Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Effect of SARS-CoV-2 infection on out-of-hospital cardiac arrest outcomes – systematic review and meta-analysis
1
Polish Society of Disaster Medicine, Warsaw, Poland
2
Baylor College of Medicine, Houston, United States
3
Maria Sklodowska-Curie Medical Academy, Warsaw, Poland
4
York University, Toronto, ON, Canada
5
Bezmialem Vakif University, Fatih/Istanbul, Turkey
6
University Zürich, Zürich, Switzerland
7
International Academy of Ecology and Medicine, Kyiv, Ukraine
8
Institute of Rural Health, Lublin, Poland
9
Institute of Environmental Protection – National Research Institute, Warsaw, Poland
10
Medical University, Lublin, Poland
Ann Agric Environ Med. 2023;30(2):369-375
KEYWORDS
TOPICS
Biological agents posing occupational risk in agriculture, forestry, food industry and wood industry and diseases caused by these agents (zoonoses, allergic and immunotoxic diseases)State of the health of rural communities depending on various factors: social factors, accessibility of medical care, etc.
ABSTRACT
Introduction and objective:
The COVID-19 pandemic caused by the SARS-CoV-2 virus has recently presented the world with an unprecedented challenge. The purpose of this systematic review and meta-analysis is to investigate the relationship between SARS-CoV-2 infection and out-of-hospital cardiac arrest (OHCA) by comparing data from infected and non-infected individuals. The study adds to our understanding of the broader effects of the pandemic on public health and emergency care by examining the influence of COVID-19 on OHCA.
Material and methods:
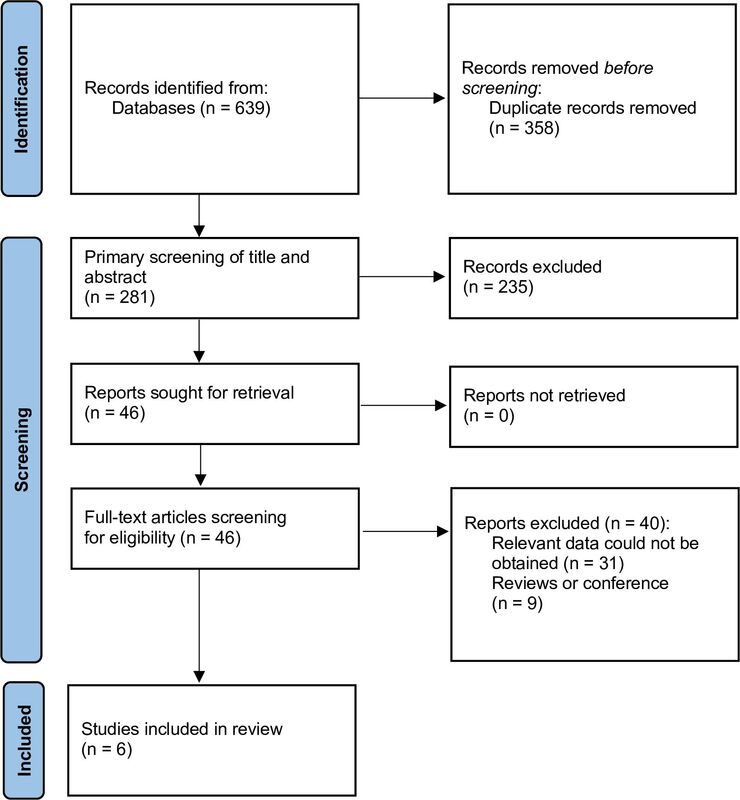
A comprehensive systematic literature search was performed using PubMed, EMBASE, Scopus, Web of Science, the Cochrane Library and Google Scholar from 1 January 2020 – 24 May 2023. Incidence rates and odds ratios (ORs) or mean differences (MDs) with 95% confidence intervals (CIs) for risk factors were recorded from individual studies, and random-effects inverse variance modelling used to generate pooled estimates.
Results:
Six studies, involving 5,523 patients, met the criteria for inclusion in the meta-analysis. Survival to hospital admission, defined as admission to the emergency department with sustained return of spontaneous circulation (ROSC), among patients with and without on-going infection was 12.2% and 20.1%, respectively (p=0.09). Survival to hospital discharge/30-day survival rate was 0.8% vs. 6.2% (p<0.001). Two studies reported survival to hospital discharge in good neurological condition; however, the difference was not statistically significant (2.1% vs. 1.8%; p=0.37).
