Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Intestinal parasitic infections among school children in northern Madagascar
1
Department of Epidemiology and Tropical Medicine, Military Institute of Medicine – National Research Institute, Warsaw, Poland
2
Clinique Medicale Beyzym, Manerinerina, Madagascar
Corresponding author
Krzysztof Korzeniewski
Department of Epidemiology and Tropical Medicine, Military Institute of Medicine - National Research Institute, Szaserów St. 128, 04-141, Warszawa, Poland
Department of Epidemiology and Tropical Medicine, Military Institute of Medicine - National Research Institute, Szaserów St. 128, 04-141, Warszawa, Poland
Ann Agric Environ Med. 2024;31(4):546-551
KEYWORDS
TOPICS
Biological agents posing occupational risk in agriculture, forestry, food industry and wood industry and diseases caused by these agents (zoonoses, allergic and immunotoxic diseases)State of the health of rural communities depending on various factors: social factors, accessibility of medical care, etc.
ABSTRACT
Introduction and objective:
According to the World Health Organization (WHO) more than 95% of all parasitic infections reported globally result from poverty, poor personal hygiene practices, open defecation practices, consumption of contaminated drinking water, and improper handling of food. The rates of parasitic infections are particularly high in the paediatric population. One of the low-income African countries, where 75% of residents live below the poverty level, is the island of Madagascar. The aim of the study was to assess the prevalence of intestinal parasitic infections among school children living in northern Madagascar.
Material and methods:
The screening was conducted in October 2023 and involved a group of 241 school children aged 5–15 years, inhabiting the Mampikony district of Madagascar. Single stool samples were collected from study participants, the samples were fixed in SAF solution, transported from Africa to Europe, and analyzed by light microscopy using 3 different diagnostic methods (direct smear, decantation with distilled water, Fülleborn method) at the Department of Epidemiology and Tropical Medicine, Military Institute of Medicine – National Research Institute in Poland.
Results:
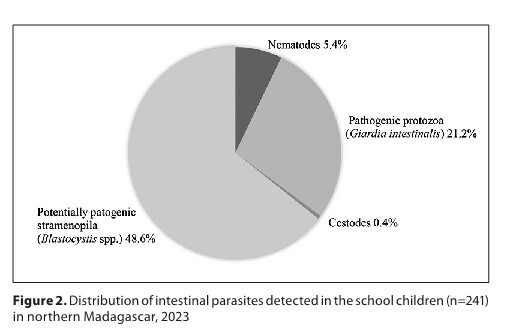
The overall prevalence of intestinal parasites in the study group was found to be 71.0%. Pathogenic intestinal parasites were detected in 65 patients (27.0%), with Giardia intestinalis being the most prevalent (21.2%). Most infections were caused by potentially pathogenic stramenopila Blastocystis spp. (48.6%).
Conclusions:
The prevalence of intestinal parasitic infections is high in the community of school children in northern Madagascar. There is an urgent need to implement long-term prevention measures which would effectively limit the spread of new cases, and reduce the prevalence rates of intestinal infections in the local community.
According to the World Health Organization (WHO) more than 95% of all parasitic infections reported globally result from poverty, poor personal hygiene practices, open defecation practices, consumption of contaminated drinking water, and improper handling of food. The rates of parasitic infections are particularly high in the paediatric population. One of the low-income African countries, where 75% of residents live below the poverty level, is the island of Madagascar. The aim of the study was to assess the prevalence of intestinal parasitic infections among school children living in northern Madagascar.
Material and methods:
The screening was conducted in October 2023 and involved a group of 241 school children aged 5–15 years, inhabiting the Mampikony district of Madagascar. Single stool samples were collected from study participants, the samples were fixed in SAF solution, transported from Africa to Europe, and analyzed by light microscopy using 3 different diagnostic methods (direct smear, decantation with distilled water, Fülleborn method) at the Department of Epidemiology and Tropical Medicine, Military Institute of Medicine – National Research Institute in Poland.
Results:
The overall prevalence of intestinal parasites in the study group was found to be 71.0%. Pathogenic intestinal parasites were detected in 65 patients (27.0%), with Giardia intestinalis being the most prevalent (21.2%). Most infections were caused by potentially pathogenic stramenopila Blastocystis spp. (48.6%).
