Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Hiatal hernia as a rare cause of cardiac complications – case based review of the literature
1
Department of Cardiology, Cardinal Wyszynski Hospital, Lublin, Poland
2
Department of General Surgery, Cardinal Wyszynski Hospital, Lublin, Poland
3
Department of Anaesthesiology and Intensive Therapy, Cardinal Wyszynski Hospital, Lublin, Poland
4
Department of Cardiology, Medical University, Lublin, Poland
Corresponding author
Andrzej Głowniak
Department of Cardiology, Medical University of Lublin, ul. Jaczewskiego 8, 20-090, Lublin, Poland
Department of Cardiology, Medical University of Lublin, ul. Jaczewskiego 8, 20-090, Lublin, Poland
Ann Agric Environ Med. 2021;28(1):20-26
KEYWORDS
TOPICS
ABSTRACT
Introduction:
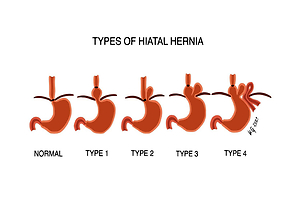
Hiatal hernia (HH) is a condition which refers to the protrusion of an intraabdominal organ in the thorax cavity throughan oesophageal hiatus of the diaphragm. Sliding HH is usually associated with non-specific symptoms, including heartburn, regurgitation or epigastric pain. Importantly, true paraesophageal hernia may lead to cardiac compression. Knowledge of cardiac manifestations of HH is limited.
Objective:
The main aim of the study is to present the rare case of a patient with gastrothorax due to hiatal hernia which caused cardiac arrest, and to provide a literature-based review of the cardiac aspects of hiatal hernia.
Brief description of the state of knowledge:
Patients with paraesophageal hernia may experience arrhythmia, including sinus tachycardia, atrial flutter, atrial fibrillation, supraventricular extrasystole and ventricular tachycardia, as well as left bundle branch block, atrioventricular conduction block and electrocardiographic changes in the ST-segment and T-wave. In echocardiograph, HH may appear as an extracardiac posterior mass encroaching on the left atrial cavity, mimicking the left atrial mass. Rarel, HH may be manifested as tension gastrothorax leading cardiac arrest. In such a case, timely diagnosis and instant adequate treatment of the underlying condition are crucial.
Conclusions:
Hiatal hernia should be considered as a possible cause of arrhythmia and changes in ST-T pattern, particularly if symptoms occurred after a meal. Differential diagnosis of the posterior mediastinal mass or intracardiac mass should include hiatal hernia. Gastrothorax is a rare condition associated with hiatal hernia which may lead to cardiac arrest. However, even timely recognition and therapy of gastrothorax does not ensure a positive clinical outcome.
Hiatal hernia (HH) is a condition which refers to the protrusion of an intraabdominal organ in the thorax cavity throughan oesophageal hiatus of the diaphragm. Sliding HH is usually associated with non-specific symptoms, including heartburn, regurgitation or epigastric pain. Importantly, true paraesophageal hernia may lead to cardiac compression. Knowledge of cardiac manifestations of HH is limited.
Objective:
The main aim of the study is to present the rare case of a patient with gastrothorax due to hiatal hernia which caused cardiac arrest, and to provide a literature-based review of the cardiac aspects of hiatal hernia.
Brief description of the state of knowledge:
Patients with paraesophageal hernia may experience arrhythmia, including sinus tachycardia, atrial flutter, atrial fibrillation, supraventricular extrasystole and ventricular tachycardia, as well as left bundle branch block, atrioventricular conduction block and electrocardiographic changes in the ST-segment and T-wave. In echocardiograph, HH may appear as an extracardiac posterior mass encroaching on the left atrial cavity, mimicking the left atrial mass. Rarel, HH may be manifested as tension gastrothorax leading cardiac arrest. In such a case, timely diagnosis and instant adequate treatment of the underlying condition are crucial.
Conclusions:
Hiatal hernia should be considered as a possible cause of arrhythmia and changes in ST-T pattern, particularly if symptoms occurred after a meal. Differential diagnosis of the posterior mediastinal mass or intracardiac mass should include hiatal hernia. Gastrothorax is a rare condition associated with hiatal hernia which may lead to cardiac arrest. However, even timely recognition and therapy of gastrothorax does not ensure a positive clinical outcome.
