Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Does gender affect health-related quality of life in patients with type 2 diabetes (ADDQoL) in Central European countries?
1
Department of Clinical Nursing, Faculty of Health Science, Medical University, Wrocław, Poland
2
Faculty of Health Sciences, University of Bielsko-Biala, Poland
3
University Hospital, Ostrava, Czech Republic
4
National Institute of Cardiovascular Diseases, Department of Anaesthesiology and Intensive Care, Bratislava, Slovak
Republic
5
Faculty of Social Science and Health Care, University of Constantinus the Philosopher, Nitra, Slovak Republic
6
School of Health Sciences, Medical University of Silesia, Katowice, Poland
7
Public Health Committee of the Polish Academy of Sciences, V Faculty of Medical Sciences, Polish Academy of Sciences,
Warsaw, Poland
Corresponding author
Agnieszka Młynarska
School of Health Sciences, Medical University of Silesia, 40-635 Katowice, Poland., Poland
School of Health Sciences, Medical University of Silesia, 40-635 Katowice, Poland., Poland
Ann Agric Environ Med. 2023;30(2):296-305
KEYWORDS
TOPICS
ABSTRACT
Objective:
The aim of this study was to compare the impact of type 2 diabetes on quality of life (QoL), taking into account gender differences in relation to individual domains of Diabetes-Related Quality of Life Audit (ADDQoL) in adult men and women in Poland, the Czech Republic and Republic of Slovakia.
Material and methods:
The participants were 608 patients from the three countries, of whom 278 were women and 330 men with type 2 diabetes mellitus. The tool used was the Audit of Diabetes-Dependent Quality of Life (ADDQoL).
Results:
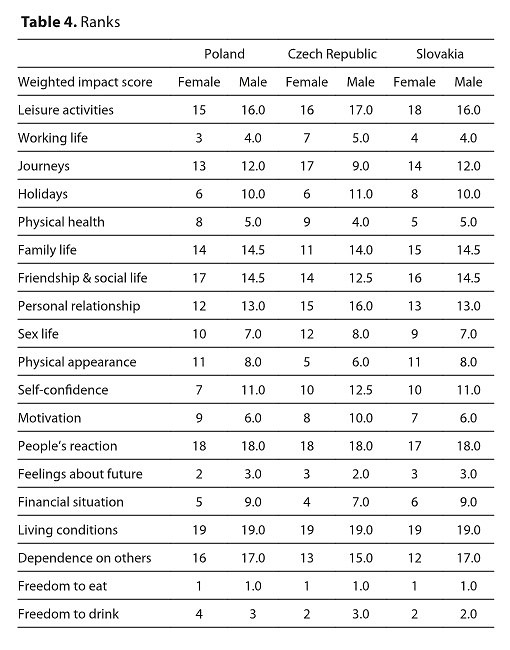
The overall average QoL was slightly higher in men than in women. In ADDQoL scores, mean weighted impact scores were negative for all domains. The domain which was the most affected by type 2 diabetes in both men and women from all three countries was the ‘freedom to eat’, while the ‘living conditions’ domain was the least affected. Diabetes had a slightly negative average weighted impact on most men and women – AWI<-3.0. Except for the different AWI scores in men with type 2 diabetes depending on their education, neither men nor women revealed any significant changes in terms of the impact of education, residence, marital status, smoking, hypertension, or taking anti-hypertensive drugs.
Conclusions:
Type 2 diabetes mellitus negatively affects all the domains of life, in both men and women in all three countries; however, this impact is insignificant. The participants assessed their quality of life as good and very good.
The aim of this study was to compare the impact of type 2 diabetes on quality of life (QoL), taking into account gender differences in relation to individual domains of Diabetes-Related Quality of Life Audit (ADDQoL) in adult men and women in Poland, the Czech Republic and Republic of Slovakia.
Material and methods:
The participants were 608 patients from the three countries, of whom 278 were women and 330 men with type 2 diabetes mellitus. The tool used was the Audit of Diabetes-Dependent Quality of Life (ADDQoL).