Conclusions:
Compared to the non-infected patients, the ongoing SARS-CoV-2 infection was associated with worse OHCA outcomes.
The COVID-19 pandemic caused by the SARS-CoV-2 virus has recently presented the world with an unprecedented challenge. The purpose of this systematic review and meta-analysis is to investigate the relationship between SARS-CoV-2 infection and out-of-hospital cardiac arrest (OHCA) by comparing data from infected and non-infected individuals. The study adds to our understanding of the broader effects of the pandemic on public health and emergency care by examining the influence of COVID-19 on OHCA.
Material and methods:
A comprehensive systematic literature search was performed using PubMed, EMBASE, Scopus, Web of Science, the Cochrane Library and Google Scholar from 1 January 2020 – 24 May 2023. Incidence rates and odds ratios (ORs) or mean differences (MDs) with 95% confidence intervals (CIs) for risk factors were recorded from individual studies, and random-effects inverse variance modelling used to generate pooled estimates.
Results:
Six studies, involving 5,523 patients, met the criteria for inclusion in the meta-analysis. Survival to hospital admission, defined as admission to the emergency department with sustained return of spontaneous circulation (ROSC), among patients with and without on-going infection was 12.2% and 20.1%, respectively (p=0.09). Survival to hospital discharge/30-day survival rate was 0.8% vs. 6.2% (p<0.001). Two studies reported survival to hospital discharge in good neurological condition; however, the difference was not statistically significant (2.1% vs. 1.8%; p=0.37).
Conclusions:
Compared to the non-infected patients, the ongoing SARS-CoV-2 infection was associated with worse OHCA outcomes.
ABBREVIATIONS
ACLS: advanced cardiovascular life support; ARDS: acute respiratory distress syndrome; CI: confidence interval; CPC: Cerebral Performance Categories; CPR: cardiopulmonary resuscitation; CVD: cardiovascular disease; EMS: emergency medical service; IHCA: in-hospital cardiac arrest; MD: mean difference; NOS: Newcastle Ottawa Scale; OHCA: out-of-hospital cardiac arrest; OR: odds ratio; ROSC: return of spontaneous circulation; PPE: personal protective equipment; PRISMA: preferred reporting items for systematic reviews and meta-analysis; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2; SHA: survival to hospital admission; SHD: survival to hospital discharge; VTE: venous thromboembolism
ACKNOWLEDGEMENTS
The study was supported by the European Research Council (ERC) Research Net and by the Polish Society of Disaster Medicine in Warsaw, Poland.
REFERENCES (76)
1.
Dzieciatkowski T, Szarpak L, Filipiak KJ, et al. COVID-19 challenge for modern medicine. Cardiol J. 2020; 27(2):175–183. https://doi.org/10.5603/CJ. a2020.0055.
2.
Nessler K, Van Poel E, Willems S, et al. The response of primary care practices in rural and urban settings in Poland to the challenges of the COVID-19 pandemic. Ann Agric Environ Med. 2022;29(4):575–581. https://doi.org/10.26444/aaem/....
3.
COVID-19 Excess Mortality Collaborators. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet. 2022 Apr 16;399(10334):1513-1536. https://doi.org/10.1016/S0140-....
4.
Karim S, Eidizadeh M, Kazemi M, et al. Risk factors related to COVID-19 survival and mortality: a cross-sectional-descriptive study in regional COVID-19 registry in Fasa, Iran. Disaster Emerg Med J. 2023; https://doi.org/10.5603/DEMJ.a....
5.
Gibson PG, Qin L, Puah SH. COVID-19 acute respiratory distress syndrome (ARDS): clinical features and differences from typical pre-COVID-19 ARDS. Med J Aust. 2020 Jul;213(2):54-56.e1. https://doi.org/10.5694/mja2.5....
6.
Matuszewski M, Ładny J, Rafique Z, et al. Prediction value of soluble urokinase plasminogen activator receptor (suPAR) in COVID-19 patients – a systematic review and meta-analysis. Ann Agric Environ Med. 2023;30(1):142–147. https://doi.org/10.26444/aaem/....