REFERENCES (71)
1.
Sfara A, Dumitrascu DL. The management of hiatal hernia: an update on diagnosis and treatment. Med Pharm Rep. 2019; 92(4): 321–325. doi: 10.15386/mpr-1323.
2.
Rochefort M, Wee, JO. Management of the Difficult Hiatal Hernia. Thorac Surg Clin. 2018; 28(4): 533–539. doi: 10.1016/j.thorsurg.2018.07.001.
3.
Roman S, Kahrilas PJ. The diagnosis and management of hiatus hernia. BM. 2014; 349. doi: 10.1136/bmj.g6154.
4.
Siegal SR, Dolan JP, Hunter JG. Modern diagnosis and treatment of hiatal hernias. Langenbecks Arch Surg. 2017; 402(8): 1145–1151. doi: 10.1007/s00423-017-1606-5.
5.
Duranceau A. Massive hiatal hernia: a review. Dis Esophagus. 2016; 29(4): 350–366. doi: 10.1111/dote.12328.
6.
Mitiek MO, Andrade RS. Giant hiatal hernia. Ann Thorac Surg. 2010; 89(6): 2168–2173. doi: 10.1016/j.athoracsur.2010.03.022.
7.
Naoum C, Falk GL, Ng AC, et al. Left atrial compression and the mechanism of exercise impairment in patients with a large hiatal hernia. J Am Coll Cardiol. 2011; 58(15): 1624–1634. doi: 10.1016/j.jacc.2011.07.013.
8.
Solé, C, Rojas S, Vives JP, Sanz E. Tension gastrothorax mimicking acute coronary syndrome and causing cardiac arrest. Eur Heart J. 2014; 35(12): 794. doi: 10.1093/eurheartj/eht336.
9.
Tokur M, Demiröz ŞM, Sayan M. Non-traumatic tension gastrothorax in a young lady. Ulus Travma Acil Cerrahi Derg. 2015; 21(4): 306–308. doi: 10.5505/tjtes.2015.71245.
10.
Shoji T, Tarui T, Kaita Y, et al. A survival case of tension gastrothorax due to hiatal hernia, the key of life-saving is thoracotomy. Am J Emerg Med. 2017; 35(1): 199.e3-199.e5. doi: 10.1016/j.ajem.2016.07.043.
11.
Kao Y, Lee WJ, Lin HJ. Tension gastrothorax: a life-threatening cause of acute abdominal pain. CMAJ 2009; 180(9): 983. doi: 10.1503/cmaj.081094.
12.
Ingelbrecht SN, Kint PA, Belderbos HN. Gastrothorax mimicking acute tension pneumothorax. Acta Clin Belg. 2007; 62(3): 184–186. doi: 10.1179/acb.2007.030.
13.
Rathinam S, Margabanthu G, Jothivel G, et al. Tension gastrothorax causing cardiac arrest in a child. Interact Cardiovasc Thorac Surg. 2002; 1(2): 99–101. doi:10.1016/s1569-9293(02)00064-6.
14.
Ahn S, Kim W, Sohn CH, et al. Tension viscerothorax after blunt abdominal trauma: a case report and review of the literature. J Emerg Med. 2012; 43(6): 451–453. doi: 10.1016/j.jemermed.2011.05.084.
15.
Flamée P, Pregardien C. Tension gastrothorax causing cardiac arrest. CMAJ 2012; 184(1): 82. doi: 10.1503/cmaj.110715.
16.
McCann B, O’Gara A. Tension viscerothorax: an important differential for tension pneumothorax. Emerg Med J. 2005; 22(3): 220–221. doi: 10.1136/emj.2003.008367.
17.
Schummer W. Hiatal hernia mimicking heart problems. BMJ Case Rep. 2017. doi:10.1136/bcr-2017-220508.
18.
Hokamaki J, Kawano H, Miyamoto S, et al. Dynamic electrocardiographic changes due to cardiac compression by a giant hiatal hernia. Intern Med. 2005; 44(2): 136–140. doi: 10.2169/internalmedicine.44.136.
19.
Zanini G, Seresini G, Racheli M, et al. Electrocardiographic changes in hiatal hernia: a case report. Cases J. 2009; 2: 8278. doi: 10.4076/1757-1626-2-8278.
20.
