Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
New insights into the socio-economic aspects of multiple sclerosis in a cohort of Polish patients
1
Department of Neurology, 10th Military Research Hospital and Polyclinic, Bydgoszcz, Poland
2
Department of Hygiene, Epidemiology and Ergonomy, Nicolaus Copernicus University, Torun, Poland
3
Department of Ophthalmology, 10th Military Research Hospital and Polyclinic, Bydgoszcz, Poland
4
Institute of Cellular Medicine, Newcastle University, United Kingdom
Corresponding author
Łukasz Rzepiński
Department of Neurology, 10th Military Research Hospital and Polyclinic, Bydgoszcz, Poland
Department of Neurology, 10th Military Research Hospital and Polyclinic, Bydgoszcz, Poland
Ann Agric Environ Med. 2021;28(1):99-106
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
The diagnosis of multiple sclerosis (MS) affects the socio-economic aspects of patients’ lives and poses new challenges. The objectives of the study were: 1) to determine selected socio-economic aspects of MS in Poland in relation to the disease type and patients’ place of residence, and 2) to evaluate the profile of patients via the MS Society (MSS) and the occupational consequences of informing an employer about the diagnosis.
Material and methods:
A retrospective, observational study was undertaken to assess a cohort of 375 Polish MS patients. Socio-economic data was collected based on the patients’ responses to questions on a questionnaire. Clinical data was obtained from available medical records.
Results:
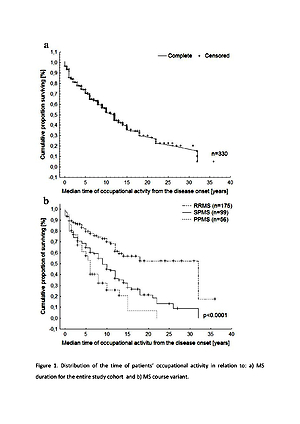
Patients with relapsing-remitting MS had a significantly longer time of occupational activity, higher economic status, higher level of education, better relationships with life partner, less likely to benefit from disability benefits, and members of MSS, than patients with progressive types of the disease. The patients living in rural areas had a significantly shorter time of occupational activity, more often experienced a decrease in income, received disability pension, and were less educated than urban residents. Patients who informed their employer about an MS diagnosis significantly more often received support from the company, were professionally active for longer, and less likely to experience a decrease in income. Membership of the MSS were dominated by patients with progressive variants of the disease and advanced disability.
Conclusions:
The disease variant and, to a lesser extent, the place of residence, affected the socio-economic aspects of MS. It might be advantageous for the patient to disclose information about MS diagnosis to the employer.
The diagnosis of multiple sclerosis (MS) affects the socio-economic aspects of patients’ lives and poses new challenges. The objectives of the study were: 1) to determine selected socio-economic aspects of MS in Poland in relation to the disease type and patients’ place of residence, and 2) to evaluate the profile of patients via the MS Society (MSS) and the occupational consequences of informing an employer about the diagnosis.
Material and methods:
A retrospective, observational study was undertaken to assess a cohort of 375 Polish MS patients. Socio-economic data was collected based on the patients’ responses to questions on a questionnaire. Clinical data was obtained from available medical records.
Results:
Patients with relapsing-remitting MS had a significantly longer time of occupational activity, higher economic status, higher level of education, better relationships with life partner, less likely to benefit from disability benefits, and members of MSS, than patients with progressive types of the disease. The patients living in rural areas had a significantly shorter time of occupational activity, more often experienced a decrease in income, received disability pension, and were less educated than urban residents. Patients who informed their employer about an MS diagnosis significantly more often received support from the company, were professionally active for longer, and less likely to experience a decrease in income. Membership of the MSS were dominated by patients with progressive variants of the disease and advanced disability.
Conclusions:
The disease variant and, to a lesser extent, the place of residence, affected the socio-economic aspects of MS. It might be advantageous for the patient to disclose information about MS diagnosis to the employer.
REFERENCES (45)
1.
Wynia K, Middel B, van Dijk JP, de Keyser JH, Reijneveld SA. The impact of disabilities on quality of life of people with multiple sclerosis. Multiple Sclerosis 2008; 14: 972–980.
2.
Montalban X, Gold R, Thompson AJ, Otero-Romero S, Amato MP, Chandraratna D, et al. ECTRIMS/EAN Guideline on the pharmacological treatment of people with multiple sclerosis. Mult Scler. 2018 Feb; 24(2): 96–120. doi: 10.1177/1352458517751049.
3.
Dobson R, Giovannoni G. Multiple sclerosis – a review. Eur J Neurol. 2019 Jan; 26(1): 27–40. doi: 10.1111/ene.13819.
4.
Nobles J, Weintraub MR, Adler NE. Subjective socioeconomic status and health: relationships reconsidered. Soc Sci Med. 2013; 82: 58–66. doi:10.1016/j.socscimed.2013.01.021.
