Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Intensification of anxiety, symptoms of depression, and level of social support among women in pathological pregnancy – a cross-sectional preliminary study
1
Department of Health Psychology, Institute of Nursing and Midwifery, Jagiellonian University Medical College (Collegium Medicum), Kraków, Poland
2
Department of Obstetrics and Gynecology, College of Medicine and Health Sciences (CMHS), United Arab Emirates University (UAEU); Żelazna Medical Centre, Warsaw, Poland
3
Chair of Obstetrics and Gynecology, Faculty of Health Sciences, Medical University, Lublin, Poland
4
Department of Cosmetology and Aesthetic Medicine, Faculty of Pharmacy, Medical University, Lublin, Poland
5
Departament of Dermatology, National Medical Institute of the Ministry of the Interior and Administration, Warsaw, Poland
6
Department of Obstetrics and Pathology of Pregnancy, Medical University, Lublin, Poland
7
Department of Women’s Health, Institute of Rural Health, Lublin, Poland
8
Second Department of Gynecology, Medical University, Lublin, Poland
9
Department of Mother and Child Health, Institute of Nursing and Midwifery, Jagiellonian University Medical College (Collegium Medicum), Kraków, Poland
Corresponding author
Michal Filip
Department of Obstetrics and Pathology of Pregnancy, Medical University of Lublin, Poland
Department of Obstetrics and Pathology of Pregnancy, Medical University of Lublin, Poland
Ann Agric Environ Med. 2024;31(2):255-263
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Women in pathological pregnancy are a group of patients especially exposed to the risk of occurrence of psychological complications. The aim of the study was assessment of the risk of depressive and anxiety disorders, and the relationship between the intensity of symptoms and social support.
Material and methods:
The study group were 300 patients hospitalized in the Department of Pathology of Pregnancy. The study was conducted using the State-Trait Anxiety Inventory (STAI), the Hospital Anxiety and Depression Scale (HADS), the Inventory of Socially Supportive Behaviours (ISSB), and an author-constructed socio-demographic questionnaire.
Results:
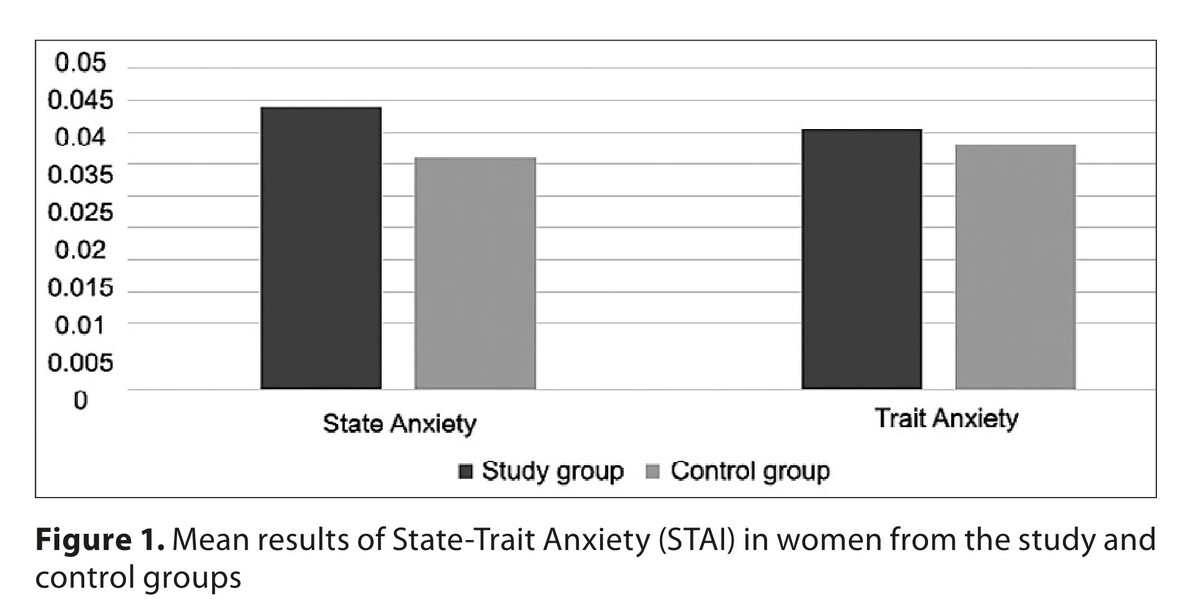
The level of State Anxiety (STAI) was higher in respondents from the study group, compared to the control group. The level of anxiety (HADS-A) was higher in the control group than in women from the study group. The level of social informational support was higher in those from the control group, compared to those from the study group. The level of emotional support was lower in respondents from the study group, compared to those from the control group. Instrumental support negatively correlated with the symptoms of depression among women in physiological pregnancy. The lack of evaluative support statistically significantly correlated with anxiety among women hospitalized before labour.