Gard JJ, Bader W, Enriquez-Sarano M, et al. Uncommon cause of ST elevation. Circulation 2011; 123(9); 259–261. doi: 10.1161/CIRCULATIONAHA.110.002477.
21.
Basir B, Safadi B, Kovacs RJ, at al. A Rare Case of Transient Inferior ST Segment Elevation. Heart Views 2013; 14(3): 117–120. doi: 10.4103/1995-705X.125928.
22.
Narala K, Banga S, Hsu M, et al. Hiatal hernia mimicking ST elevation myocardial infarction. Cardiology 2014; 129(4): 258–261. doi: 10.1159/000367778.
23.
Rossington JA, Balerdi M, Hoye AJ. Noncardiac pathology exposed at coronary angiography for ST-segment elevation. JACC Cardiovasc Interv. 2014; 7(5): 41–43. doi: 10.1016/j.jcin.2013.07.025.
24.
Kakarala K, Edriss H, Nugent K. Gastropericardial fistula as a delayed complication of a Nissen fundoplication. Proc (Bayl Univ Med Cent) 2015; 28(4): 478–481. doi: 10.1080/08998280.2015.11929314.
25.
Harada K, Tamura U, Ichimiya C, et al. Left ventricular obstruction caused by a large hiatal hernia. Echocardiography 2017; 34(8): 1254–1256. doi: 10.1111/echo.13563.
26.
Rubini Gimenez M, Gonzalez Jurka L, Zellweger MJ, et al. A case report of a giant hiatal hernia mimicking an ST-elevation myocardial infarction. Eur Heart J Case Rep. 2019; 3(3): 138. doi: 10.1093/ehjcr/ytz138.
27.
Arvind A, Niec R, Hajifathalian K, et al. Hiatal Hernia Presenting with Recurrent Non-ST Elevation Myocardial Infarction and Cardiac Tamponade. ACG Case Rep J. 2019; 6(12): e00278. doi: 10.14309/crj.0000000000000278.
28.
Gürgün C, Yavuzgil O, Akín M. Images in cardiology. Paraoesophageal hiatal hernia as a rare cause of dyspnoea. Heart. 2002; 87(3): 275. doi:10.1136/heart.87.3.275.
29.
Duygu H, Ozerkan F, Saygi S, et al. Persistent atrial fibrillation associated with gastroesophageal reflux accompanied by hiatal hernia. Anadolu Kardiyol Derg. 2008; 8(2): 164–165.
30.
Cristian DA, Constantin AS, Barbu M, et al. Paroxysmal postprandial atrial fibrilation suppressed by laparoscopic repair of a giant paraesophageal hernia compressing the left atrium. J Gastrointestin Liver Dis. 2015; 24(1): 113–116. doi: 10.15403/jgld.2014.1121.dac.
31.
Schilling RJ, Kaye GC. Paroxysmal atrial flutter suppressed by repair of a large paraesophageal hernia. Pacing Clin Electrophysiol. 1998; 21(6): 1303–1305. doi: 10.1111/j.1540-8159.1998.tb00191.x.
32.
Patel A, Shah R, Nadavaram S, et al. Hiatal hernia squeezing the heart to flutter. Am J Emerg Med. 2014; 32(4): 392. doi: 10.1016/j.ajem.2013.10.024.
33.
Tursi A, Cuoco L. Recurrent supraventricular extrasystolia due to retrocardiac stomach. Am J Gastroenterol. 2001; 96(1): 257–258. doi:10.1111/j.1572-0241.2001.03494.x.
34.
Gnanenthiran SR, Naoum C, Kilborn MJ, et al. Posterior cardiac compression from a large hiatal hernia – A novel cause of ventricular tachycardia. HeartRhythm Case Rep. 2018; 4(8): 362–366. doi:10.1016/j.hrcr.2018.05.003.
35.
Gleadle J, Dennis M. A thrilling case of hiatus hernia. Postgrad Med J. 1989; 65(769): 832–834. doi: 10.1136/pgmj.65.769.832.
36.
Roy RR, Sagar S, Bunch TJ, et al. Hiatal Hernia Is Associated With an Increased Prevalence of Atrial Fibrillation in Young Patients. J Atr Fibrillation. 2013; 6(2): 894. doi: 10.4022/jafib.894.
37.