7.
Szarpak Ł, Nowak B, Kosior Det al. Cytokines as predictors of COVID-19 severity: evidence from a meta-analysis. Pol Arch Intern Med. 2021 Jan 29;131(1):98-99. https://doi.org/10.20452/pamw.....
8.
Matuszewski M, Pruc M, Szarpak L, et al. A comprehensive review and meta-analysis of the relationships between interleukin-7 levels and COVID-19 severity. J Health Soc Sci. 2023;8(1):33-44. https://doi.org/10.19204/2023/....
9.
Schmidt W, Jóźwiak B, Czabajska Z, et al. On-admission laboratory predictors for developing critical COVID-19 during hospitalization – a multivariable logistic regression model. Ann Agric Environ Med. 2022;29(2):274–280. https://doi.org/10.26444/aaem/....
10.
Matuszewski M, Afolabi AA, Ilesanmi OS, et al. Associations between Interleukin-4 and COVID-19 severity: A systematic review and meta-analysis. J Health Soc Sci. 2022;7(4):381-396. https://doi.org/10.19204/2022/....
11.
Yaman E, Demirel B, Yilmaz A, et al. Retrospective evaluation of laboratory findings of suspected paediatric COVID-19 patients with positive and negative RT-PCR. Disaster Emerg Med J. 2021;6(3):97-103. https://doi.org/10.5603/DEMJ.a....
12.
Montazersaheb S, Hosseiniyan Khatibi SM, Hejazi MS, et al. COVID-19 infection: an overview on cytokine storm and related interventions. Virol J. 2022 May 26;19(1):92. https://doi.org/10.1186/s12985....
13.
Olszewska-Parasiewicz J, Szarpak Ł, et al. Statins in COVID-19 Therapy. Life (Basel). 2021 Jun 16;11(6):565. https://doi.org/10.3390/life11....
14.
Dubey L, Dorosh O, Dubey N, et al. COVID-19-induced coagulopathy: Experience, achievements, prospects. Cardiol J. 2023 Jan 2. https://doi.org/10.5603/CJ.a20....
15.
Levy JH, Iba T, Olson LB, Corey KM, Ghadimi K, Connors JM. COVID-19: Thrombosis, thromboinflammation, and anticoagulation considerations. Int J Lab Hematol. 2021;43 Suppl 1(Suppl 1):29-35. https://doi.org/10.1111/ijlh.1....
16.
Katsoularis I, Fonseca-Rodríguez O, Farrington P, et al. Risk of acute myocardial infarction and ischaemic stroke following COVID-19 in Sweden: a self-controlled case series and matched cohort study. Lancet 2021;398:599–607.doi:10.1016/S0140-6736(21)00896-5 pmid:http://www.ncbi.nlm.nih.gov/pu....
17.
Wang W, Wang CY, Wang SI, Wei JC. Long-term cardiovascular outcomes in COVID-19 survivors among non-vaccinated population: A retrospective cohort study from the TriNetX US collaborative networks. E Clin Med. 2022 Nov;53:101619. doi: 10.1016/j.eclinm.2022.101619. Epub 2022 Aug.
18.
Nucera G, Chirico F, Rafique Z, Gilis-Malinowska N, Gasecka A, Litvinova N, Wang B, Ilesanmi OS, Pruc M, Jaguszewski MJ, Szarpak L. Need to update cardiological guidelines to prevent COVID-19 related myocardial infarction and ischemic stroke. Cardiol J. 2022;29(1):174-175. doi: 10.5603/CJ.a2021.0120. Epub 2021 Oct 13. PMID: 34642925; PMCID: PMC8890413.
19.
Bielski K, Szarpak A, Jaguszewski MJ, Kopiec T, Smereka J, Gasecka A, Wolak P, Nowak-Starz G, Chmielewski J, Rafique Z, Peacock FW, Szarpak L. The Influence of COVID-19 on Out-Hospital Cardiac Arrest Survival Outcomes: An Updated Systematic Review and Meta-Analysis. J Clin Med. 2021 Nov 27;10(23):5573. doi: 10.3390/jcm10235573. PMID: 34884289; PMCID: PMC8658174.
20.
Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–87.
21.
