Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Determinants of life situation, stress, coping resilience, and life satisfaction among parents of children with arrhythmia – a cross-sectional study
1
Department of Propaedeutics of Nursing, Faculty of Health Sciences, Medical University of Silesia, Katowice, Poland
2
Jagiellonian University Collegium Medicum UJ, Department of Pediatric Cardiology, University Children’s Hospital in Kraków, Poland
3
Krakowska Clinic, Kraków, Poland
4
Paediatric Cardiology Department, Faculty of Medical Sciences, Medical University of Silesia, Katowice, Poland
Corresponding author
Ewelina Kolarczyk
Department of Propaedeutics of Nursing, Faculty of Health Sciences in Katowice,, Francuska 20/24, 40-027, Katowice, Poland
Department of Propaedeutics of Nursing, Faculty of Health Sciences in Katowice,, Francuska 20/24, 40-027, Katowice, Poland
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
In some cases, there is a need to hospitalize a child for diagnosis and treatment of cardiac arrhythmias, resulting in expected changes in family functioning, often making it impossible to carry out the current family and professional plans of the child’s parents/caregivers. The aim of the study was to examine the life situation of parents of children with cardiac arrhythmias in relation to the incidence of stress, the role of spirituality, life satisfaction, coping resilience, and to selected socio-demographic factors.
Material and methods:
The study included 101 parents of children with heart arhythm and conduction disorders who were diagnosed and treated at a Clinical Centre. The survey used the Life Situation Assessment Questionnaire for Parents, Satisfaction with Life Scale (SWLS), the Perceived Stress Scale (PSS) and the Brief Resilient Coping Scale.
Results:
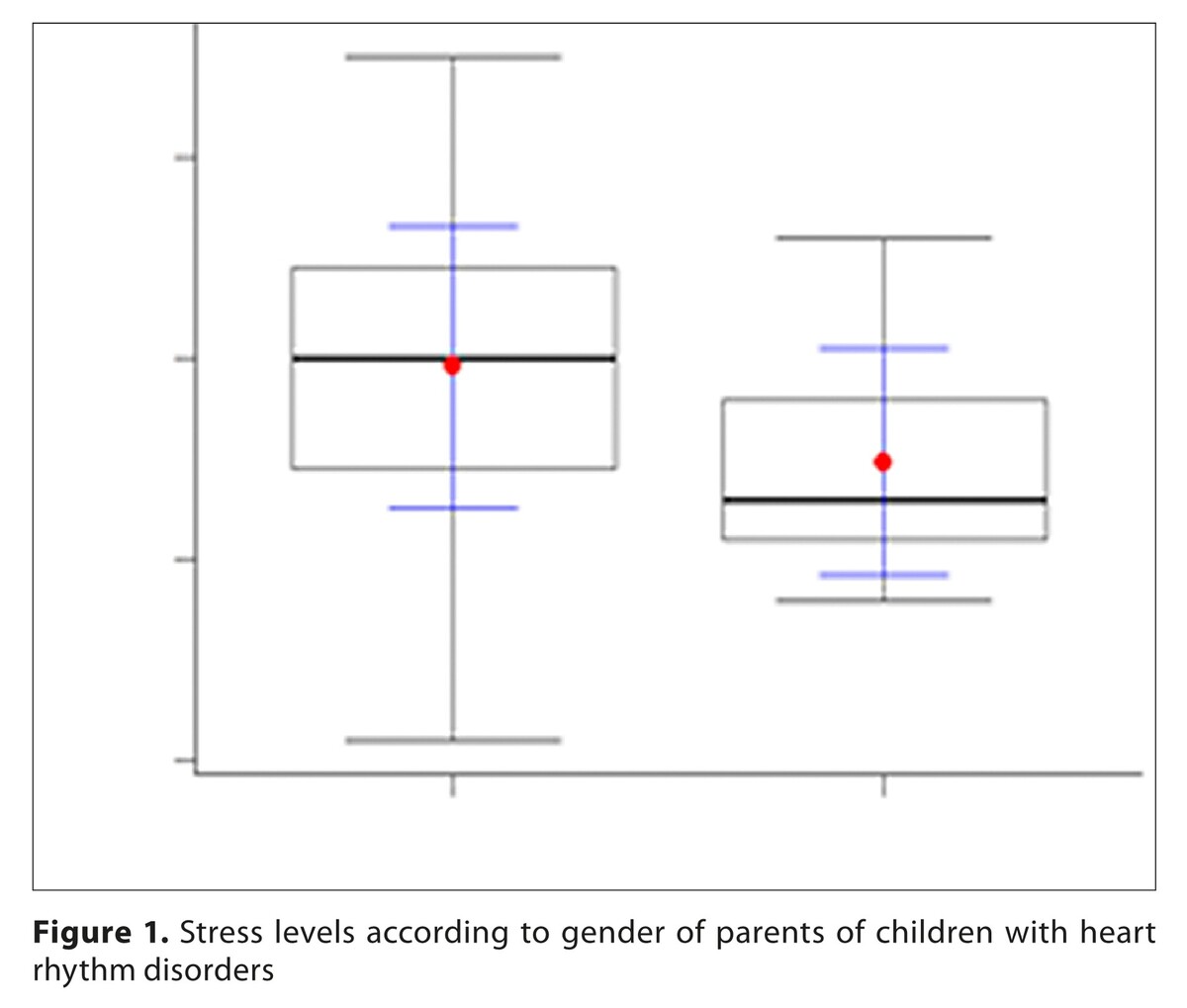
Analysis showed that the personal functioning of the parents was good (p=0.002), while the impact of spirituality on life functioning was medium (p=0.010). The level of general life situation, level of life satisfaction and level of perceived stress, were significantly high (p=0.001;p=0.001; p=0.004). More stress was felt by mothers than fathers (p=0.023) and parents with higher education (p=0.047), as well as those who practice religion (p=0.008). Parents who were in a relationship felt better life satisfaction (p=0.004), and the living situation of rural residents was statistically significantly better than urban residents (p=0.024).
