Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Functional ability of the elderly and related factors in the Subcarpathian Region
1
Laboratory of Clinical Skills, Chair of Nursing Development, Faculty of Health Sciences, Medical University, Lublin, Poland
2
Department of Nursing, State University of Applied Sciences, Krosno, Poland
3
Faculty of Health Sciences, School of Higher Education, Radom, Poland
4
Postgraduate Studies Centre, Medical College, University of Information Technology and Management, Rzeszów, Poland
5
Department of Fundamentals of Nursing, Chair of Nursing Development, Faculty of Health Sciences, Medical University,
Lublin, Poland
Corresponding author
Wiesław Marian Fidecki
Laboratory of Clinical Skills, Chair of Nursing Development, Faculty of Health Sciences,, Medical University of Lublin, Staszica 4-6, 20-059, Lublin, Poland
Laboratory of Clinical Skills, Chair of Nursing Development, Faculty of Health Sciences,, Medical University of Lublin, Staszica 4-6, 20-059, Lublin, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Functional ability is the ability to independently perform basic life activities, such as moving, eating, controlling the physiological functions of the body, and maintaining body hygiene. Functional ability is measured by the living environment’s degree of independence and self-reliance. The Activities of Daily Living (ADL) is mainly based on physical and health factors, while the Instrumental Activities of Daily Living (IADL) is more closely related to psychosocial and cognitive resources. The aim of the study was to assess functional fitness and its determinants among seniors from the Subcarpathian Region.
Material and methods:
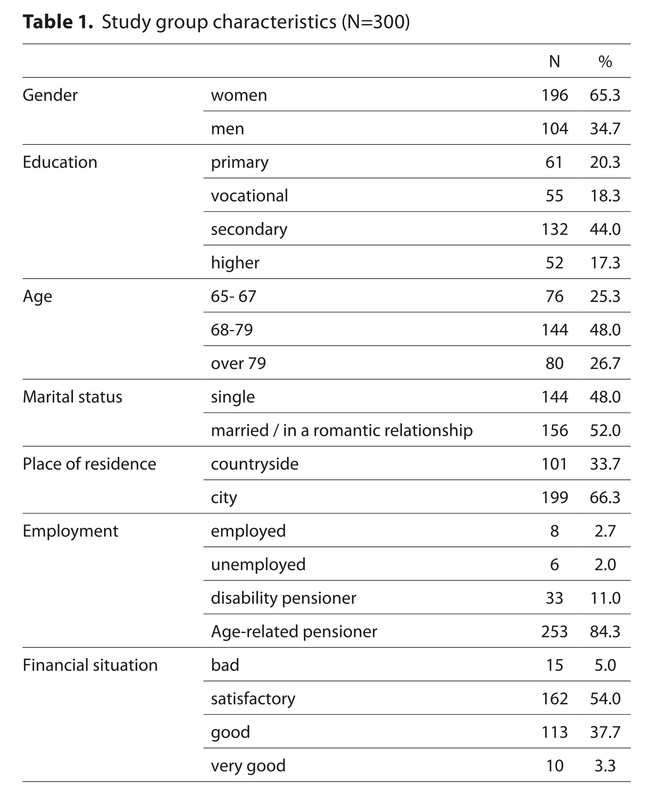
The study was conducted in a group of 300 seniors in the Subcarpathian Region. The study used two standardized research tools: The Lawton Instrumental Activities of Daily Living (IADL) and Scale and the Up and Go Test.
Results:
The functional status of the elderly in terms of instrumental daily activities totalled 21.08; median – 24 points; interquartile range – 5.75 points. Timed Up and Go Test enabled evaluation of the risk of falls in the research group (a high score equals a higher risk of falls). The average score was 19.07 seconds, with a median of 15.25 seconds and an interquartile range of 927 seconds. The risk of falls proved to be moderate with nearly half of the respondents – 46.7%, and high – 25%.
