Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Perceived stress and burnout in nurses – the moderating role of age and network analysis perspective
1
The John Paul II Catholic University of Lublin, Lublin, Poland
2
University of Economics and Human Sciences in Warsaw, Warsaw, Poland
These authors had equal contribution to this work
Corresponding author
Małgorzata Tatala
The John Paul II Catholic University of Lublin, Al. Racławickie 14, 20-950 Lublin, Poland
The John Paul II Catholic University of Lublin, Al. Racławickie 14, 20-950 Lublin, Poland
Ann Agric Environ Med. 2025;32(1):85-97
KEYWORDS
Maslach Burnout Inventorynetwork analysisCOVID-19StressNursesBurnoutPerceived StressCoping StrategiesAge Moderation
TOPICS
ABSTRACT
Introduction and objective:
The primary focus of the study was to examine the relationship between stress and burnout among nurses during the COVID-19 pandemic, with a special emphasis on exploring the moderating impact of age. Building upon Cohen, Camarck and Mermelstein’s notion of perceived stress and Maslach’s comprehensive understanding of burnout, the research aimed to shed light on how these factors interact within the nursing profession.
Material and methods:
The research employed a cross-sectional approach, conducting an extensive analysis through online surveys with a substantial cohort of 463 nurses. Two measures were used: the Perceived Stress Scale (PSS-10) and Maslach Burnout Inventory (MBI).
Results:
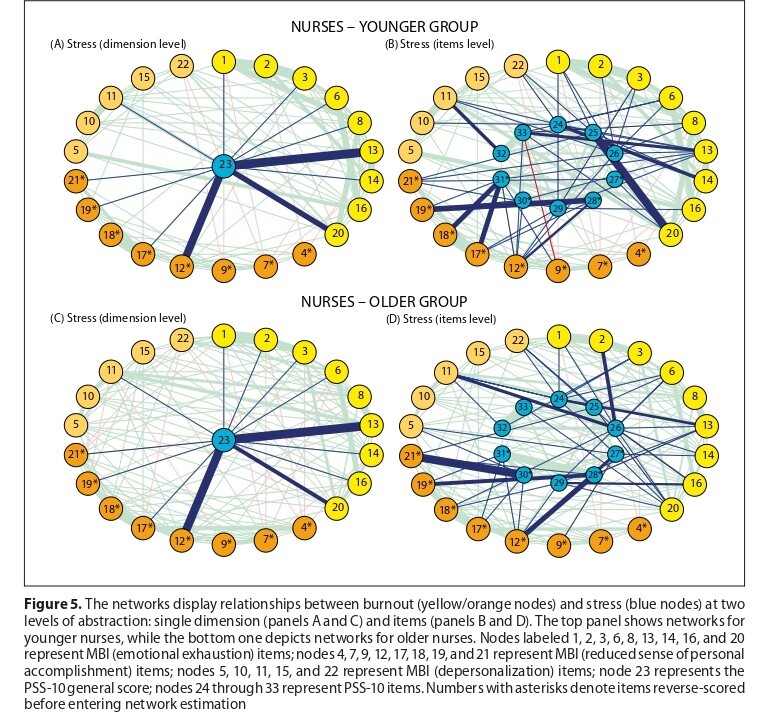
The results of the study confirmed a positive and notable link between stress and burnout across all identified dimensions. Notably, age emerged as a crucial moderator, demonstrating statistical significance, particularly in the area of reduced personal accomplishment. The moderating effect of age was most pronounced within the oldest age group, highlighting the nuanced role of age in influencing the stress-burnout dynamic among nurses. Additionally, network analysis revealed consistent connectivity between stress and burnout nodes across age cohorts, underscoring the robustness of these associations within the nursing population.
Conclusions:
The study confirmed the relationship between stress and burnout among nurses and highlights the moderating role of age, especially concerning reduced personal accomplishment. Urgent interventions are needed to equip nurses of all ages with coping strategies, particularly during challenging times like the COVID-19 pandemic.
The primary focus of the study was to examine the relationship between stress and burnout among nurses during the COVID-19 pandemic, with a special emphasis on exploring the moderating impact of age. Building upon Cohen, Camarck and Mermelstein’s notion of perceived stress and Maslach’s comprehensive understanding of burnout, the research aimed to shed light on how these factors interact within the nursing profession.