Nishiyama, C, Kiguchi, T, Okubo, M, Alihodžić, H, Al-Araji, R, Baldi, E, et al. Three-year trends in out-of-hospital cardiac arrest across the world: second report from the International Liaison Committee on Resuscitation (ILCOR). Resuscitation. (2023) 186:109757. doi: 10.1016/j.resuscitation.2023.10975.
22.
Bielski K, Böttiger BW, Pruc M, et al. Outcomes of audio-instructed and video-instructed dispatcher-assisted cardiopulmonary resuscitation: a systematic review and meta-analysis. Ann Med. 2022 Dec;54(1):464-471. doi: 10.1080/07853890.2022.2032314.
23.
Hallstrom A, Cobb L, Johnson E, Copass M. Cardiopulmonary resuscitation by chest compressions alone or with mouth to mouth ventilation. N Engl J Med. 2000;342(21):1546–53. 10.1056/NEJM200005253422101.
24.
Leung KY, Chu CMM, Lui CT. Exposure-response relationship between COVID-19 incidence rate and incidence and survival of out-of-hospital cardiac arrest (OHCA). Resusc Plus. 2023 Jun;14:100372. doi: 10.1016/j.resplu.2023.100372.
25.
Borkowska MJ, Smereka J, Safiejko K, et al. Out-of-hospital cardiac arrest treated by emergency medical service teams during COVID-19 pandemic: A retrospective cohort study. Cardiol J. 2021;28(1):15-22. doi: 10.5603/CJ.a2020.0135.
26.
Kennedy C, Alqudah Z, Stub D, Anderson D, Nehme Z. The effect of the COVID-19 pandemic on the incidence and survival outcomes of EMS-witnessed out-of-hospital cardiac arrest. Resuscitation. 2023 Jun;187:109770. doi: 10.1016/j.resuscitation.2023.109770.
27.
Meyer-Szary J, Jaguszewski MJ, Smereka J, et al. Impact of COVID-19 on pediatric out-of-hospital cardiac arrest in the Masovian region. Disaster Emerg Med J. 2021;6(4):183-185. DOI: 10.5603/DEMJ.a2021.0028.
28.
Navolokina A, Smereka J, Böttiger BW, et al. The Impact of COVID-19 on Pediatric Cardiac Arrest Outcomes: A Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2023 Jan 8;20(2):1104. doi: 10.3390/ijerph20021104.
29.
Chojecka D, Pytlos J, Zawadka M, et al. How to Maintain Safety and Maximize the Efficacy of Cardiopulmonary Resuscitation in COVID-19 Patients: Insights from the Recent Guidelines. J Clin Med. 2021 Nov 30;10(23):5667. doi: 10.3390/jcm10235667.
30.
Solomon MD, McNulty EJ, Rana JS. The covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693.
31.
Liu CH, Tsai MJ, Hsu CF, Tsai CH, Su YS, Cai DC. The Influence of the COVID-19 Pandemic on Emergency Medical Services to Out-of-Hospital Cardiac Arrests in a Low-Incidence Urban City: An Observational Epidemiological Analysis. Int J Environ Res Public Health. 2023 Feb 3;20(3):2713. doi: 10.3390/ijerph20032713. PMID: 36768079; PMCID: PMC9915115.
32.
Al-Jeabory M, Safiejko K, Bialka S, Pruc M, Gasecka A, Szarpak L. Impact of COVID-19 on bystander cardiopulmonary resuscitation in out-of-hospital cardiac arrest: Is it as bad as we think? Cardiol J. 2020;27(6):884-885. doi: 10.5603/CJ.a2020.0179.
33.
Kurosaki H, Okumura K, Nunokawa C, Yao S, Murasaka K, Inaba H. Effects of the 2020 COVID-19 pandemic on outcomes of out-of-hospital cardiac arrest and bystander resuscitation efforts: a nationwide cohort study in Japan. Eur J Emerg Med. 2023 Jun 1;30(3):171-178. doi: 10.1097/MEJ.0000000000001014.
34.
Fazel MF, Mohamad MHN, Sahar MA, Juliana N, Abu IF, Das S. Readiness of Bystander Cardiopulmonary Resuscitation (BCPR) during the COVID-19 Pandemic: A Review. Int J Environ Res Public Health. 2022 Sep 2;19(17):10968. doi: 10.3390/ijerph191710968. PMID: 36078684; PMCID: PMC9518324.