Conclusions:
Understanding the life situation and emotions of parents of children with cardiac arrhythmia will help health care providers offer sufficient support.
In some cases, there is a need to hospitalize a child for diagnosis and treatment of cardiac arrhythmias, resulting in expected changes in family functioning, often making it impossible to carry out the current family and professional plans of the child’s parents/caregivers. The aim of the study was to examine the life situation of parents of children with cardiac arrhythmias in relation to the incidence of stress, the role of spirituality, life satisfaction, coping resilience, and to selected socio-demographic factors.
Material and methods:
The study included 101 parents of children with heart arhythm and conduction disorders who were diagnosed and treated at a Clinical Centre. The survey used the Life Situation Assessment Questionnaire for Parents, Satisfaction with Life Scale (SWLS), the Perceived Stress Scale (PSS) and the Brief Resilient Coping Scale.
Results:
Analysis showed that the personal functioning of the parents was good (p=0.002), while the impact of spirituality on life functioning was medium (p=0.010). The level of general life situation, level of life satisfaction and level of perceived stress, were significantly high (p=0.001;p=0.001; p=0.004). More stress was felt by mothers than fathers (p=0.023) and parents with higher education (p=0.047), as well as those who practice religion (p=0.008). Parents who were in a relationship felt better life satisfaction (p=0.004), and the living situation of rural residents was statistically significantly better than urban residents (p=0.024).
Conclusions:
Understanding the life situation and emotions of parents of children with cardiac arrhythmia will help health care providers offer sufficient support.
ACKNOWLEDGEMENTS
The authors would like to express their gratitude to Mr. Piotr
Dec from a statistics company for their statistical support.
The authors also wish to thank Ms. Barbara Wójcik and Ms.
Monika Staszkiewicz from the Secretariat of the Pediatric
Cardiology Department for the assistance throughout this
research project, as well as all the parents of hospitalized
children with congenital heart disease who participated in
this study.