Material and methods:
The research employed a cross-sectional approach, conducting an extensive analysis through online surveys with a substantial cohort of 463 nurses. Two measures were used: the Perceived Stress Scale (PSS-10) and Maslach Burnout Inventory (MBI).
Results:
The results of the study confirmed a positive and notable link between stress and burnout across all identified dimensions. Notably, age emerged as a crucial moderator, demonstrating statistical significance, particularly in the area of reduced personal accomplishment. The moderating effect of age was most pronounced within the oldest age group, highlighting the nuanced role of age in influencing the stress-burnout dynamic among nurses. Additionally, network analysis revealed consistent connectivity between stress and burnout nodes across age cohorts, underscoring the robustness of these associations within the nursing population.
Conclusions:
The study confirmed the relationship between stress and burnout among nurses and highlights the moderating role of age, especially concerning reduced personal accomplishment. Urgent interventions are needed to equip nurses of all ages with coping strategies, particularly during challenging times like the COVID-19 pandemic.
REFERENCES (87)
1.
Selye H. Forty years of stress research: principal remaining problems and misconceptions. Can Med Assoc J. 1976;115(1):53–56.
2.
Fata L, Mootabi F, Bolhari J, Kazemzadeh Atoofi M. Stress management, guide of workshop education. Tehran Danjeh; 2008.
3.
Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer Publishing Company; 1984.
4.
Sharma P, Davey A, Davey S, Shukla A, Shrivastava K, Bansal R. Occupational stress among staff nurses: Controlling the risk to health. Indian J Occup Environ Med. 2014;18(2):52–56. doi:10.4103/0019-5278.146890.
5.
Poręba-Chabros A, Mamcarz P, Jurek K. Social support as a moderator between the perception of the disease and stress level in lung cancer patients. Ann Agric Environ Med. 2020;27(4):630–635. doi:10.26444/aaem/123099.
6.
Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–283. doi:10.1037/0022-3514.56.2.267.
7.
Wolfgang AP. Job Stress in the Health Professions: A Study of Physicians, Nurses, and Pharmacists. Behav Med. 1988;14(1):43–47. doi:10.1080/08964289.1988.9935123.
8.
Jordan TR, Khubchandani J, Wiblishauser M. The impact of perceived stress and coping adequacy on the health of nurses: A pilot investigation. Nurs Res Pract. 2016:5843256. https://www.hindawi.com/journa....
9.
Healy C, McKay M. Identifying sources of stress and job satisfaction in the nursing environment. Aust J Adv Nurs Q Publ R Aust Nurs Fed. 1999;17(2):30–35.
10.
Alshawush K, Hallett N, Bradbury-Jones C. The impact of transition programmes on workplace bullying, violence, stress and resilience for students and new graduate nurses: A scoping review. J Clin Nurs. 2022;31(17–18):2398–2417. doi:10.1111/jocn.16124.
11.
Janowski K, Tatala M, Jedynak T, Wałachowska K. Social support and psychosocial functioning in women after mastectomy. Palliat Support Care. 2020;18(3):314–321. doi:10.1017/S1478951519000774.
12.
Khamisa N, Oldenburg B, Peltzer K, Ilic D. Work related stress, burnout, job satisfaction and general health of nurses. Int J Environ Res Public Health. 2015;12(1):652–666. doi:10.3390/ijerph120100652.
13.
Pietrabissa G, Simpson SG. Psychological Consequences of Social Isolation During COVID-19 Outbreak. Front Psychol. 2020;11. https://www.frontiersin.org/ar....
14.
Dymecka J, Gerymski R, Machnik-Czerwik A. Fear of COVID-19 as a buffer in the relationship between perceived stress and life satisfaction in the Polish population at the beginning of the global pandemic. Health Psychol Rep. 2021;9(2):149–159. doi:10.5114/hpr.2020.102136.
15.
Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. 2020;88:901–907. doi:10.1016/j.bbi.2020.05.026.
16.
Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open. 2020;3:e203976. doi:10.1001/jamanetworkopen.2020.3976
17.
Lai S, Ruktanonchai NW, Zhou L, Prosper O, Luo W, Floyd JR, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020;585: 410–413. doi:10.1038/s41586-020-2293-x.
18.