Patel N, Ibrahim S, Shah J, et al. Deglutition syncope. Proc (Bayl Univ Med Cent) 2017; 30(3): 293–294. doi: 10.1080/08998280.2017.11929619.
38.
Kounis NG, Zavras GM, Kitrou MP, et al. Unusual electrocardiographic manifestations in conditions with increased intrathoracic pressure. Acta Cardiol. 1988; 43(6): 653–661.
39.
Maruyama T, Fukata M, Akashi K. Association of atrial fibrillation and gastroesophageal reflux disease: Natural and therapeutic linkage of the two common diseases. J Arrhythm. 2018; 35(1): 43–51. doi:10.1002/joa3.12125.
40.
Singh M, Sood A, Rehman MU, et al. Elevated Hemi-diaphragms as a Cause of ST-segment Elevation: A case report and review of literature. J Electrocardiol. 2017; 50(5): 681–685. doi: 10.1016/j.jelectrocard.2017.04.001.
41.
Khouzam RN, Akhtar A, Minderman D, et al. Echocardiographic aspects of hiatal hernia: A review. J Clin Ultrasound. 2007; 35(4): 196–203. doi: 10.1002/jcu.20312.
42.
Yang SS, Wagner P, Dennis C. Images in cardiovascular medicine. Hiatal hernia masquerading as left atrial mass. Circulation. 1996; 93(4): 836. doi: 10.1161/01.cir.93.4.836.
43.
Oishi Y, Ishimoto T, Nagase N, et al. Syncope upon swallowing caused by an esophageal hiatal hernia compressing the left atrium: a case report. Echocardiography 2004; 21(1): 61–64. doi: 10.1111/j.0742-2822.2004.03005.x.
44.
Lim HS, Leong DP, Alasady M. Massive hiatus hernia mimicking a left atrial mass. Heart Lung Circ. 2013; 22(10): 875–876. doi: 10.1016/j.hlc.2013.01.001.
45.
Koskinas KC, Oikonomou K, Karapatsoudi E, et al. Echocardiographic manifestation of hiatus hernia simulating a left atrial mass: case report. Cardiovasc Ultrasound. 2008; 6: 46. doi: 10.1186/1476-7120-6-46.
46.
Innasimuthu AL, Rao GK, Chuah S. Left atrial compression by a hiatus hernia. J Cardiovasc Comput Tomogr. 2007; 1(2): 106–107. doi: 10.1016/j.jcct.2007.04.010.
47.
Brown A, Austin D, Kanakala V. Cardiac compression due to gastric volvulus: an unusual cause of chest pain. BMJ Case Rep. 2017. doi:10.1136/bcr-2017-219595.
48.
Kim SH, Kim MG, Kim SJ, et al. Unusual Diaphragmatic Hernias Mimicking Cardiac Masses. J Cardiovasc Ultrasound. 2015; 23(2): 107–112. doi: 10.4250/jcu.2015.23.2.107.
49.
Matar A, Mroue J, Camporesi E, et al. Large Hiatal Hernia Compressing the Heart. Am J Cardiol. 2016; 117(3): 483–484.
50.
Gupta M, Nanda NC, Inamdar V. Two- and three-dimensional transthoracic echocardiographic assessment of hiatal hernia. Echocardiography. 2008; 25(7): 790–793. doi: 10.1111/j.1540-8175.2008.00702.x.
51.
Torres D, Parrinello G, Cardillo M, et al. Large hiatal hernia at chest radiography in a woman with cardiorespiratory symptoms. Am J Emerg Med. 2012; 30(9): 2103.e1–2103.e21033. doi: 10.1016/j.ajem.2012.03.009.
52.
Palios J, Clements S.Jr, Lerakis S. Chest pain due to hiatal hernia mimicking as cardiac mass. Acute Card Care. 2014; 16(2): 88–89. doi:10.3109/17482941.2014.889313.
53.
Langberg S, Favot M. Hiatal Hernia Mimicking Aortic Aneurysm on Point-of-care Echocardiography. Clin Pract Cases Emerg Med. 2017; 1(4): 419–420. doi: 10.5811/cpcem.2017.6.33450.
54.
Sonsöz MR, Gören MT, Bugra Z. A suspicious left atrial mass in a patient with stroke: Hiatal hernia. Anatol J Cardiol. 2019; 22(2): 5002. doi: 10.14744/AnatolJCardiol.2019.62678.