Conclusions:
The results obtained suggest the necessity for the substantive preparation of medical and psychological staff employed in departments of pathology of pregnancy to provide proper emotional and informational support for hospitalized women.
Women in pathological pregnancy are a group of patients especially exposed to the risk of occurrence of psychological complications. The aim of the study was assessment of the risk of depressive and anxiety disorders, and the relationship between the intensity of symptoms and social support.
Material and methods:
The study group were 300 patients hospitalized in the Department of Pathology of Pregnancy. The study was conducted using the State-Trait Anxiety Inventory (STAI), the Hospital Anxiety and Depression Scale (HADS), the Inventory of Socially Supportive Behaviours (ISSB), and an author-constructed socio-demographic questionnaire.
Results:
The level of State Anxiety (STAI) was higher in respondents from the study group, compared to the control group. The level of anxiety (HADS-A) was higher in the control group than in women from the study group. The level of social informational support was higher in those from the control group, compared to those from the study group. The level of emotional support was lower in respondents from the study group, compared to those from the control group. Instrumental support negatively correlated with the symptoms of depression among women in physiological pregnancy. The lack of evaluative support statistically significantly correlated with anxiety among women hospitalized before labour.
Conclusions:
The results obtained suggest the necessity for the substantive preparation of medical and psychological staff employed in departments of pathology of pregnancy to provide proper emotional and informational support for hospitalized women.
REFERENCES (65)
1.
Soma-Pillay P, Nelson-Piercy C, Tolppanen H, Mebazaa A. Physiological changes in pregnancy. Cardiovasc J Afr. 2016;27(2):89–94. doi:10.5830/CVJA-2016-021.
2.
Forte Camarneiro AP, de Miranda Justo JMR. Emotional states and psychopathological symptoms in couples during pregnancy and post-partum. J Reprod Infant Psychol. 2022;40(4):384–398. doi:10.1080/02646838.2020.1814226.
3.
Bayrampour H, Ali E, McNeil DA, Benzies K, MacQueen G, Tough S. Pregnancy-related anxiety: A concept analysis. Int J Nurs Stud. 2016;55:115–130. doi:10.1016/j.ijnurstu.2015.10.023.
4.
Liu Y, Zhang L, Guo N, Jiang H. Postpartum Depression and Postpartum Post-Traumatic Stress Disorder: Prevalence and Associated Factors. BMC Psychiatry. 2021;21:487. doi:10.1186/s12888-021-03432-7.
5.
Glover V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract Res Clin Obstet Gynaecol. 2014;28(1):25–35. doi:10.1016/j.bpobgyn.2013.08.017.
6.
Dudenhausen JW, Pschyrembel W. Praktische Geburtshilfe: mit geburtshilflichen Operationen. 22 erweiterte und korrigierte Auflage. De Gruyter Berlin Boston. 2019.
7.
Traylor CS, Johnson JD, Kimmel MC, Manuck TA. Effects of psychological stress on adverse pregnancy outcomes and nonpharmacologic approaches for reduction: an expert review. Am J Obstet Gynecol MFM. 2020;2(4):100229. doi:10.1016/j.ajogmf.2020.100229.
8.
Khil J, Picardo S, Seow CH, et al. Physiological and psychological stress in pregnant women with quiescent inflammatory bowel disease: A pilot study using salivary biomarkers. JGH Open. 2020;4(4):692–697. Published 2020 Mar 4. doi:10.1002/jgh3.12317.
9.
Szymona-Pałkowska K. Psychologiczna analiza doświadczeń rodziców w sytuacji ciaży wysokiego ryzyka. Lublin: Prace Wydziału Nauk Społecznych/Towarzystwo Naukowe Katolickiego Uniwersytetu Lubelskiego. Tow. Naukowe Katolickiego Uniwersytetu Lubelskiego; 2005.
11.
Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Consult Psychol Press Palo Alto 1983.
12.
Cattell RB. Psychological Measurement of Anxiety and Depression: A Quantitative Approach. Can Psychiatric Assoc J. 1962;7(1_suppl):11–23. doi: 10.1177/09067437610070/S03.
13.