Results:
The overall average QoL was slightly higher in men than in women. In ADDQoL scores, mean weighted impact scores were negative for all domains. The domain which was the most affected by type 2 diabetes in both men and women from all three countries was the ‘freedom to eat’, while the ‘living conditions’ domain was the least affected. Diabetes had a slightly negative average weighted impact on most men and women – AWI<-3.0. Except for the different AWI scores in men with type 2 diabetes depending on their education, neither men nor women revealed any significant changes in terms of the impact of education, residence, marital status, smoking, hypertension, or taking anti-hypertensive drugs.
Conclusions:
Type 2 diabetes mellitus negatively affects all the domains of life, in both men and women in all three countries; however, this impact is insignificant. The participants assessed their quality of life as good and very good.
REFERENCES (43)
1.
Araszkiewicz A, Bandurska-Stankiewicz E, Budzyński A, Cypryk K, Czech A, Czupryniak L, et al. 2021 Guidelines on the management of patients with diabetes. A position of Diabetes Poland. Clin Diabetol. 2021;10(1):1–113.
3.
Rokicka D, Wróbel M, Szymorska-Kajanek A, Bożek A, Strojek K. Assessment of compliance to self monitoring of blood glucose in type 2 diabetic patients and level of implementation of Polish Diabetes Association Recommendation for general practitioners — results of multicenter, prospective educational health programme — DIABCON study. Clin Diabetol. 2018;7(3):129–135. doi:10.5603/DK.2018.0008.
4.
American Diabetes Association. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Medical Care in Diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S34-S45. doi:10.2337/dc19-S004.
5.
Krzemińska S, Bąk E, Šáteková L, Polanská A, Hašová K, Laurinc M. Comparison of Diabetes-Dependent Quality of Life (ADDQoL) in Patients with T2DM in Poland, The Czech Republic, and Slovakia. Diabetes Metab Syndr Obes. 2020; 13:3773–3786. https://doi.org/10.2147/DMSO.S....
6.
Lee KH, Xu H, Wu B. Gender differences in quality of life among community-dwelling older adults in low- and middle-income countries: results from the Study on global AGEing and adult health (SAGE). BMC Public Health 20, 114 (2020). https://doi.org/10.1186/s12889....
7.
Oreel TH, Nieuwkerk PT, Hartog ID, Netjes JE, Vonk ABA, Lemkes J, van Laarhoven HWM, Scherer-Rath M, Sprangers MAG, Henriques JPS. Gender differences in quality of life in coronary artery disease patients with comorbidities undergoing coronary revascularization. PLoS One. 2020;15(6):e0234543. doi: 10.1371/journal.pone.0234543. PMID: 32555617; PMCID: PMC7299316.
8.
Tesfay A, Gebremariam A, Gerbaba M, Abrha H. Gender differences in health related quality of life among people living with HIV on highly active antiretroviral therapy in Mekelle Town, Northern Ethiopia. Biomed Res Int. 2015;2015:516369. doi:10.1155/2015/516369.
9.
da Rocha NS, Schuch FB, Fleck MP. Gender differences in perception of quality of life in adults with and without chronic health conditions: the role of depressive symptoms. J Health Psychol. 2014;19(6):721–729. doi:10.1177/1359105313478644.
10.
Castellano-Guerrero AM, Guerrero R, Ruiz-Aranda D, et al. Gender differences in quality of life in adults with long-standing type 1 diabetes mellitus. Diabetol Metab Syndr. 2020;12:64. Published 2020 Jul 17. doi:10.1186/s13098-020-00571-x.
11.
Statistical report: diabetes statistics in Poland and in the world. [in Polish]. Available from: http://cukrzycapolska.pl/cukrz.... Accessed 03.02.2021.
14.
Bradley C, Speight J. Patient perceptions of diabetes and diabetes therapy: assessing quality of life. Diabetes Metab Res Rev. 2002;18 Suppl 3:S64-S69. doi:10.1002/dmrr.279.
15.
Bradley C, Todd C, Gorton T, Symonds E, Martin A, Plowright R. The development of an individualized questionnaire measure of perceived impact of diabetes on quality of life: the ADDQoL. Qual Life Res. 1999;8(1–2):79–91. doi:10.1023/a:1026485130100.
16.