35.
Ventura CAI, Denton EE, David JA, Schoenfelder BJ, Mela L, Lumia RP, Rudi RB, Haldar B. Emergency Medical Services Prehospital Response to the COVID-19 Pandemic in the US: A Brief Literature Review. Open Access Emerg Med. 2022 May 30;14:249-272. doi: 10.2147/OAEM.S366006. PMID: 35669176; PMCID: PMC9165654.
36.
McCann-Pineo M, Li T, Barbara P, Levinsky B, Debono J, Berkowitz J. Utility of Emergency Medical Dispatch (EMD) Telephone Screening in Identifying COVID-19 Positive Patients. Prehosp Emerg Care. 2021 Jul 12:1-10. doi: 10.1080/10903127.2021.1939817. Epub ahead of print. PMID: 34115573.
37.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002. https://doi.org/10.1002/sim.11....
38.
Baert V, Jaeger D, Hubert H, Lascarrou JB, Debaty G, Chouihed T, Javaudin F; GR-RéAC. Assessment of changes in cardiopulmonary resuscitation practices and outcomes on 1005 victims of out-of-hospital cardiac arrest during the COVID-19 outbreak: registry-based study. Scand J Trauma Resusc Emerg Med. 2020 Dec 18;28(1):119. doi: 10.1186/s13049-020-00813-x.
39.
Baldi E, Sechi GM, Mare C, et al. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020 Jun 1;41(32):3045-3054. doi: 10.1093/eurheartj/ehaa508.
40.
Cho JW, Jung H, Lee MJ, et al. Preparedness of personal protective equipment and implementation of new CPR strategies for patients with out-of-hospital cardiac arrest in the COVID-19 era. Resusc Plus. 2020 Sep;3:100015. doi: 10.1016/j.resplu.2020.100015.
41.
Fothergill RT, Smith AL, Wrigley F, Perkins GD. Out-of-Hospital Cardiac Arrest in London during the COVID-19 pandemic. Resusc Plus. 2021 Mar;5:100066. doi: 10.1016/j.resplu.2020.100066.
42.
Navalpotro-Pascual JM, Fernández Pérez C, Peinado Vallejo FA, et al. Caseload and cardiopulmonary arrest management by an out-of-hospital emergency service during the COVID-19 pandemic. Emergencias. 2021;33(2):100-106.
43.
Sultanian P, Lundgren P, Strömsöe A, et al. Cardiac arrest in COVID-19: characteristics and outcomes of in- and out-of-hospital cardiac arrest. A report from the Swedish Registry for Cardiopulmonary Resuscitation. Eur Heart J. 2021 Mar 14;42(11):1094-1106. doi: 10.1093/eurheartj/ehaa1067.
44.
Scquizzato T, Landoni G, Scandroglio AM, Franco A, Calabrò MG, Paoli A, D'Amico F, Yavorovskiy A, Zangrillo A. Outcomes of out-of-hospital cardiac arrest in patients with SARS-CoV-2 infection: a systematic review and meta-analysis. Eur J Emerg Med. 2021 Dec 1;28(6):423-431. doi: 10.1097/MEJ.0000000000000878.
45.
Borkowska MJ, Jaguszewski MJ, Koda M, et al. Impact of Coronavirus Disease 2019 on Out-of-Hospital Cardiac Arrest Survival Rate: A Systematic Review with Meta-Analysis. J Clin Med. 2021 Mar 15;10(6):1209. doi: 10.3390/jcm10061209.
46.
Teoh SE, Masuda Y, Tan DJH, Liu N, Morrison LJ, Ong MEH, Blewer AL, Ho AFW. Impact of the COVID-19 pandemic on the epidemiology of out-of-hospital cardiac arrest: a systematic review and meta-analysis. Ann Intensive Care. 2021 Dec 7;11(1):169. doi: 10.1186/s13613-021-00957-8.
47.
Lim ZJ, Ponnapa Reddy M, Afroz A, Billah B, Shekar K, Subramaniam A. Incidence and outcome of out-of-hospital cardiac arrests in the COVID-19 era: A systematic review and meta-analysis. Resuscitation. 2020 Dec;157:248-258. doi: 10.1016/j.resuscitation.2020.10.025.