Conclusions:
The examined group of seniors showed a relatively good level of functional fitness in terms of instrumental activities of daily living. At the same time, however, there was a relatively high risk of falls. The subjects’ functional fitness level was differentiated by education, age, place of residence, professional status, and financial situation. Interdependencies were found between the level of education, age, marital status, professional status and the risk of falls.
Functional ability is the ability to independently perform basic life activities, such as moving, eating, controlling the physiological functions of the body, and maintaining body hygiene. Functional ability is measured by the living environment’s degree of independence and self-reliance. The Activities of Daily Living (ADL) is mainly based on physical and health factors, while the Instrumental Activities of Daily Living (IADL) is more closely related to psychosocial and cognitive resources. The aim of the study was to assess functional fitness and its determinants among seniors from the Subcarpathian Region.
Material and methods:
The study was conducted in a group of 300 seniors in the Subcarpathian Region. The study used two standardized research tools: The Lawton Instrumental Activities of Daily Living (IADL) and Scale and the Up and Go Test.
Results:
The functional status of the elderly in terms of instrumental daily activities totalled 21.08; median – 24 points; interquartile range – 5.75 points. Timed Up and Go Test enabled evaluation of the risk of falls in the research group (a high score equals a higher risk of falls). The average score was 19.07 seconds, with a median of 15.25 seconds and an interquartile range of 927 seconds. The risk of falls proved to be moderate with nearly half of the respondents – 46.7%, and high – 25%.
Conclusions:
The examined group of seniors showed a relatively good level of functional fitness in terms of instrumental activities of daily living. At the same time, however, there was a relatively high risk of falls. The subjects’ functional fitness level was differentiated by education, age, place of residence, professional status, and financial situation. Interdependencies were found between the level of education, age, marital status, professional status and the risk of falls.
ACKNOWLEDGEMENTS
This publication was funded by the Polish Ministry of Education and Science under the project ‘Doskonała Nauka II’, ‘Wsparcie bezpieczeństwa pacjenta przez popularyzację dowodów naukowych w praktyce zawodów medycznych’. Project No. KONF/SP/0265/2023/01.
REFERENCES (25)
1.
Steuden S. Wybrane psychologiczne aspekty procesu starzenia się i starości. In: Cybulski M, Krajewska-Kułak E, Waszkiewicz N, et al, editors. Psychogeriatria. Warszawa: Wyd. PZWL; 2019. p. 299–312.
3.
Kim Y, Park KS, Yoo JI. Associations between the quality of life in sarcopenia measured with the SarQoL® and nutritional status. Health Qual Life Outcomes. 2021;19:28. https://doi.org/10.1186/s12955....
4.
Błędowski P, Grodzicki T, Mossakowska M, et al. Polsenior 2. Badanie poszczególnych obszarów stanu zdrowia osób starszych, w tym jakości życia związanej ze zdrowiem. Gdańsk: Gdański Uniwersytet Medyczny; 2021.
5.
Beltz S, Gloystein S, Litschkoet T, et al. Multivariate analysis of independent determinants of ADL/IADL and quality of life in the elderly. BMC Geriatr. 2022;22:894. https://doi.org/10.1186/s12877....
6.
Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9(3):179–186.
7.
Wizner B, Skalska A, Klich-Rączka A, et al. Ocena stanu funkcjonalnego u osób w starszym wieku. In: Mossakowska M, Więcek A, Błędowski P, editors. Aspekty medyczne, psychologiczne, socjologiczne i ekonomiczne starzenia się ludzi w Polsce. Poznań: Wyd. Med. Termedia; 2012. p. 83–84.
8.
Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Physical Therapy. 2000;80(9):896–903.
9.
Saintrain MVdL, Saintrain SV, de Oliveira Branco JG, et al. Dependence in instrumental activities of daily living and its implications for older adults’ oral health. PLoS ONE. 2021;16(4):e0249275. https://doi.org/10.1371/journa.... pone.0249275\.