Lu J, Gu J, Li K, Xu C, Su W, Lai Z, et al. COVID-19 Outbreak Associated with Air Conditioning in Restaurant, Guangzhou, China, 2020. Emerg Infect Dis. 2020;26:1628. doi:10.3201/eid2607.200764.
19.
Ruiz-Frutos C, Ortega-Moreno M, Allande-Cussó R, Domínguez-Salas S, Dias A, Gómez-Salgado J. Health-related factors of psychological distress during the COVID-19 pandemic among non-health workers in Spain. Saf Sci. 2021;133:104996. doi:10.1016/j.ssci.2020.104996.
20.
Ruiz-Frutos C, Ortega-Moreno M, Allande-Cussó R, Ayuso-Murillo D, Domínguez-Salas S, Gómez-Salgado J. Sense of coherence, engagement, and work environment as precursors of psychological distress among non-health workers during the COVID-19 pandemic in Spain. Saf Sci. 2021;133:105033. doi:10.1016/j.ssci.2020.105033.
21.
Ruiz-Frutos C, Ortega-Moreno M, Soriano-Tarín G, Romero-Martín M, Allande-Cussó R, Cabanillas-Moruno JL, et al. Psychological Distress Among Occupational Health Professionals During Coronavirus Disease 2019 Pandemic in Spain: Description and Effect of Work Engagement and Work Environment. Front Psychol. 2021;12. https://www.frontiersin.org/ar....
22.
Domínguez-Salas S, Gómez-Salgado J, Guillén-Gestoso C, Romero-Martín M, Ortega-Moreno M, Ruiz-Frutos C. Health care workers’ protection and psychological safety during the COVID-19 pandemic in Spain. J Nurs Manag. 2021;29(7):1924–1933. doi:10.1111/jonm.13331.
23.
Hendy A, Abozeid A, Sallam G, Abboud Abdel Fattah H, Ahmed Abdelkader Reshia F. Predictive factors affecting stress among nurses providing care at COVID-19 isolation hospitals at Egypt. Nurs Open. 2021;8(1):498–505. doi:10.1002/nop2.652.
24.
Maslach C. Maslach Burnout Inventory-Human Services Survey (MBI-HSS). MBI Man. 1996;192–198.
25.
Maslach C, Schaufeli WB, Leiter MP. Job Burnout. Annu Rev Psychol. 2001;52(1): 397–422. doi:10.1146/annurev.psych.52.1.397.
26.
Poghosyan L, Aiken LH, Sloane DM. Factor structure of the Maslach burnout inventory: an analysis of data from large scale cross-sectional surveys of nurses from eight countries. Int J Nurs Stud. 2009;46(7):894–902. doi:0.1016/j.ijnurstu.2009.03.004.
27.
Maslach C, Jackson SE. The measurement of experienced burnout. J Organ Behav. 1981;2(2):99–113. doi:10.1002/job.4030020205.
28.
Hreciński P. Polskie opracowanie krótkiej wersji Skali poczucia skuteczności nauczycielskiej (TSES) Tschannen-Moran i Woolfolk Hoy. Testy Psychol W Prakt Badaniach. 2016;1:19–35.
29.
Tucholska S. Wypalenie zawodowe u nauczycieli. Psychologiczna analiza zjawiska i jego osobowościowych uwarunkowań. Lublin: Wydawnictwo KUL; 2009.
30.
Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. 2020;16(1):1–11. doi:10.1186/s12992-020-00589-w.
31.
Baptista PCP, Lourenção DC de A, Silvestre Silva-Junior J, Cunha AA da, Gallasch CH. Distress and pleasure indicators in health care workers on the COVID-19 front line. Rev Lat Am Enfermagem. 2022;30:e3555. doi:10.1590/1518-8345.5707.3519.
32.
Teixeira K, Opolko C, Sussman T. I felt guilty [that] I didn’t do enough. Organizational and policy responses exacerbated frontline social worker distress. Can Soc Work Rev. 2022;39:63–80.
33.
Adriaenssens J, De Gucht V, Maes S. Determinants and prevalence of burnout in emergency nurses: A systematic review of 25 years of research. Int J Nurs Stud. 2015;52(2):649–661. doi:10.1016/j.ijnurstu.2014.11.004.
34.