FUNDING
This research was funded by the Medical University of Silesia
in Katowice, Poland, under the “Young Scientist” research
grant, no: BNW-2-043/N/4/Z.
REFERENCES (42)
1.
Shen L, Liu S, Hu F, et al. Electrophysiological characteristics and ablation outcomes in patients with catecholaminergic polymorphic ventricular tachycardia. J Am Heart Assoc. 2023;12(24):e031768. http://doi:10.1161/JAHA.123.03....
2.
Oeffl N, Krainer M, Kurath-Koller S, et al. Cardiac arrhythmias requiring electric countershock during the neonatal period-a systematic review. Children (Basel). 2023;10(5):838. http:// doi:10.3390/children10050838.
3.
Taylor RA, Thomas R, Lawrence D. Nonutility of diagnostic testing in ambulatory patients with supraventricular tachycardia. Pediatr Emerg Care. 2022;38(3):e1036-e1040. http://doi:10.1097/PEC.0000000....
4.
Drago F, Battipaglia I, Di Mambro C. Neonatal and paediatric arrhythmias: clinical and electrocardiographic aspects. Card Electrophysiol Clin. 2018;10(2):397–412. http://doi:10.1016/j.ccep.2018....
5.
Brancato F, De Rosa G, Gambacorta A, et al. Role of troponin determination to diagnose chest pain in the paediatric emergency department. Pediatr Emerg Care. 2021;37(12):e1589-e1592. http://doi:10.1097/PEC.0000000....
6.
Velázquez-Rodríguez E, García-Hernández N, Silva-Oropeza E, et al. Idiopathic left fascicular ventricular tachycardia in children and adolescents. Taquicardia ventricular fascicular izquierda idiopática en niños y adolescentes. Bol Med Hosp Infant Mex. 2022;79(4):248–258. http://doi:10.24875/BMHIM.2100....
7.
Wojcik MH, Krous HF, Goldstein RD. Sudden unexplained death in childhood: current understanding. Pediatr Emerg Care. 2023;39(12):979–983. http:// doi:10.1097/01.pec.0000997588.40847.b0.
8.
Tsuda T, Fitzgerald KK, Temple J. Sudden cardiac death in children and young adults without structural heart disease: a comprehensive review. Rev Cardiovasc Med. 2020;21(2):205–216. http://doi:10.31083/j.rcm.2020....
9.
Cohen MI. Frequent premature ventricular beats in healthy children: when to ignore and when to treat?. Curr Opin Cardiol. 2019;34(1):65–72. http://doi:10.1097/HCO.0000000....
10.
Turska-Kmieć A. Natural history of idiopathic ventricular arrhythmias in children. WDR 2017;3(44):4–8. https://doi.org/10.5604/01.300....
11.
Van Niekerk C, Van Deventer BS, du Toit-Prinsloo L. Long QT syndrome and sudden unexpected infant death. J Clin Pathol. 2017;70(9): 808–813. http://doi:10.1136/jclinpath-2....
12.
Wall JJ, Iyer RV. Catecholaminergic polymorphic ventricular tachycardia. Pediatr Emerg Care. 2017;33(6):427–431. http://doi:10.1097/PEC.0000000....
13.
Mariani MV, Pierucci N, Fanisio F, et al. Inherited arrhythmias in the paediatric population: an updated overview. Medicina (Kaunas). 2024;60(1):94. http://doi:10.3390/medicina600....
14.
Whitaker J, Wright MJ, Tedrow U. Diagnosis and management of ventricular tachycardia. Clin Med (Lond). 2023;23(5):442–448. http://doi:10.7861/clinmed.202....
15.
Escudero CA, Tan RBM, Beach CM, Dalal AS, et al. Approach to wide complex tachycardia in paediatric patients. CJC Pediatr Congenit Heart Dis. 2022;1(2):60–73. http://doi:10.1016/j.cjcpc.202....
16.