48.
Smereka J, Szarpak L. COVID 19 a challenge for emergency medicine and every health care professional. Am J Emerg Med. 2020 Oct;38(10):2232-2233. doi: 10.1016/j.ajem.2020.03.038.
49.
Garcia-Castrillo L, Petrino R, Leach R, Dodt C, Behringer W, Khoury A, Sabbe M. European Society For Emergency Medicine position paper on emergency medical systems' response to COVID-19. Eur J Emerg Med. 2020 Jun;27(3):174-177. doi: 10.1097/MEJ.0000000000000701.
50.
Jachetti A, Colombo G, Brignolo-Ottolini B, Franchi J, Solbiati M, Pecorino Meli M, Bosco P, Costantino G. Emergency department reorganisation to cope with COVID-19 outbreak in Milan university hospital: a time-sensitive challenge. BMC Emerg Med. 2021 Jun 28;21(1):74. doi: 10.1186/s12873-021-00464-w.
51.
Sabbaghi M, Namazinia M, Miri K. Time indices of pre-hospital EMS missions before and during the COVID-19 pandemic: a cross-sectional study in Iran. BMC Emerg Med. 2023 Jan 28;23(1):9. doi: 10.1186/s12873-023-00780-3.
52.
Malysz M, Dabrowski M, Böttiger BW, et al. Resuscitation of the patient with suspected/confirmed COVID-19 when wearing personal protective equipment: A randomized multicenter crossover simulation trial. Cardiol J. 2020;27(5):497-506. doi: 10.5603/CJ.a2020.0068.
53.
Bray J, Cartledge S, Scapigliati A. Bystander CPR in the COVID-19 pandemic. Resusc Plus. 2020 Dec;4:100041. doi: 10.1016/j.resplu.2020.100041.
54.
Mori Y, Iio Y, Aoyama Y, Kozai H, Tanaka M, Aoike M, Kawamura H, Seguchi M, Tsurudome M, Ito M. Willingness and Predictors of Bystander CPR Intervention in the COVID-19 Pandemic: A Survey of Freshmen Enrolled in a Japanese University. Int J Environ Res Public Health. 2022 Nov 27;19(23):15770. doi: 10.3390/ijerph192315770.
55.
April MD. COVID-19 lockdown and bystander cardiopulmonary resuscitation: All associations are local. Resuscitation. 2023 May;186:109780. doi: 10.1016/j.resuscitation.2023.109780.
56.
Babini G, Ristagno G. COVID-19 and reduced bystander cardiopulmonary resuscitation: A thanatophobic attitude leading to increased deaths from cardiac arrest? Acta Anaesthesiol Scand. 2023 Jan;67(1):2-3. doi: 10.1111/aas.14151.
57.
Szarpak L, Pruc M, Nadolny K, Smereka J, Ladny JR. Role of a field hospital in COVID-19 pandemic. Disaster Emerg Med J. 2020;5(4):221-223. DOI: 10.5603/DEMJ.a2020.0046.
58.
Kokudo N, Sugiyama H. Hospital capacity during the COVID-19 pandemic. Glob Health Med. 2021 Apr 30;3(2):56-59. doi: 10.35772/ghm.2021.01031.
59.
Alqahtani F, Khan A, Alowais J, Alaama T, Jokhdar H. Bed Surge Capacity in Saudi Hospitals During the COVID-19 Pandemic. Disaster Med Public Health Prep. 2021 Apr 19:1-7. doi: 10.1017/dmp.2021.117.
60.
Tapia-Conyer R, Valdez-Vázquez RR, Lomelín-Gascón J, et al. Rapid establishment of a dedicated COVID-19 hospital in Mexico city during a public health crisis. Hosp Pract (1995). 2022 Aug;50(3):183-187. doi: 10.1080/21548331.2021.2017644.
61.
Perkins GD, Graesner JT, Semeraro F, et al. European Resuscitation Council Guidelines 2021: Executive summary. Resuscitation. 2021 Apr;161:1-60. doi: 10.1016/j.resuscitation.2021.02.003.
62.
Bhardwaj A, Alwakeel M, Duggal A, Abi Fadel F, Abella BS. Post resuscitation myocardial dysfunction and echocardiographic characteristics following COVID-19 cardiac arrest. Resuscitation. 2022 Apr;173:57-58. doi: 10.1016/j.resuscitation.2022.02.009.