Gómez-Polo C, Vilches AA, Ribas D, Castano-Séiquer A, Montero J. Behaviour and Anxiety Management of Paediatric Dental Patients through Virtual Reality: A Randomised Clinical Trial. J Clin Med. 2021;10(14):3019. Published 2021 Jul 7. doi:10.3390/jcm10143019.
14.
Rybakowski J, Pużyński S, Wciórka J. Psychiatria. T. 1, Podstawy psychiatrii. In: Wroclaw: Elsevier Urban & Partner; 2010.
15.
Abdoli N, Salari N, Darvishi N, et al. The global prevalence of major depressive disorder (MDD) among the elderly: A systematic review and meta-analysis. Neurosci Biobehav Rev. 2022;132:1067–1073. doi:10.1016/j.neubiorev.2021.10.041.
16.
Van den Bergh BRH, van den Heuvel MI, Lahti M, et al. Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neurosci Biobehav Rev. 2020;117:26–64. doi:10.1016/j.neubiorev.2017.07.003.
17.
Dadi AF, Miller ER, Bisetegn TA, Mwanri L. Global burden of antenatal depression and its association with adverse birth outcomes: an umbrella review. BMC Public Health. 2020 Feb 4;20(1):173. doi:10.1186/s12889-020-8293-9.
19.
Jahan N, Went TR, Sultan W, et al. Untreated Depression During Pregnancy and Its Effect on Pregnancy Outcomes: A Systematic Review. Cureus. 2021;13(8):e17251. Published 2021 Aug 17. doi:10.7759/cureus.17251.
20.
Stewart CP, Oaks BM, Laugero KD, et al. Maternal cortisol and stress are associated with birth outcomes, but are not affected by lipid-based nutrient supplements during pregnancy: an analysis of data from a randomized controlled trial in rural Malawi. BMC Pregnancy Childbirth. 2015;15:346. Published 2015 Dec 22. doi:10.1186/s12884-015-0793-8.
21.
Nath A, Murthy GVS, Babu GR, Di Renzo GC. Effect of prenatal exposure to maternal cortisol and psychological distress on infant development in Bengaluru, southern India: a prospective cohort study. BMC Psychiatry. 2017;17(1):255. Published 2017 Jul 17. doi:10.1186/s12888-017-1424-x.
22.
Zuccarello D, Sorrentino U, Brasson V, et al. Epigenetics of pregnancy: looking beyond the DNA code. J Assist Reprod Genet. 2022;39(4):801–816. doi:10.1007/s10815-022-02451-x.
23.
Cao-Lei L, Laplante DP, King S. Prenatal Maternal Stress and Epigenetics: Review of the Human Research. Curr Mol Bio Rep. 2016;2:16–25. https://doi.org/10.1007/s40610....
24.
Muraca GM, Joseph KS. The association between maternal age and depression. J Obstet Gynaecol Can. 2014;36(9):803–810. doi:10.1016/S1701-2163(15)30482-5.
25.
Herrera CL, Byrne JJ, Nelson DB, Schell RC, Dashe JS. Postpartum Depression Risk following Prenatal Diagnosis of Major Fetal Structural Anomalies. Am J Perinatol. 2022;39(1):16–21. doi:10.1055/s-0041-1739265.
26.
Ghaedrahmati M, Kazemi A, Kheirabadi G, Ebrahimi A, Bahrami M. Postpartum depression risk factors: A narrative review. J Educ Health Promot. 2017;6:60. Published 2017 Aug 9. doi:10.4103/jehp.jehp_9_16.
27.
Mughal S, Azhar Y, Siddiqui W. Postpartum Depression. Treasure Island (FL): StatPearls Publishing; 2022.
28.
American Psychiatric Association. DSM-5 Task Force. Diagnostic and Statistical Manual of Mental Disorders: DSM-5TM (5th ed.). Am Psych Publishing. 2013.
29.
Carson RC, Butcher JN, Mineka S. Abnormal Psychology and Modern Life. 10. ed. 1998 update. New York: Longman; 1998.
30.
Kessler RC, Sampson NA, Berglund P, et al. Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys. Epidemiol Psychiatr Sci. 2015;24(3):210–226. doi:10.1017/S2045796015000189.
31.
Filipiak G. The Role of Social Support in the Family. Rocz Socjol Rodz. 1999;11:131–144.
32.
Sęk H, Cieślak R, Suchecki J. Wsparcie społeczne, stres i zdrowie. Wyd. 1, 5 dodr. Warszawa: Wydawnictwo Naukowe PWN; 2012.
33.
