Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
VARIA
Iron deficiency, iron deficiency anaemia and anaemia of inflammation – an overview
1
Department of Paediatric Propedeutics, Medical University, Lublin, Poland
Corresponding author
Beata Kulik-Rechberger
Medical University of Lublin, Department of Paediatric Propedeutics, Lublin, Poland
Medical University of Lublin, Department of Paediatric Propedeutics, Lublin, Poland
Ann Agric Environ Med. 2024;31(1):151-157
KEYWORDS
TOPICS
ABSTRACT
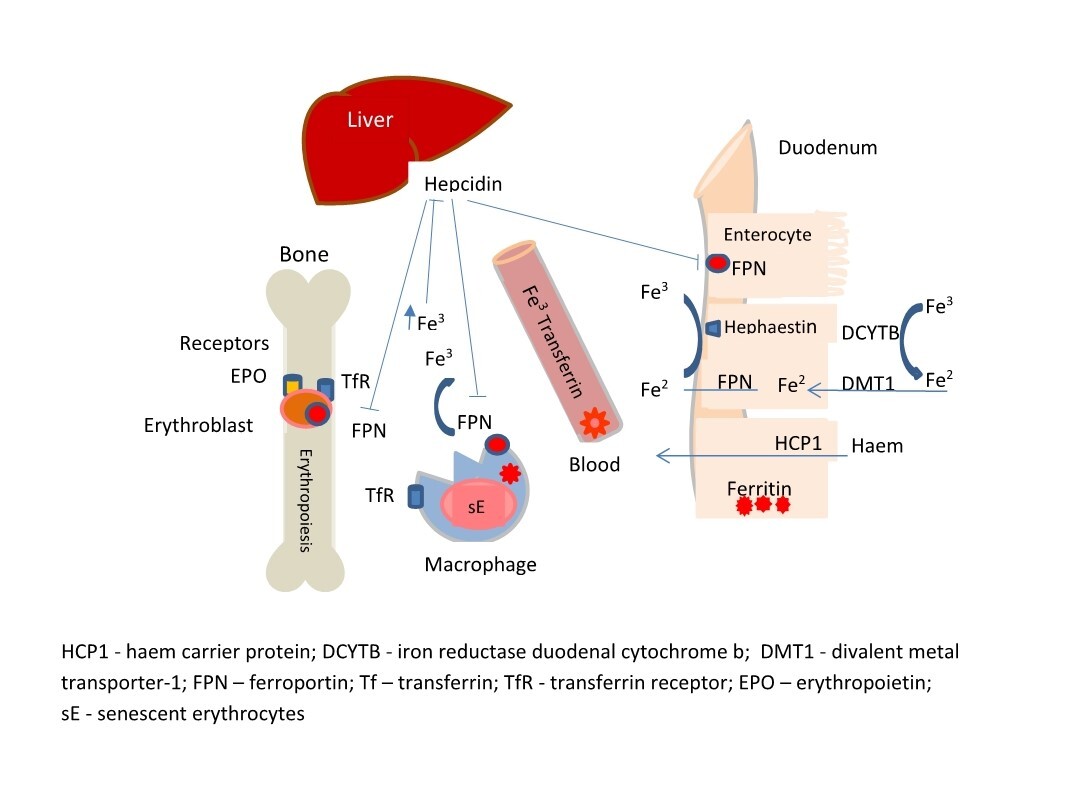
Iron is an essential trace element for various cellular proteins and for biological processes in all cells. Severe iron deficiency (ID) impairs haem synthesis, reduces erythropoiesis and causes iron deficiency anaemia (IDA). Iron restriction in anaemia of inflammation is mainly due to retention of iron in macrophages. This condition is known as ‘functional iron deficiency’. A review of studies performed in Europe shows that the prevalence of ID and IDA in young children varies by region. It is more common in eastern than western European countries. This overview summarises information on the need for iron supplementation in children, and the current understanding of the regulatory mechanisms of iron homeostasis and ironrestricted erythropoiesis. The causes of anaemia during infection and the usefulness of classical and new indicators to distinguish absolute from functional iron deficiency are discussed.