10.
Silva TLD, Motta VVD, Garcia WJ, et al. Quality of life and falls in elderly people: a mixed methods study. Rev Bras Enferm. 2021;74(Suppl 2):e20200400. https://doi.org/10.1590/0034-7....
11.
Jalali M, Mojgani P, Saeedi H, et al. The relationship between common foot problems with falls and quality of life in older people. Int J Older People Nurs. 2021;16(6):e12402. https://doi.org/10.1111/opn.12....
12.
Song J, Lee E. Health-related quality of life of elderly women with fall experiences. Int J Environ Res Public Health. 2021;18(15):7804. https://doi.org/10.3390%2Fijer....
13.
Arokiasamy P, Uttamacharya U, Jain K, et al. The impact of multi-morbidity on adult physical and mental health in lowand middle-income countries: what does the study on global ageing and adult health (SAGE) reveal? BMC Med. 2015;13:178.
14.
Verropoulou G, Tsimbos C. Disability trends among older adults in ten European countries over 2004–2013, using various indicators and Survey of Health, Ageing and Retirement in Europe (SHARE) data. Ageing Soc. 2016;37(10):2152–82. https://doi.org/10.1017/S01446....
15.
Wahrendorf M, Reinhardt JD, Siegrist J. Relationships of Disability with Age Among Adults Aged 50 to 85: Evidence from the United States, England and Continental Europe. PLoS One. 2013;8(8):e71893. https://doi.org/10.1371/journa....
16.
Patel R, Srivastava S, Kumar P, et al. Socio-economic inequality in functional disability and impairments with focus on instrumental activity of daily living: a study on older adults in India. BMC Public Health. 2021;21:1541. https://doi.org/10.1186/s12889....
17.
Wróblewska Z, Chmielewski JP, Florek-Łuszczki M, et al. Assessment of functional capacity of the elderly. Ann Agric Environ Med. 2023;30(1):156–163. https://doi.org/:10.26444/aaem....
18.
Lewko J, Kamińska KM, Doroszkiewicz H, et al. Ocena narażenia na upadki a wydolność funkcjonalna wśród osób starszych w środowisku zamieszkania. Probl Piel. 2014;2:159–164.
19.
Chen SW, Chippendale T. Factors associated with IADL independence: implications for OT practice. Scand J Occup Ther. 2017;24(2):109–115. http://dx.doi.org/10.1080/1103....
20.
Dhar M, Kaeley N, Mahala P, et al. The Prevalence and Associated Risk Factors of Fear of Fall in the Elderly: A Hospital-Based, Cross-Sectional Study. Cureus. 2022;14(3):1–8. http://dx.doi.org/10.7759/cure....
21.
Ek S, Rizzuto D, Fratiglioni L, et al. Risk Factors for Injurious Falls in Older Adults: The Role of Sex and Length of Follow-Up. J Am Geriatr Soc. 2019;67:246–253. https://doi.org/10.1111/jgs.15....
22.
Tsai YJ, Yang PY, Yang YC, et al. Prevalence and risk factors of falls among community-dwelling older people: results from three consecutive waves of the national health interview survey in Taiwan. BMC Geriatr. 2020;20:529. https://doi.org/10.1186/s12877....
23.
Talarska D, Strugała M, Szewczyczak M, et al. Is independence of older adults safe considering the risk of falls? BMC Geriatr. 2017;17:66. https://doi.org/10.1186/s12877....
24.
Zhang L, Zhihong D, Liya Q, et al. Falls and risk factors of falls for urban and rural community-dwelling older adults in China BMC Geriatr. 2019;19:379. https://doi.org/10.1186/s12877....
25.
Masugi Y, Kawai H, Ejiri M, et al. Early strong predictors of decline in instrumental activities of daily living in community-dwelling older Japanese people. PLoS ONE 2022;17(4):e0266614. https://doi.org/10.1371/journa....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.