Matsuishi Y, Mathis BJ, Masuzawa Y, Okubo N, Shimojo N, Hoshino H, et al. Severity and prevalence of burnout syndrome in paediatric intensive care nurses: A systematic review. Intensive Crit Care Nurs. 2021;67:103082. doi:10.1016/j.iccn.2021.103082.
35.
Wang J, Mao F, Wu L, Yang X, Zhang X, Sun Y, et al. Work-related potential traumatic events and job burnout among operating room nurses: Independent effect, cumulative risk, and latent class approaches. J Adv Nurs. 2022;78(7):2042–2054. doi:10.1111/jan.15114.
36.
Samir AlKudsi Z, Hany Kamel N, El-Awaisi A, Shraim M, Saffouh El Hajj M. Mental health, burnout and resilience in community pharmacists during the COVID-19 pandemic: A cross-sectional study. Saudi Pharm J. 2022;30(7):1009–1017. doi:10.1016/j.jsps.2022.04.015.
37.
Galanis P, Vraka I, Fragkou D, Bilali A, Kaitelidou D. Nurses’ burnout and associated risk factors during the COVID-19 pandemic: A systematic review and meta-analysis. J Adv Nurs. 2021;77(8):3286–3302. doi:10.1111/jan.14839.
38.
Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. EClinicalMedicine. 2020;24:100424. https://www.thelancet.com/jour....
39.
Bernier D. A study of coping: Successful recovery from severe burnout and other reactions to severe work-related stress. Work Stress. 1998;12(1): 50–65. doi:10.1080/02678379808256848.
40.
Schaufeli W, Enzmann D. The Burnout Companion To Study And Practice: A Critical Analysis. London: Taylor & Francis LTD; 1998.
42.
Dima G, Meseșan Schmitz L, Șimon M-C. Job Stress and Burnout among Social Workers in the VUCA World of COVID-19 Pandemic. Sustainability. 2021;13:7109. doi:10.3390/su13137109.
43.
Finney C, Stergiopoulos E, Hensel J, Bonato S, Dewa CS. Organizational stressors associated with job stress and burnout in correctional officers: a systematic review. BMC Public Health. 2013;13: 82. doi:10.1186/1471-2458-13-82.
44.
Weilenmann S, Ernst J, Petry H, Pfaltz MC, Sazpinar O, Gehrke S, et al. Health care workers’ mental health during the first weeks of the SARS-CoV-2 pandemic in Switzerland—a cross-sectional study. Front Psychiatry. 2021;12:594340. doi:10.3389/fpsyt.2021.594340.
45.
Cai H, Tu B, Ma J, Chen L, Fu L, Jiang Y, et al. Psychological Impact and Coping Strategies of Frontline Medical Staff in Hunan Between January and March 2020 During the Outbreak of Coronavirus Disease 2019 (COVID-19) in Hubei, China. Med Sci Monit Int Med J Exp Clin Res. 2020;26:e924171-1–e924171-16. doi:10.12659/MSM.924171.
46.
Walesa C, Tatala M, Rydz E. Rozwój religijności człowieka. Tom III: Osoba dorosła. Lublin: Wydawnictwo KUL; 2023.
47.
Tatala M. The role of personal adjustment to developmental crises in improving quality of life. Int J Psychol Couns. 2009;10:187–193.
48.
Tatala M, Wojtasiński M, Janowski K. Loneliness and time abroad in Polish migrants in the UK: Protective role of religious experience. Plos One. 2023;18(2):e0279984. doi:10.1371/journal.pone.0279984.
49.
Tatala M. Psychological aspects of religious morality in middle and late adulthood. Kwart Nauk Fides Ratio. 2021;48(4):147–160. doi:10.34766/fetr.v48i4.941.
50.
Pala AN, Chuang JC, Chien A, Krauth DM, Leitner SA, Okoye NM, et al. Depression, anxiety, and burnout among hospital workers during the COVID-19 pandemic: A cross-sectional study. Plos One. 2022;17(12):e0276861. doi:10.1371/journal.pone.0276861.
51.
Janowski K, Tatala M, Jedynak T, Księżpolska A, Głowacka B. Wsparcie społeczne a ocena własnej choroby, nasilenie objawów depresyjnych i akceptacja życia z chorobą u kobiet po mastektomii. 2016;21(2):188–205. https://repozytorium.ukw.edu.p....