REFERENCES (59)
1.
Janbek J, Sarki M, Specht IO, et al. A systematic literature review of the relation between iron status/anemia in pregnancy and offspring neurodevelopment. Eur J Clin Nutr. 2019;73(12):1561–1578.
2.
Gattermann N, Muckenthaler MU, Kulozik AE, et al. The Evaluation of Iron Deficiency and Iron Overload. Dtsch Arztebl Int. 2021;118(49):847–856.
3.
McCann S, Perapoch Amadó M, Moore SE. The Role of Iron in Brain Development: A Systematic Review. Nutrients. 2020;12(7):2001.
4.
Wiegersma AM, Dalman C, Lee BK, et al. Association of Prenatal Maternal Anemia With Neurodevelopmental Disorders. JAMA Psychiatry. 2019;76(12):1294–1304.
5.
Means RT. Iron Deficiency and Iron Deficiency Anemia: Implications and Impact in Pregnancy, Fetal Development, and Early Childhood Parameters. Nutrients. 2020;12(2):447.
6.
World Health Organization. (2022). WHO Global anemia estimates, 2021 Edition. Global anemia estimates in women of reproductive age, by pregnancy status, and in children aged 6–59 months. https://www.who.int/data/gho/d....
7.
Christian P, Smith ER. Adolescent Undernutrition: Global Burden, Physiology, and Nutritional Risks. Ann Nutr Metab. 2018;72(4):316–328.
8.
Shao J, Lou J, Rao R, et al. Maternal serum ferritin concentration is positively associated with newborn iron stores in women with low ferritin status in late pregnancy. J Nutr. 2012;142(11):2004–2009.
9.
van der Merwe LF, Eussen SR. Iron status of young children in Europe. Am J Clin Nutr. 2017;106 (Suppl 6):1663S–1671S.
10.
Gupta PM, Perrine CG, Mei Z, et al. Iron, Anemia, and Iron Deficiency Anemia among Young Children in the United States Nutrients 2016, 8, 330. Nutrients. 2017;9(8):876.
11.
Gedfie S, Getawa S, Melku M. Prevalence and Associated Factors of Iron Deficiency and Iron Deficiency Anemia Among Under-5 Children: A Systematic Review and Meta-Analysis. Glob Pediatr Health. 2022;9:2333794X221110860.
12.
Tang D, Chen X, Kang R, et al. Ferroptosis: molecular mechanisms and health implications. Cell Res. 2021;31(2):107–125.
13.
Zhang DL, Ghosh MC, Rouault TA. The physiological functions of iron regulatory proteins in iron homeostasis – an update. Front Pharmacol. 2014;5:124.
14.
Galetti V, Stoffel NU, Sieber C, et al. Threshold ferritin and hepcidin concentrations indicating early iron deficiency in young women based on upregulation of iron absorption. EClinicalMedicine. 2021;39:101052.
16.
Anderson GJ, Frazer DM. Current understanding of iron homeostasis. Am J Clin Nutr. 2017;106(Suppl 6):1559S–1566S. doi:10.3945/ajcn.117.155804.
17.
Chen JJ. Regulation of protein synthesis by the heme-regulated eIF2alpha kinase: relevance to anemias. Blood. 2007;109(7):2693–2699.
18.
Powers JM, Buchanan GR. Disorders of Iron Metabolism: New Diagnostic and Treatment Approaches to Iron Deficiency. Hematol Oncol Clin North Am. 2019;33(3):393–408.
19.
Chaber R. Jak wstępnie w 4 krokach zdiagnozować niedokrwistość u dziecka – kompendium dla lekarzy POZ Standardy Medyczne/Pediatria 2023. Vol. 20:41–51.
21.