Thomas PA, Liu H, Umberson D. Family Relationships and Well-Being. Innov Aging. 2017;1(3):igx025. doi:10.1093/geroni/igx025.
34.
Kebede AA, Gessesse DN, Aklil MB, et al. Low husband involvement in maternal and child health services and intimate partner violence increases the odds of postpartum depression in northwest Ethiopia: A community-based study. PLoS One. 2022;17(10):e0276809. Published 2022 Oct 26. doi:10.1371/journal.pone.0276809.
35.
Stapleton LR, Schetter CD, Westling E, et al. Perceived partner support in pregnancy predicts lower maternal and infant distress. J Fam Psychol. 2012;26(3):453–463. doi:10.1037/a0028332.
36.
Ding R, Guo C, Song X, Zheng X. Male knowledge, attitude and practice and partner pregnancy among Chinese unmarried youth. PLoS One. 2019;14(3):e0214452. Published 2019 Mar 26. doi:10.1371/journal.pone.0214452.
37.
Wrzesniewski K. Inwentarz Stanu i Cechy Lęku STAI: Polska Adaptacja STAI: Podręcznik. 2006.
38.
Karakuła H, Grzywa A, Śpila B, Baszak J, Gieroba A, Kosikowski W, Jędrych M. Zastosowanie Skali Lęku i Depresji – HADS w Chorobach Psychosomatycznych. (The Application of Hospital Anxiety and Depression Scale in Psychosomatic Disorder.). Psychiatr Pol. 1996;30:653–668.
39.
Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J Psychosom Res. 2002;52(2):69–77. doi:10.1016/s0022-3999(01)00296-3.
40.
Krystyna B, Hanna PB. Polska adaptacja Wielowymiarowej Skali Spostrzeganego Wsparcia Społecznego. Pol Forum Psychol; 2017. doi:10.14656/PFP20170404.
41.
Bedaso A, Adams J, Peng W, Sibbritt D. The relationship between social support and mental health problems during pregnancy: a systematic review and meta-analysis. Reprod Health. 2021;18(1):162. Published 2021 Jul 28. doi:10.1186/s12978-021-01209-5.
42.
Włodarczyk-Semczuk A, Pempel K. Death of Pregnant Woman Ignites Debate about Abortion Ban in Poland. Reuters 2021.
43.
Rutkowska A, Rolińska A, Kwaśniewski W, Makara-Studzińska M, Kwaśniewska A. Anxiety as a State and Trait in Women with Normal and Highly Compromised Pregnancy. Curr Probl Psychiatry. 2011;12:56–59.
44.
Luo Y, Zhang K, Huang M, Qiu C. Risk factors for depression and anxiety in pregnant women during the COVID-19 pandemic: Evidence from meta-analysis. PLoS One. 2022;17(3):e0265021. Published 2022 Mar 4. doi:10.1371/journal.pone.0265021.
45.
Noury R, Karimi N, Mohammadi M. Relationship between Prenatal Depression with Social Support and Marital Satisfaction. Sarem J Reprod Med. 2016;1:153–157. doi:10.29252/sjrm.1.4.153.
46.
Mabetha K, Soepnel L, Klingberg S, Mabena G, Motlhatlhedi M, Norris SA, Draper CE. Social Support during Pregnancy: A Phenomenological Exploration of Young Women’s Experiences of Support Networks on Pregnancy Care and Wellbeing in Soweto, South Africa. Obstetrics and Gynecology. 2022.
47.
Morikawa M, Okada T, Ando M, et al. Relationship between social support during pregnancy and postpartum depressive state: a prospective cohort study. Sci Rep. 2015;5:10520. Published 2015 May 29. doi:10.1038/srep10520.
48.
Branecka -Woźniak D. [The assessment of anxiety in pregnant women in respect of biological, medical and socio-environmental factors]. Pomeranian J Life Sci. 2015;61:433–443.
49.
Hijazi HH, Alyahya MS, Al Abdi RM, et al. The Impact of Perceived Social Support During Pregnancy on Postpartum Infant-Focused Anxieties: A Prospective Cohort Study of Mothers in Northern Jordan. Int J Womens Health. 2021;13:973–989. Published 2021 Oct 21. doi:10.2147/IJWH.S329487.
50.
Kamali S, Ahmadian L, Khajouei R, Bahaadinbeigy K. Health information needs of pregnant women: information sources, motives and barriers. Health Info Libr J. 2018;35(1):24–37. doi:10.1111/hir.12200.
51.