Conclusions:
The prevalence of intestinal parasitic infections is high in the community of school children in northern Madagascar. There is an urgent need to implement long-term prevention measures which would effectively limit the spread of new cases, and reduce the prevalence rates of intestinal infections in the local community.
REFERENCES (34)
1.
Torgerson PR, Devleesschauwer B, Praet N, et al. World Health Organization Estimates of the Global and Regional Disease Burden of 11 Foodborne Parasitic Diseases, 2010: A Data Synthesis. PLoS Med. 2015;12(12):e1001920. https://doi:10.1371/journal.pm....
2.
Fauziah N, Aviani JK, Agrianfanny YN, et al. Intestinal parasitic infection and nutritional status in children under five years old: a systematic review. Trop Med Infect Dis. 2022;7(11):371. https://doi:10.3390/tropicalme....
3.
Hajissa K, Islam MA, Sanyang AM, et al. Prevalence of intestinal protozoan parasites among school children in Africa: A systematic review and meta-analysis. PLoS Negl Trop Dis. 2022;16(2):e0009971. https://doi:10.1371/journal.pn....
4.
Simelane N, Thembane N. Prevalence of intestinal parasite infections among paediatric populations in underdeveloped nations: a review. Student’s J Health Res Africa. 2023;4(6):9.
5.
Chelkeba L, Mekonnen Z, Alemu Y, et al. Epidemiology of intestinal parasitic infections in preschool and school-aged Ethiopian children: a systematic review and meta-analysis. BMC Public Health. 2020;20(1):117. https://doi:10.1186/s12889-020....
6.
Ngowi HA. Prevalence and pattern of waterborne parasitic infections in eastern Africa: A systematic scoping review. Food Waterborne Parasitol. 2020;8(20):e00089. https://doi:10.1016/j.fawpar.2....
7.
World Health Organization. Soil-transmitted helminth infections. Geneva: WHO; 2017.
8.
United Nations. UN list of least developed countries. Available at: https://unctad.org/topic/least... (access: 2024.02.08).
9.
Kasprowicz D. Medics to Africa. The level of achievement of the millennium development goals on the example of Madagascar. Ann Acad Med Gedan. 2014;44:143–155.
10.
Rahantamalala A, Rakotoarison RL, Rakotomalala E, et al. Prevalence and factors associated with human Taenia solium taeniosis and cysticercosis in twelve remote villages of Ranomafana rainforest, Madagascar. PLoS Negl Trop Dis. 2022;16(4):e0010265. https://doi: 10.1371/journal.pntd.0010265.
11.
Garcia LS. Practical Guide to Diagnostic Parasitology. 2nd ed. Washington DC, USA: ASM Press; 2009.
12.
Birhanu M, Gedefaw L, Asres Y. Anemia among school-age children: magnitude, severity and associated factors in Pawe Town, Benishangul-Gumuz Region, Northwest Ethiopia. Ethiop J Health Sci. 2018;28(3):259–266. https://doi:10.4314/ejhs.v28i3....
13.
Korzeniewski K, Augustynowicz A, Bylicka-Szczepanowska E, et al. Intestinal parasitic infections in a population of BaAka Pygmies inhabiting the Congo Basin in the Central African Republic. Ann Agric Environ Med. 2021;28(1):127–130. https://doi:10.26444/aaem/1316....
14.
World Health Organization. Global distribution and prevalence of soil-transmitted helminth infections. Geneva: WHO key fact sheet; 2020.
15.
World Health Organization. Investing to overcome the global impact of neglected tropical diseases: third WHO report on neglected tropical diseases 2015. Geneva: WHO; 2015.
16.
Ahmed M. Intestinal Parasitic Infections in 2023. Gastroenterology Res. 2023;16(3):127–140. https://doi:10.14740/gr1622.
17.
Greigert V, Abou-Bacar A, Brunet J, et al. Human intestinal parasites in Mahajanga, Madagascar: The kingdom of the protozoa. PLoS One. 2018;13(10):e0204576. https://doi:10.1371/journal.po....
18.
Camacho-Alvarez I, Goyens P, Luizaga-López JM, Jacobs F. Geographic differences in the distribution of parasitic infections in children of Bolivia. Parasite Epidemiol Control. 2021;14:e00217. https://doi:10.1016/j.parepi.2....