Munro MG, Mast AE, Powers JM, et al. The relationship between heavy menstrual bleeding, iron deficiency, and iron deficiency anemia. Am J Obstet Gynecol. 2023;S0002–9378(23)00024–8.
22.
Abioye AI, McDonald EA, Park S, et al. Maternal anemia type during pregnancy is associated with anemia risk among offspring during infancy. Pediatr Res. 2019;86(3):396–402.
23.
Camaschella C. Iron deficiency [published correction appears in Blood. 2023 Feb 9;141(6):682]. Blood. 2019;133(1):30–39.
24.
Fisher AL, Nemeth E. Iron homeostasis during pregnancy. Am J Clin Nutr. 2017;106(Suppl 6):1567S–1574S.
25.
Donker AE, van der Staaij H, Swinkels DW. The critical roles of iron during the journey from fetus to adolescent: Developmental aspects of iron homeostasis. Blood Rev. 2021;50:100866.
26.
Davidson EM, Simpson JA, Fowkes FJI. The interplay between maternal-infant anemia and iron deficiency. Nutr Rev. 2023;81(4):480–491.
27.
Mattiello V, Schmugge M, Hengartner H, et al. Diagnosis and management of iron deficiency in children with or without anemia: consensus recommendations of the SPOG Pediatric Hematology Working Group. Eur J Pediatr. 2020;179(4):527–545.
28.
National Institutes of Health Office of Dietary Supplements: Iron Fact Sheet for Health Professionals Accessed 9/2/2019.
29.
Muckenthaler MU, Rivella S, Hentze MW, et al. A Red Carpet for Iron Metabolism. Cell. 2017;168(3):344–361.
30.
Fewtrell M, Bronsky J, Campoy C, et al. Complementary Feeding: A Position Paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on Nutrition. J Pediatr Gastroenterol Nutr. 2017;64(1):119–132.
31.
EFSA Panel on Dietetic Products Nutrition and Allergies. Scientific opinion on dietary reference values for iron. EFSA J 2015;13:4254.
32.
Lauterbach R. Homeostaza żelaza – zapobieganie niedoborowi we wczesnym okresie rozwoju. In: Standardy Opieki Medycznej nad Noworodkiem w Polsce – zalecenia Polskiego Towarzystwa Neonatologicznego. 4th ed. Warszawa: Media-Press Sp. z o.o.; 2021. p. 471–475.
33.
Domellöf M, Braegger C, Campoy C, et al. Iron requirements of infants and toddlers. J Pediatr Gastroenterol Nutr. 2014;58(1):119–129.
34.
World Health Organization. Daily iron supplementation in infants and children Guideline. Geneva: World Health Organization; 2016.
35.
Nairz M, Theurl I, Wolf D, et al. Iron deficiency or anemia of inflammation?: Differential diagnosis and mechanisms of anemia of inflammation. Eisenmangel oder Entzündungsanämie?: Differenzialdiagnose und Mechanismen der Entzündungsanämie. Wien Med Wochenschr. 2016;166(13–14):411–423.
36.
Weiss G, Ganz T, Goodnough LT. Anemia of inflammation. Blood. 2019;133(1):40–50.
37.
Nemeth E, Rivera S, Gabayan V, et al. IL-6 mediates hypoferremia of inflammation by inducing the synthesis of the iron regulatory hormone hepcidin. J Clin Invest. 2004;113(9):1271–1276.
38.
Marques O, Weiss G, Muckenthaler MU. The role of iron in chronic inflammatory diseases: from mechanisms to treatment options in anemia of inflammation. Blood. 2022;140(19):2011–2023.
39.
Bergamaschi G, Borrelli de Andreis F, Aronico N, et al. Anemia in patients with Covid-19: pathogenesis and clinical significance [published correction appears in Clin Exp Med. 2021;21(2):239–246.
40.
Ganz T, Nemeth E. Iron sequestration and anemia of inflammation. Semin Hematol. 2009;46:387–393.