Abdi S, Faramarzi M, Bouzari Z, Chehrazi M, Esfandyari M. Association between social support and pregnancy stress: a cross-sectional study of neighbors’ interactions. J Egypt Public Health Assoc. 2022;97(1):15. Published 2022 Sep 12. doi:10.1186/s42506-022-00113-5.
52.
Grzywniak C, Kwiatkowski T, Kobos M, Trystuła M. Transcranial direct current stimulation (tDCS) for post- stroke anxiety and depression following SARS-COV2 infection and neurocovid-19 contraction. Acta Neuropsychol. 2022;20(4):471–483. doi:10.5604/01.3001.0016.1340.
53.
Aknin L, De Neve J, Dunn E, et al. The neurological consequences of contracting COVID-19. Acta Neuropsychol. 2021;19(3):301–305. doi:10.5604/01.3001.0014.9953.
54.
MacQueen B, MacQueen W. Neuro-COVID: A preliminary review. Acta Neuropsychol. 2021;19(3):389–402. doi:10.5604/01.3001.0015.2692.
55.
Khalki H, Ouirari J, Boulbaroud S, Karim H, Abboussi O, Khalki L. Prevalence of symptoms of anxiety, depression and associated socio-demographic factors during the COVID-19 pandemic in Morocco. Acta Neuropsychol. 2022;20(2):159–173. doi:10.5604/01.3001.0015.8750.
56.
Renaud-Charest O, Lui LMW, Eskander S, Ceban F, Ho R, Di Vincenzo JD, Rosenblat JD, Lee Y, Subramaniapillai M, McIntyre RS. Onset and frequency of depression in post-COVID-19 syndrome: A systematic review. J Psychiatr Res. 2021;144:129–137. doi:10.1016/j.jpsychires.2021.09.054.
57.
Ayaz R, Hocaoglu M, Günay T, Yardimci OD, Turgut A, Karateke A. Anxiety and depression symptoms in the same pregnant women before and during the COVID-19 pandemic. J Perinat Med. 2020;48(9):965–970. doi:10.1515/jpm-2020-0380.
58.
Luo Y, Zhang K, Huang M, Qiu C. Risk factors for depression and anxiety in pregnant women during the COVID-19 pandemic: Evidence from meta-analysis. PLoS One. 2022;17(3):e0265021. Published 2022 Mar 4. doi:10.1371/journal.pone.02650.
59.
Campos-Garzón C, Riquelme-Gallego B, de la Torre-Luque A, Caparrós-González RA. Psychological Impact of the COVID-19 Pandemic on Pregnant Women: A Scoping Review. Behav Sci (Basel). 2021;11(12):181. Published 2021 Dec 16. doi:10.3390/bs11120181.
60.
Grigoriadis S, Graves L, Peer M, et al. Maternal Anxiety During Pregnancy and the Association With Adverse Perinatal Outcomes: Systematic Review and Meta-Analysis. J Clin Psychiatry. 2018;79(5):17r12011. Published 2018 Sep 4. doi:10.4088/JCP.17r12011.
61.
Smorti M, Gemignani A, Bonassi L, Mauri G, Carducci A, Ionio C. The impact of Covid-19 restrictions on depressive symptoms in low-risk and high-risk pregnant women: a cross-sectional study before and during pandemic. BMC Pregnancy Childbirth. 2022;22(1):191. Published 2022 Mar 8. doi:10.1186/s12884-022-04515-3.
62.
Abrar A, Fairbrother N, Smith AP, Skoll A, Albert AYK. Anxiety among women experiencing medically complicated pregnancy: A systematic review and meta-analysis. Birth. 2020;47(1):13–20. doi:10.1111/birt.12443.
63.
Burchill E, Lymberopoulos E, Menozzi E, Budhdeo S, McIlroy JR, Macnaughtan J, Sharma N. The Unique Impact of COVID-19 on Human Gut Microbiome Research. Front Med (Lausanne). 2021;8:652464. https://doi.org/10.3389/fmed.2....
64.
Janowska M, Rog J, Karakula-Juchnowicz H. Disruptions within gut microbiota composition induced by improper antibiotics therapy as a probable trigger factor for development of depression – Case Reports. Ann Agric Environ Med. 2021;28(4):713–718. doi:10.26444/aaem/132452.
65.
Liu L, Wang H, Chen X, Zhang Y, Zhang H, Xie P. Gut microbiota and its metabolites in depression: from pathogenesis to treatment. EBioMedicine. 2023;90:104527. doi:10.1016/j.ebiom.2023.104527.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.