19.
Cociancic P, Torrusio SE, Zonta ML, Navone GT. Risk factors for intestinal parasitoses among children and youth of Buenos Aires, Argentina. One Health. 2019;9:100116. https://doi:10.1016/j.onehlt.2....
20.
Hernández-Castro C, Agudelo-López SDP, Medina-Lozano AP, et al. The burden of intestinal parasitic infections in Antioquia, Colombia: Impact in childhood growth development and nutritional status. Acta Trop. 2024;251:107119. https://doi:10.1016/j.actatrop....
21.
Daryani A, Hosseini-Teshnizi S, Hosseini SA, et al. Intestinal parasitic infections in Iranian preschool and school children: A systematic review and meta-analysis. Acta Trop. 2017;169:69–83.
22.
Okyay P, Ertug S, Gultekin B, et al. Intestinal parasites prevalence and related factors in school children, a western city sample-Turkey. BMC Public Health. 2004;4:64.
23.
Sanprasert V, Srichaipon N, Bunkasem U, et al. Prevalence of intestinal protozoan infections among children in Thailand: a large-scale screening and comparative study of three standard detection methods. Southeast Asian J Trop Med Public Health. 2016;47(6):1123–33.
24.
Sharma AK, Khan S. Prevalence of intestinal parasitic infection in children among age of 6 to 12 years in rural area of Bareilly District: cross sectional study. Indian J Community Health. 2020;32(4):677–680.
25.
Khan W, Rahman H, Rafiq N, et al. Risk factors associated with intestinal pathogenic parasites in schoolchildren. Saudi J Biol Sci. 2022;29(4):2782–2786. https://doi:10.1016/j.sjbs.202....
26.
Kantzanou M, Karalexi MA, Vrioni G, Tsakris A. Prevalence of intestinal parasitic infections among children in Europe over the last five years. Trop Med Infect Dis. 2021;6(3):160. https://doi:10.3390/tropicalme....
27.
Ghiwot Y, Degarege A, Erko B. Prevalence of intestinal parasitic infections among children under five years of age with emphasis on Schistosoma mansoni in Wonji Shoa Sugar Estate, Ethiopia. PLoS One. 2014;9(10):e109793. https://doi:10.1371/journal.po....
28.
Hakizimana E, Kim JY, Oh S, et al. Intestinal parasitic infections among children aged 12–59 months in Nyamasheke District, Rwanda. Parasites Hosts Dis. 2023;61(3):304–309. https://doi:10.3347/PHD.23045.
29.
Oyegue-Liabagui SL, Ndjangangoye NK, Kouna LC, et al. 7. Molecular prevalence of intestinal parasites infections in children with diarrhea in Franceville, Southeast of Gabon. BMC Infect Dis. 2020;20(1):350. https://doi: 10.1186/s12879-020-05071-x.
30.
Buchy P. Intestinal parasitoses in the Mahajanga region, west coast of Madagascar. Bull Soc Pathol Exot. 2003;96(1):41–45 [in French].
31.
Sartorius B, Cano J, Simpson H, et al. Prevalence and intensity of soil-transmitted helminth infections of children in sub-Saharan Africa, 2000–18: a geospatial analysis. Lancet Glob Health. 2021;9(1):e52-e60. https://doi:10.1016/S2214-109X....
32.
Razafiarimanga ZN, Yao YBK, Rajerison M, et al. Risk factors for intestinal parasite portage in an informal suburb on the West coast of Madagascar. Parasite Epidemiol Control. 2022;19:e00267. https://doi:10.1016/j.parepi.2....
33.
Habib A, Andrianonimiadana L, Rakotondrainipiana M, et al. High prevalence of intestinal parasite infestations among stunted and control children aged 2 to 5 years old in two neighborhoods of Antananarivo, Madagascar. PLoS Negl Trop Dis. 2021;15(4):e0009333. https://doi:10.1371/journal.pn....
34.
Garcia LS, Campbell J, Fritsche PTR, et al. Procedures for the recovery and identification of parasites from the intestinal tract, Approved Guideline. Pensylvania: Clinical and Laboratory Standards Institute; 2005.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.