52.
Walesa C, Tatala M. Rozwój religijności człowieka. Tom II: Młodzież. Lublin: Wydawnictwo KUL; 2020.
53.
Tatala M. Ocena stresu wywołanego traumatycznym zdarzeniem w grupie ratowników medycznych i strażaków: przyczynek do rozumienia kultury pracy. Rocz Kult. 2022;13(3):35–55. doi:10.18290/rkult22133.2.
54.
Wałachowska K, Janowski K, Tatala M. The efficacy of three interventions modifying stereotypes and prejudice towards people with schizophrenia. Pol Psychol Bull. 2009; 40(4):251–257. doi:10.2478/s10059-009-0020-4.
55.
Xie C, Li X, Zeng Y, Hu X. Mindfulness, emotional intelligence and occupational burnout in intensive care nurses: A mediating effect model. J Nurs Manag. 2021;29(3):535–542. doi:10.1111/jonm.13193.
56.
Silverstein M, Giarrusso R. Aging and Family Life: A Decade Review. J Marriage Fam. 2010;72(5):1039–1058. doi:10.1111/j.1741-3737.2010.00749.x.
57.
Turnipseed DL. An Analysis of the Influence of Work Environment Variables and Moderators on the Burnout Syndrome. J Appl Soc Psychol. 1994;24(9):782–800. doi:10.1111/j.1559-1816.1994.tb00612.x.
58.
Akman O, Ozturk C, Bektas M, Ayar D, Armstrong MA. Job satisfaction and burnout among paediatric nurses. J Nurs Manag. 2016;24(7):923–933. doi:10.1111/jonm.12399.
59.
Schooley B, Hikmet N, Tarcan M, Yorgancioglu G. Comparing burnout across emergency physicians, nurses, technicians, and health information technicians working for the same organization. Medicine (Baltimore). 2016;95(10):e2856. https://www.ncbi.nlm.nih.gov/p....
60.
Zheng X, Qin X, Liu X, Liao H. Will creative employees always make trouble? Investigating the roles of moral identity and moral disengagement. J Bus Ethics. 2019;157:653–672. doi:10.1007/s10551-017-3683-3.
61.
Borsboom D, Van Der Maas HLJ, Dalege J, Kievit RA, Haig BD. Theory Construction Methodology: A Practical Framework for Building Theories in Psychology. Perspect Psychol Sci. 2021;16(4):756–766. doi:10.1177/1745691620969647.
62.
Epskamp S, Borsboom D, Fried EI. Estimating psychological networks and their accuracy: A tutorial paper. Behav Res Methods. 2018;50:195–212. doi:10.3758/s13428-017-0862-1.
64.
LeBeau B. Simglm: Simulate models based on the generalized linear model. R package version 0.8; 2022.
65.
Green P, MacLeod CJ, Alday P. Package ‘simr.’ R Package See Httpscran R-Proj Orgwebpackagessimr. 2016. https://ftp.acc.umu.se/mirror/....
66.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. https://www.jstor.org/stable/2....
67.
Ogińska-Bulik N, Juczyński Z. Type D personality in Poland: Validity and application of the Polish DS14. Pol Psychol Bull. 2009; 40(3):130–136. doi: 10.2478/s10059-009-0029-8 2009.
68.
Pasikowski T. Polish adaptation of Maslach Burnout Inventory questionnaire. In: Sęk H, editor. Occupational burnout. Causes. Mechanisms. Prevention. Warsaw. Polish Scientific Publishers PWN. 2006;13–31:135–148.
69.
Johnson PO, Fay LC. The Johnson-Neyman technique, its theory and application. Psychometrika. 1950;15(4):349–367. doi:10.1007/BF02288864.
70.
Burger J, Isvoranu A-M, Lunansky G, Haslbeck JMB, Epskamp S, Hoekstra RHA, et al. Reporting standards for psychological network analyses in cross-sectional data. Psychol Methods. 2023;28(4):806–824. doi:10.1037/met0000471.
71.
Epskamp S, Cramer AOJ, Waldorp LJ, Schmittmann VD, Borsboom D. qgraph: Network Visualizations of Relationships in Psychometric Data. J Stat Softw. 2012;48(4). doi:10.18637/jss.v048.i04.
72.