Bak E, Marcisz C, Nowak-Kapusta Z, Dobrzyn-Matusiak D, Marcisz E, Krzeminska S. Psychometric properties of the Audit of Diabetes-Dependent Quality of Life (ADDQoL) in a population-based sample of Polish adults with type 1 and 2 diabetes. Health Qual Life Outcomes. 2018;16(1):53. Published 2018 Mar 27. doi:10.1186/s12955-018-0878-y.
17.
Brož J, Janickova Zdarska D, Urbanova J, et al. An international, multicenter, observational survey to evaluate diabetes control in subjects using insulin for the treatment of type 1 and type 2 diabetes mellitus in the Czech Republic and Slovak Republic: study protocol for a cross-sectional survey. Open Access J Clin Trials. 2016;8:13–20. doi:10.2147/OAJCT.S103459.
18.
R Core Team (2019). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.
19.
Daher AM, AlMashoor SHA, Winn T. Performance of the Malay Audit of Diabetes Dependent Quality of Life-18 and Associates of Quality of Life among Patients with Type 2 Diabetes Mellitus from Major Ethnic Groups of Malaysia. PLOS ONE. 2016;11(10):e0163701. https://doi.org/10.1371/journa....
20.
Levterova B, Orbetzova M, Levterov G, Dimitrova D, Todorov P. Assessment of the impact of type 2 diabetes on the quality of life by Audit of Diabetes-Dependent Quality-of-Life (ADDQoL-19). Biotechnol Biotechnol Equipment. 2018;32:6, 1627–1634, doi: 10.1080/13102818.2018.1532319.
21.
Bradley C, Eschwege E, de Pablos-Velasco P, et al. Predictors of Quality of Life and Other Patient-Reported Outcomes in the PANORAMA Multinational Study of People With Type 2 Diabetes. Diabetes Care. 2018;41(2):267–276. doi:10.2337/dc16-2655.
22.
Badura Brzoza K, Główczyński P, Piegza M, Błachut M, Sedlaczek K, Nabrdalik K, Gumprecht J, Gorczyca P. Acceptance of the disease and quality of life in patients with type 1 and type 2 diabetes. Eur J Psychiatry. 2022;36:114–119. doi: 10.1016/j.ejpsy.2021.12.001.
23.
Nemcova J, Hlinkova E, Farsky I, Ziakova K, Jarosova D, Zelenikova R, Buzgova R, Janikova E, Zdzieblo K, Wiraszka G, Stepien R, Nowak-Starz G, Csernus M, Balogh Z. Quality of life in patients with diabetic foot ulcer in Visegrad coun-tries. J Clin Nursing 2017;26(9–10):1245–1256.
24.
Abedini MR, Bijari B, Miri Z, et al. The quality of life of the patients with diabetes type 2 using EQ-5D-5 L in Birjand. Health Qual Life Outcomes. 2020;18:18. https://doi.org/10.1186/s12955....
25.
Arifin B, Idrus LR, van Asselt AD, Purba FD, Perwitasari DA, Thobari JA, Cao Q, Krabbe PF, Postma MJ. Health-related quality of life in Indonesian T2DM outpatients measured with the Bahasa version of EQ-5D. Qual. Life Res. 2019;28:1179–1190. doi:10.1007/s11136-019-02105-z.
26.
Bujang MA, Adnan TH, Mohd Hatta NKB, Ismail M, Lim CJ. A Revised Version of Diabetes Quality of Life Instrument Maintaining Domains for Satisfaction, Impact, and Worry. J Diabetes Res. 2018;2018:5804687. doi: 10.1155/2018/5804687.
27.
Alaofe H, Hounkpatin WA, Djrolo F, Ehiri J, Rosales C. Knowledge, attitude, practice and associated factors among patients with type 2 diabetes in Cotonou, Southern Benin. BMC Public Health. 2021;21:339. doi: 10.1186/s12889-021-10289-8.
28.
Tramunt B, Smati S, Grandgeorge N, Lenfant F, Arnal JF, Montagner A, Gourdy P. Sex differences in metabolic regulation and diabetessusceptibility. Diabetologia. 2020;63:453–461. doi: 10.1007/s00125-019-05040-3.
29.
Lewko J, Krajewska-Kułak E. Multidimensional assessment of quality of life of patients with diabetes. Pol Merk Lek. 2010;28:486–489.