41.
Abbas M, Hayirli Z, Drakesmith H, et al. Effects of iron deficiency and iron supplementation at the host-microbiota interface: Could a piglet model unravel complexities of the underlying mechanisms? Front Nutr. 2022;9:927754.
42.
Hess SY, Owais A, Jefferds MED, et al. Accelerating action to reduce anemia: Review of causes and risk factors and related data needs. Ann N Y Acad Sci. 2023;1523(1):11–23.
43.
Tanous O, Levin C, Suchdev PS, et al. Resolution of iron deficiency following successful eradication of Helicobacter pylori in children. Acta Paediatr. 2022;111(5):1075–1082.
44.
Pasricha SR, Tye-Din J, Muckenthaler MU, et al. Iron deficiency. Lancet. 2021;397(10270):233–248.
45.
Kumar SB, Arnipalli SR, Mehta P, et al. Iron Deficiency Anemia: Efficacy and Limitations of Nutritional and Comprehensive Mitigation Strategies. Nutrients. 2022;14(14):2976.
46.
Cappellini MD, Motta I. Anemia in Clinical Practice-Definition and Classification: Does Hemoglobin Change With Aging?. Semin Hematol. 2015;52(4):261–269.
47.
WHO, UNICEF, UNU: Iron deficiency anemia: assessment, prevention, and control: a guide for programme managers. Geneva: World Health Organization; 2001. WHO/ NHD/01.3.
48.
WHO. WHO guideline on use of ferritin concentrations to assess iron status in individuals and populations. 2020. https://www.who.int/publicatio... (accessed Nov 14, 2020).
49.
Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372(19): 1832–1843.
50.
Dignass A, Farrag K, Stein J. Limitations of Serum Ferritin in Diagnosing Iron Deficiency in Inflammatory Conditions. Int J Chronic Dis. 2018;2018:9394060.
51.
Baker RD, Greer FR; Committee on Nutrition American Academy of Pediatrics. Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics. 2010;126(5):1040–1050.
52.
Mukhtarova N, Ha B, Diamond CA, et al. Serum Ferritin Threshold for Iron Deficiency Screening in One-Year-Old Children. J Pediatr. 2022;245:217–221.
53.
Gelaw Y, Woldu B, Melku M. The Role of Reticulocyte Hemoglobin Content for Diagnosis of Iron Deficiency and Iron Deficiency Anemia, and Monitoring of Iron Therapy: a Literature Review. Clin Lab. 2019;65(12):10.7754/Clin.Lab.2019.190315.
54.
Ogawa C, Tsuchiya K, Maeda K. Reticulocyte hemoglobin content. Clin Chim Acta. 2020 May;504:138–145.
55.
Soldin OP, Miller M, Soldin SJ. Pediatric reference ranges for zinc protoporphyrin. Clin Biochem. 2003;36(1):21–5.
56.
Rohner F, Namaste SM, Larson LM, et al. Adjusting soluble transferrin receptor concentrations for inflammation: Biomarkers Reflecting Inflammation and Nutritional Determinants of Anemia (BRINDA) project. Am J Clin Nutr. 2017;106(Suppl 1):372S–382S.
57.
Bhatia P, Siyaram D, Deepshikha, et al. Lower Plasma Soluble Transferrin Receptor Range in Healthy Indian Pediatric Cohort as Compared to Asian and Western Data. Indian J Hematol Blood Transfus. 2017;33(3):405–407.
58.
Pagani A, Nai A, Silvestri L, Camaschella C. Hepcidin and Anemia: A Tight Relationship. Front Physiol. 2019;10:1294.
59.
Au TY, Benjamin S, Wiśniewski OW. Is the Role of Hepcidin and Erythroferrone in the Pathogenesis of Beta Thalassemia the Key to Developing Novel Treatment Strategies? Thalass Rep. 2022, 12, 123–134.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.