Epskamp S, Fried EI. A Tutorial on Regularized Partial Correlation Networks. Psychol Methods. 2018;23(4):617–634. doi:10.1037/met0000167.
73.
Van Borkulo CD, Van Bork R, Boschloo L, Kossakowski JJ, Tio P, Schoevers RA, et al. Comparing network structures on three aspects: A permutation test. Psychol Methods. 2023;28(6):1273–1285. doi:10.1037/met0000476.
74.
Haslbeck JMB, Waldorp LJ. How well do network models predict observations? On the importance of predictability in network models. Behav Res Methods. 2018;50:853–861. doi:10.3758/s13428-017-0910-x.
75.
Yarkoni T, Westfall J. Choosing Prediction Over Explanation in Psychology: Lessons From Machine Learning. Perspect Psychol Sci. 2017;12(6):1100–1122. doi:10.1177/1745691617693393.
76.
Shah MK, Gandrakota N, Cimiotti JP, Ghose N, Moore M, Ali MK. Prevalence of and factors associated with nurse burnout in the US. JAMA Netw Open. 2021;4(2):e2036469. doi:10.1001/jamanetworkopen.2020.36469.
77.
Gómez-Urquiza JL, Vargas C, De la Fuente EI, Fernández-Castillo R, Cañadas-De la Fuente GA. Age as a Risk Factor for Burnout Syndrome in Nursing Professionals: A Meta-Analytic Study. Res Nurs Health. 2017;40(2):99–110. doi:10.1002/nur.21774.
78.
Zeng LN, Zhang JW, Zong QQ, Chan SW, Browne G, Ungvari GS, et al. Prevalence of burnout in mental health nurses in China: A meta-analysis of observational studies. Arch Psychiatr Nurs. 2020;34(3):141–148. doi:10.1016/j.apnu.2020.03.006.
79.
Zhang Y, Wang C, Pan W, Zheng J, Gao J, Huang X, et al. Stress, burnout, and coping strategies of frontline nurses during the COVID-19 epidemic in Wuhan and Shanghai, China. Front Psychiatry. 2020;11:565520. doi:10.3389/fpsyt.2020.565520.
80.
Yao Y, Yao W, Wang W, Li H, Lan Y. Investigation of risk factors of psychological acceptance and burnout syndrome among nurses in China: Acceptance and burnout in nurses. Int J Nurs Pract. 2013;19(5): 530–538. doi:10.1111/ijn.12103.
81.
Cohen S, Kamarck T, Mermelstein R. Perceived stress scale. Meas Stress Guide Health Soc Sci. 1994;10(2):1–2.
82.
Mefoh PC, Ude EN, Chukwuorji JC. Age and burnout syndrome in nursing professionals: moderating role of emotion-focused coping. Psychol Health Med. 2019;24(1):101–107. doi:10.1080/13548506.2018.1502457.
83.
Murat M, Köse S, Savaşer S. Determination of stress, depression and burnout levels of front-line nurses during the COVID-19 pandemic. Int J Ment Health Nurs. 2021;30(2): 533–543. doi:10.1111/inm.12818.
84.
Huang L, Caspari JH, Sun X, Thai J, Li Y, Chen F, et al. Risk and protective factors for burnout among physicians from standardized residency training programs in Shanghai: a cross-sectional study. BMC Health Serv Res. 2020;20:965. doi:10.1186/s12913-020-05816-z.
85.
Gózd-Barszczewska AI, Panasiuk L. Częstość występowania modyfikowalnych czynników ryzyka chorób układu sercowo-naczyniowego w grupie pacjentów hospitalizowanych z powodu objawowej choroby wieńcowej w regionie lubelskim. Med Og Nauk Zdr. 2021;27(4):453–560. doi:10.26444/monz/144082.
86.
Strzemecka J, Goździewska M, Skrodziuk J, Galińska EM, Lachowski S. Factors of work environment hazardous for health in opinions of employees working underground in the ‘Bogdanka’coal mine. Ann Agric Environ Med. 2019;26(3):409–414. doi:10.26444/aaem/106224.
87.
Wisłowska M, Kanecki K, Tyszko P, Kapała A. Jakość życia zależna od zdrowia u pacjentów z reumatoidalnym zapaleniem stawów. Reumatologia. 2010;48(2):104-111.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.