5.
Laskowska I. Availability of health services vs. health condition of residents of rural areas in Poland – Analysis performed on the basis of EHIS 2009. Ann Agric Environ Med. 2015; 22(4): 700–703. doi: 10.5604/12321966.1185779.
6.
Briggs FBS, Thompson NR, Conway DS. Prognostic factors of disability in relapsing remitting multiple sclerosis. Mult Scler Relat Disord. 2019 May; 30: 9–16. doi: 10.1016/j.msard.2019.01.045.
7.
Crielaard L, Kavaliunas A, Ramanujam R, Olsson T, Hillert J, Stridh P, et al. Factors associated with and long-term outcome of benign multiple sclerosis: a nationwide cohort study. J Neurol Neurosurg Psychiatry. 2019 Jul; 90(7): 761–767. doi: 10.1136/jnnp-2018-319913.
8.
Harding KE, Wardle M, Carruthers R, Robertson N, Zhu F, Kingwell E, et al. Socioeconomic status and disability progression in multiple sclerosis: A multinational study. Neurology. 2019 Mar 26; 92(13): e1497-e1506. doi: 10.1212/WNL.0000000000007190.
9.
Pfleger CC, Flachs EM, Koch-Henriksen N. Social consequences of multiple sclerosis. Part 2. Divorce and separation: a historical prospective cohort study. Mult Scler. 2010; 16(7): 878–82.
10.
Salter A, Thomas N, Tyry T, Cutter G, Marrie RA. Employment and absenteeism in working-age persons with multiple sclerosis. J Med Econ. 2017 May; 20(5): 493–502. doi: 10.1080/13696998.2016.1277229.
11.
Fantoni-Quinton S, Kwiatkowski A, Vermersch P, Roux B, Hautecoeur P, Leroyer A. Impact of multiple sclerosis on employment and use of job-retention strategies: The situation in France in 2015. J Rehabil Med. 2016 Jun 13; 48(6): 535–40. doi: 10.2340/16501977-2093.
12.
Persechino B, Fontana L, Buresti G, Fortuna G, Valenti A, Iavicoli S. Improving the job-retention strategies in multiple sclerosis workers: the role of occupational physicians. Ind Health. 2019; 57(1): 52–69. doi:10.2486/indhealth.2017-0214.
13.
GBD 2016 Multiple Sclerosis Collaborators. Global, regional, and national burden of multiple sclerosis 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019; 18(3): 269–285. doi:10.1016/S1474-4422(18)30443-5.
14.
Pantyley V. Health inequalities among rural and urban population of Eastern Poland in the context of sustainable development. Ann Agric Environ Med. 2017; 24(3): 477–483. doi: 10.5604/12321966.1233905.
15.
Krzyżak M, Maślach D, Szpak A, Piotrowska K, Florczyk K, Skrodzka M, et al. Trends of potential years of life lost due to main causes of deaths in urban and rural population in Poland, 2002–2011. Ann Agric Environ Med. 2015; 22(3): 564–571.
16.
Gong G, Phillips SG, Hudson C, Curti D, Philips BU. Higher US Rural Mortality Rates Linked To Socioeconomic Status, Physician Shortages, And Lack Of Health Insurance. Health Aff (Millwood). 2019 Dec; 38(12): 2003–2010. doi: 10.1377/hlthaff.2019.00722.
17.
Joseph G, da Silva ICM, Barros AJD, Victora CG. Socioeconomic inequalities in access to skilled birth attendance among urban and rural women in low-income and middle-income countries. BMJ Glob Health. 2018; 3(6): e000898. doi:10.1136/bmjgh-2018-000898.
18.
Poser CM, Paty DW, Scheinberg L, McDonald WI, Davis FA, Ebers GC, et al. New diagnostic criteria for multiple sclerosis: Guidelines for research protocols. Ann Neurol. 1983; 13: 227–231.
19.
McDonald WI, Compston A, Edan G, Goodkin D, Hartung HP; Lublin FD, et al. Recommended diagnostic criteria for multiple sclerosis: Guidelines from the International Panel on the diagnosis of multiple sclerosis. Ann. Neurol. 2001; 50: 121–127.
20.
Polman CH, Reingold SC, Edan G, Filippi M, Hartung HP, Kappos L, et al. Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol. 2005; 58: 840–846.
21.
Polman CH, Reingold SC, Banwell B, Clanet M, Cohen JA, Filippi M, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011; 69: 292–302.
22.
Weinshenker BG, Bass B, Rice GP, Noseworthy J, Carriere W, Baskerville J, et al. The natural history of multiple sclerosis: a geographically based study. I. Clinical course and disability. Brain. 1989; 112: 133–146.
23.
Lublin FD, Reingold SC. Defining the clinical course of multiple sclerosis: results of an international survey. National Multiple Sclerosis Society (USA) Advisory Committee on Clinical Trials of New Agents in Multiple Sclerosis. Neurology. 1996 Apr; 46(4): 907–11.