30.
Glasgow RE, Ruggiero L, Eakin EG, Dryfoos J, Chobanian L. Quality of life and associated characteristics in a large national sample of adults with diabetes. Diabetes Care. 1997;20(4):562–7. doi: 10.2337/diacare.20.4.562. PMID: 9096981.
31.
Bąk E, Nowak-Kapusta Z, Dobrzyn-Matusiak D, Marcisz-Dyla E, Marcisz C, Krzemińska SA. An assessment of diabetes-dependent quality of life (ADDQoL) in women and men in Poland with type 1 and type 2 diabetes. Ann Agric Environ Med. 2019;26(3):429–438. doi:10.26444/aaem/99959.
32.
D’Souza MS, Venkatesaperumal R, Ruppert SD, Karkada SN, Jacob D. Health Related Quality of Life among Omani Men and Women with Type 2 Diabetes. J Diabetes Res. 2016;2016:8293579. doi:10.1155/2016/8293579.
33.
Chew BH, Mohd-Sidik S, Shariff-Ghazali S. Negative effects of diabetes-related distress on health-related quality of life: an evaluation among the adult patients with type 2 diabetes mellitus in three primary healthcare clinics in Malaysia. Health Qual Life Outcomes. 2015;13:187. doi: 10.1186/s12955-015-0384-4.
34.
Szcześniak G, Żmurowska B. Comparing the impact of type 2 diabetes mellitus on the quality of life in men and women. Fam Med Prim Care Rev. 2009;11:517–520.
35.
Glińska J, Skupińska A, Lewandowska M, Brosowska B, Kunikowska B. Demographic factors and the quality of life of patients with diabetes mellitus. Nursing Topics. 2012;20(3):279–288.
36.
Chudiak A, Lomper K, Jankowska-Polańska B, Uchmanowicz I. The impact of diabetes education on the assessment of the quality of life of patients type 2 diabetes. Probl Pielęgniarstwa. 2015;23:1–6. 10.5603/PP.2015.0001.
37.
Ptasiński A, Pączek L. Influence of diabetes on quality of life- assessment with the use of ADDQL questionnaire in general practice. Med Metab. 2008;4:45–48.
38.
Pichon-Riviere A, Irazola V, Beratarrechea A, Alcaraz A, Carrara C. Quality of life in type 2 diabetes mellitus patients requiring insulin treatment in Buenos Aires, Argentina: a cross-sectional study. Int J Health Policy Manag. 2015;4:475–480. doi:10.15171/ijhpm.2015.80.
39.
Zamponi V, Mazzilli R, Bitterman O, Olana S, Iorio C, Festa C, Giuliani C, Mazzilli F, Napoli A. Association between type 1 diabetes and female sexual dysfunction. BMC Womens Health. 2020;20:73. doi: 10.1186/s12905-020-00939-1.
40.
Celik S, Golbasi Z, Kelleci M, et al. Sexual Dysfunction and Sexual Quality of Life in Women with Diabetes: The Study Based on a Diabetic Center. Sex Disabil. 2015;33:233–241. doi.org/10.1007/s11195-014-9383-3.
41.
Bąk E, Marcisz C, Krzemińska S, Dobrzyn-Matusiak D, Foltyn A, Drosdzol-Cop A. Relationships of Sexual Dysfunction with Depression and Acceptance of Illness in Women and Men with Type 2 Diabetes Mellitus. Int J Environ Res Public Health. 2017;14(9):1073. doi:10.3390/ijerph14091073.
42.
Bąk E, Młynarska A, Sternal D, Kadłubowska M, Marcisz-Dyla E, Marcisz C. Sexual Function and Sexual Quality of Life in Premenopausal Women with Controlled Type 1 and 2 Diabetes-Preliminary Study. Int J Environ Res Public Health. 2021;18(5):2536. doi:10.3390/ijerph18052536.
43.
Flotynska J, Uruska A, Michalska A, Araszkiewicz A, Zozulinska-Ziolkiewicz D. Sexual Dysfunction Is a More Common Problem in Young Women with Type 1 Diabetes than in Healthy Women. J Sex Marital Ther. 2019;45:643–651. doi:10.1080/0092623X.2019.1610121.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.