55.
D’Cruz IA, Hancock HL. Echocardiographic characteristics of diaphragmatic hiatus hernia. Am J Cardiol. 1995; 75(4): 308–310. doi: 10.1016/0002-9149(95)80049-x.
56.
Smelley M, Lang RM. Large mass impinging on the left atrium: diagnostic value of a new cocktail. J Am Soc Echocardiogr. 2007; 20(12). doi: 10.1016/j.echo.2007.05.010.
57.
Bowles MH, Lipman RE. Hiatal hernia: the “X” factor in transesophageal echocardiography. J Am Soc Echocardiogr. 1993; 6(6): 631–633. doi: 10.1016/s0894-7317(14)80184-3.
58.
Frans EE, Nanda NC, Patel V, et al. Transesophageal two-dimensional echocardiographic identification of hiatal hernia. Echocardiography. 2005; 22(6): 533–535. doi:10.1111/j.1540-8175.2005.50017.x.
59.
Siu CW, Jim MH, Ho HH, et al. Recurrent acute heart failure caused by sliding hiatus hernia. Postgrad Med J. 2005; 81(954): 268–269. doi: 10.1136/pgmj.2004.023416.
60.
Ishibashi Y, Nishigami K, Watanabe M, et al. Heart failure induced by the restrictive left ventricle due to hiatus hernia. J Echocardiogr. 2013; 11(3): 103–105. doi: 10.1007/s12574-013-0177-x.
61.
Matsuda M, Okutani R, Ueda M, et al. A large hiatal hernia exacerbated after aortic surgery: an unusual cause of heart failure. J Cardiothorac Vasc Anesth. 2012; 26(4): 41–42. doi: 10.1053/j.jvca.2012.02.011.
62.
Kawabe K, Tsutsumi N, Ikejiri K. Pseudo-heart Failure Due to a Large Hiatal Hernia. Intern Med. 2019; 58(23): 3483–3484. doi: 10.2169/internalmedicine.3167-19.
63.
Malik SB, Chen N, Parker RA, et al. Transthoracic Echocardiography: Pitfalls and Limitations as Delineated at Cardiac CT and MR Imaging. 2017; 37(2): 383–406. doi: 10.1148/rg.2017160105.
64.
Devbhandari MP, Khan MA, Hooper TL. Cardiac compression following cardiac surgery due to unrecognised hiatus hernia. Eur J Cardiothorac Surg. 2007; 32(5): 813–815. doi: 10.1016/j.ejcts.2007.08.002.
65.
Papoulidis P, Beatty JW, Dandekar U. Hiatal hernia causing extra-pericardial tamponade after coronary bypass surgery. Interact Cardiovasc Thorac Surg. 2014; 19(4): 716–717. doi: 10.1093/icvts/ivu215.
66.
Sobczyk D, Darocha T, Gałązkowski R, et al. Echocardiography Is Essential in Detection of Cardiac Tamponade Due to Sliding Hiatal Hernia. J Cardiothorac Vasc Anesth. 2015; 29(5): 60–61. doi: 10.1053/j.jvca.2015.04.008.
67.
Saito H, Miyazaki T, Sohda M, et al. Postprandial cardiogenic syncope caused by gastric polyp-induced pyloric obstruction in an elderly woman with a giant hiatal hernia: a case report. Surg Case Rep. 2017; 3(1): 124. doi: 10.1186/s40792-017-0403-2.
68.
Vanerio G. Syncope caused by huge hiatal hernia. Case Rep Cardiol. 2011; 560734. doi: 10.1155/2011/560734.
69.
Coolidge AM, Czerniach D, Wiener DC. Intestinal Tamponade. Ann Thorac Surg. 2019; 108(3): 193–194. doi: 10.1016/j.athoracsur.2019.01.048.
70.
Oishi Y, Ishimoto T, Nagase N, et al. Syncope upon swallowing caused by an esophageal hiatal hernia compressing the left atrium: a case report. Echocardiography. 2004; 21(1): 61–64. doi: 10.1111/j.0742-2822.2004.03005.x.
71.
Maekawa T, Suematsu M, Shimada T, et al. Unusual swallow syncope caused by huge hiatal hernia. Intern Med. 2002; 41(3): 199–201. doi: 10.2169/internalmedicine.41.199.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.