24.
Leray E, Yaouanq J, Le Page E, Coustans M, Laplaud D, Oger J, et al. Evidence for a two-stage disability progression in multiple sclerosis. Brain. 2010; 133: 1900–1913.
25.
Scalfari A, Neuhaus A, Degenhardt A, Rice GP, Muraro PA, Daumer M, et al. The natural history of multiple sclerosis: a geographically based study 10: relapses and long-term disability. Brain. 2010 Jul; 133(Pt 7): 1914–29.
26.
Kurtzke JF. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology. 1983; 33: 1444–1452.
27.
Rzepiński Ł, Zawadka-Kunikowska M, Maciejek Z, Newton J, Zalewski P. Early Clinical Features, Time to Secondary Progression, and Disability Milestones in Polish Multiple Sclerosis Patients. Medicina (Kaunas). 2019 May 31; 55(6). pii: E232. doi: 10.3390/medicina55060232.
29.
Pierzchala K, Adamczyk-Sowa M, Dobrakowski P, Kubicka-Baczyk K, Niedziela N, Sowa P. Demographic characteristics of MS patients in Poland’s upper Silesia region. Int J Neurosci. 2015; 125(5): 344–51.
30.
Jaracz K, Pawlak M, Górna K, Kołcz B, Wołoszyn D, Kozubski W. Quality of life and social support in patients with multiple sclerosis. Neurol Neurochir Pol. 2010; 44(4): 358–65.
31.
Cai J, Coyte PC, Zhao H. Decomposing the causes of socioeconomic-related health inequality among urban and rural populations in China: a new decomposition approach. Int J Equity Health. 2017; 16(1): 128. doi:10.1186/s12939-017-0624-9.
32.
Dorjdagva J, Batbaatar E, Dorjsuren B, Kauhanen J. Explaining differences in education-related inequalities in health between urban and rural areas in Mongolia. Int J Equity Health. 2015; 14: 154. doi:10.1186/s12939-015-0281-9.
34.
Brola W, Fudala M, Flaga S, Ryglewicz D, Potemkowski A. Polski rejestr chorych na stwardnienie rozsiane – stan obecny, perspektywy i problemy. Aktualn Neurol. 2015; 15(2): 68–73.
35.
Koopman WJ, Benbow CL, Vandervoort M. Top 10 needs of people with multiple sclerosis and their significant others. J Neurosci Nurs. 2006; 38: 369–373.
36.
Koziarska D, Król J, Nocoń D, Kubaszewski P, Rzepa T, Nowacki P. Prevalence and factors leading to unemployment in MS (multiple sclerosis) patients undergoing immunomodulatory treatment in Poland. PLoS One. 2018; 13(4): e0194117. doi:10.1371/journal.pone.0194117.
37.
Wiberg M, Murley C, Tinghög P, Alexanderson K, Palmer E, Hillert J, et al. Earnings among people with multiple sclerosis compared to references, in total and by educational level and type of occupation: a population-based cohort study at different points in time. BMJ Open. 2019; 9(7): e024836. doi:10.1136/bmjopen-2018-024836.
38.
Castelo-Branco A, Landfeldt E, Svedbom A, Löfroth E, Kavaliunas A, Hillert J. Clinical course of multiple sclerosis and labour-force absenteeism: a longitudinal population-based study. Eur J Neurol. 2019 Apr; 26(4): 603–609. doi: 10.1111/ene.13863.
40.
Flachenecker P, Stuke K, Elias W, Freidel M, Haas J, Pitschnau-Michel D, et al. Multiple sclerosis registry in Germany: results of the extension phase 2005/2006. Dtsch Arztebl Int. 2008; 105(7): 113–9.
41.
Julian LJ, Vella L, Vollmer T, Hadjimichael O, Mohr DC. Employment in multiple sclerosis. Exiting and re-entering the work force. J Neurol. 2008 Sep; 255(9): 1354–60.
42.
Bøe Lunde HM, Telstad W, Grytten N, Kyte L, Aarseth J, Myhr K-M, et al. Employment among Patients with Multiple Sclerosis-A Population Study. Ed. Roberto Furlan. PLoS ONE. 2014; 9(7): e103317.
43.
Matz CJ, Stieb DM, Brion O. Urban-rural differences in daily time-activity patterns, occupational activity and housing characteristics. Environ Health. 2015; 14: 88. doi:10.1186/s12940-015-0075-y.
44.
Marrie RA, Horwitz R, Cutter G, Tyry T, Campagnolo D, Vollmer T. Comorbidity, socioeconomic status and multiple sclerosis. Mult Scler 2008; 14: 1091–1098.
45.
Minkler M, Fuller-Thomson E, Guralnik JM. Gradient of Disability across the Socioeconomic Spectrum in the United States. N Engl J Med 2006; 355: 695–703.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.