63.
Tajbakhsh A, Gheibi Hayat SM, Taghizadeh H, Akbari A, Inabadi M, Savardashtaki A, Johnston TP, Sahebkar A. COVID-19 and cardiac injury: clinical manifestations, biomarkers, mechanisms, diagnosis, treatment, and follow up. Expert Rev Anti Infect Ther. 2021 Mar;19(3):345-357. doi: 10.1080/14787210.2020.1822737.
64.
Giustino G, Croft LB, Stefanini GG, et al. Characterization of Myocardial Injury in Patients With COVID-19. J Am Coll Cardiol. 2020 Nov 3;76(18):2043-2055. doi: 10.1016/j.jacc.2020.08.069.
65.
Zhang X, Wang B, Geng T, et al. Causal associations between COVID-19 and atrial fibrillation: A bidirectional Mendelian randomization study. Nutr Metab Cardiovasc Dis. 2022 Apr;32(4):1001-1009. doi: 10.1016/j.numecd.2021.11.010.
66.
Szarpak L, Pruc M, Filipiak KJ, et al. Myocarditis: A complication of COVID-19 and long-COVID-19 syndrome as a serious threat in modern cardiology. Cardiol J. 2022;29(1):178-179. doi: 10.5603/CJ.a2021.0155.
67.
Patone M, Mei XW, Handunnetthi L, et al. Risks of myocarditis, pericarditis, and cardiac arrhythmias associated with COVID-19 vaccination or SARS-CoV-2 infection. Nat Med. 2022 Feb;28(2):410-422. doi: 10.1038/s41591-021-01630-0.
68.
Szarpak L, Filipiak KJ, Gasecka A, Pruc M, Drozd A, Jaguszewski MJ. Correlation between takotsubo cardiomyopathy and SARS-CoV-2 infection. Med Hypotheses. 2021 Jan;146:110454. doi: 10.1016/j.mehy.2020.110454.
69.
Dherange P, Lang J, Qian P, Oberfeld B, Sauer WH, Koplan B, Tedrow U. Arrhythmias and COVID-19: A Review. JACC Clin Electrophysiol. 2020 Sep;6(9):1193-1204. doi: 10.1016/j.jacep.2020.08.002.
70.
Denegri A, Sola M, Morelli M, et al. Arrhythmias in COVID-19/SARS-CoV-2 Pneumonia Infection: Prevalence and Implication for Outcomes. J Clin Med. 2022 Mar 7;11(5):1463. doi: 10.3390/jcm11051463.
71.
Szarpak L, Filipiak KJ, Skwarek A, et al. Outcomes and mortality associated with atrial arrhythmias among patients hospitalized with COVID-19: A systematic review and meta-analysis. Cardiol J. 2022;29(1):33-43. doi: 10.5603/CJ.a2021.0167.
72.
Asakura H, Ogawa H. COVID-19-associated coagulopathy and disseminated intravascular coagulation. Int J Hematol. 2021 Jan;113(1):45-57. doi: 10.1007/s12185-020-03029-y.
73.
Dubey L, Lytvyn H, Dorosh O, et al. The pathogenesis of COVID-19: Hypercoagulation and D-dimer in thrombotic complications. J Health Soc Sci 2023, 8, 1, 45-58. Doi: 10.19204/2023/thpt4.
74.
Plášek J, Gumulec J, Máca J, Škarda J, Procházka V, Grézl T, Václavík J. COVID-19 associated coagulopathy: Mechanisms and host-directed treatment. Am J Med Sci. 2022 Jun;363(6):465-475. doi: 10.1016/j.amjms.2021.10.012.
75.
Joffre J, Rodriguez L, Matthay ZA, et al. COVID-19-associated Lung Microvascular Endotheliopathy: A "From the Bench" Perspective. Am J Respir Crit Care Med. 2022 Oct 15;206(8):961-972. doi: 10.1164/rccm.202107-1774OC.
76.
Poor HD. Pulmonary Thrombosis and Thromboembolism in COVID-19. Chest. 2021 Oct;160(4):1471-1480. doi: 10.1016/j.chest.2021.06.016.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.