppl 1): 7–19.doi: 10.1590/abd1806-4841.20198607.
8.
Salomon J, Piotrowska A, Matusiak Ł, et al. Chitinase – 3-like Protein 1(YKL-40) is expressed in lesional skin in hidradenitis suppurativa. In Vivo. 2019 Jab-Feb; 33(1): 141–143.
9.
Melnik BC, John SM, Chen W, Plewing G. T-helper 17 cell/regulatory T-cell imbalance in hidradenitis suppurativa (acne inversa): the link to hair follicle dissection, obesity, smoking and autoimmune comorbidities. Br J Dermatol. 2018; 179: 260–272.
10.
Kantarjian H, Issa JPJ, Rosenfeld CS, et al. Decitabine improves patient outcomes in myelodysplastic syndromes. Cancer. 2006; 106(8): 1794–1780.
11.
Fenaux P, Mufti JG, Hellstrom-Lindberg E, et al. Efficacy of azacitidine compared with that of conventional care regimens in the treatment of higher – risk myelodysplastic syndromes: a randomised, open-label, phase III study. Lancet Oncol. 2009; 10(3): 223–232.
12.
Merkel D, Filanovsky K, Aviv A, et al. Predictive parameters for infections during azacytidine therapy in high risk MDS patients American Society for Hematology Annual meeting 2011. San Diego. 2011.
13.
Trubiano JA, Dickinson M, Thursky KA, et al. Incidence, etiology and timing of infections following azacitidine therapy for myelodysplastic syndromes. Leuk Lymphoma. 2017; 58(10): 2379–2386.
14.
Drozd-Sokołowska J, Gil L, Waszczuk-Gajda A, et al. Azacitidine use after allogenic stem cell transplantation – results from the Polish Adult Leukemia Group. Transplant Proc. 2016; 48(5): 1802–1805.
15.
Fenaux P, Platzbecker U, Ades L. How we manage adults with myelodysplastic syndrome. Brit J Haematol. 2020; 189: 1016–1027.
16.
Zając M, Giannopoulos K. Znaczenie ekspresji nukleofosminy i jej mutacji w ostrej białaczce szpikowej. Acta Haematol Pol. 2011; 42(1): 63–73.
17.
Bains A, Luthra R, Medeiros Lj, Zuo Z. FLT3 and NPM1 mutations in myelodysplastic syndromes: Frequency and potential value for predicting progression to acute myeloid leukemia. Am J Clin Pathol. 2011; 135(1): 62–69.
18.
Bullen JJ, Rogers HJ, Spalding PB, Ward CG. Natural resistance, iron and infection: a challenge for clinical medicine. J Med Microbiol. 2006; 55(3): 251–258.
19.
Wong CAC, Wong SAY, Leitcg HA. Iron overload in lower international prognostic scoring system risk patients with myelodsyplastic syndrome receiving red blood cell transfusions: Relation to infections and possible benefit of iron chelation therapy. Leuk Res. 2018; Feb 10: 67: 75–81.doi: 10.1016/j.leukres.2018.02.005.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.