Manickavasagam A, Roshan J. Catheter ablation of paediatric ventricular arrhythmias: a work in progress. Indian Pacing Electrophysiol J. 2023;23(4):108–109. http://doi:10.1016/j.ipej.2023....
17.
Ljubas Perčić D, Krmek N, Benko I, et al. Frequent accelerated idioventricular rhythm in an otherwise healthy child: a case report and review of literature. BMC Cardiovasc Disord. 2023;23(1):37. http://doi:10.1186/s12872-023-....
18.
Zhang Y, Zhou H, Bai Y, et al. Families under pressure: A qualitative study of stressors in families of children with congenital heart disease. Stress Health. 2023;39(5):989–999. http://doi:10.1002/smi.3240.
19.
Olowookere SA, Badmus SA, Laoye O, Ijadunola MY, Hassan M. Burden of family caregivers of ophthalmic patients in a university teaching hospital in south-west Nigeria. Malawi Med J. 2019;31(1):39–44. http://doi:10.4314/mmj.v31i1.7.
20.
Toledano-Toledano F, Luna D. The psychosocial profile of family caregivers of children with chronic diseases: a cross-sectional study. Biopsychosoc Med. 2020;14:29. http://doi:10.1186/s13030-020-....
21.
Cetinbakis G, Bastug G, Ozel-Kizil ET. Factors contributing to higher caregiving burden in Turkish mothers of children with autism spectrum disorders. Int J Dev Disabil. 2018;66(1):46–53. http://doi:10.1080/20473869.20....
22.
Bektas İ, Kır M, Yıldız K, et al. Symptom Frequency in children with congenital heart disease and parental care burden in predicting the quality of life of parents in Turkey. J Pediatr Nurs. 2020;53:e211-e216. http://doi:10.1016/j.pedn.2020....
23.
Semerci R, Uysal G, Açikgöz A, Demirer P. The predictive power of religious coping on care burden, depression, stress, and anxiety of parents of paediatric oncology patients in Turkey. J Relig Health. 2024;63(5):3618–3635. http://doi:10.1007/s10943-024-....
24.
Allam LE, Nabih MA, El-Missiry MA. The psychological impact of permanent cardiac pacemakers on paediatric patients and their parents: A case control study. Indian Heart J. 2018;70(6):872–878. http://doi:10.1016/j.ihj.2018.....
25.
Dalir Z, Heydari A, Kareshki H, Manzari ZS. Coping with caregiving stress in families of children with congenital heart disease: a qualitative study. Int J Community Based Nurs Midwifery. 2020;8(2):127–139. http://doi:10.30476/IJCBNM.202....
26.
Yakubu YA, Schutte DW. Caregiver attributes and socio-demographic determinants of caregiving burden in selected low-income communities in cape town, South Africa. J Compassionate Health Care. 2018;5:3. https://doi.org/10.1186/s40639....
27.
Gonzalez M, Zeidan J, Lai J, et al. Socio-demographic disparities in receipt of clinical health care services during the COVID-19 pandemic for canadian children with disability. BMC Health Serv Res. 2022;22(1):1434. http://doi:10.1186/s12913-022-....
28.
Pankewicz A, Davis RK, Kim J, et al. Children with special needs: social determinants of health and care coordination. Clin Pediatr (Phila). 2020;59(13):1161–1168. http://doi:10.1177/00099228209....
29.
Han J, Zhang L, Yang F, Wang L. Illness cognition and associated socio-demographic and clinical factors in parents of children with leukemia. BMC Psychol. 2024;12(1):289. http://doi:10.1186/s40359-024-....
30.
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Online https://www.equator-network.or... (access: 2024.06.29).
31.
Kolarczyk E, Morka A, Barański K, Szydłowski L. Life situation of a caregiver of a child with congenital heart defect and/or other cardiac problems: structure and preliminary validation of a new questionnaire. Front Psychol. 2023;14:1194031. http://doi:10.3389/fpsyg.2023.....
32.
Juczynski Z. Satisfaction with Life Scale. In: Measurement tools in health promotion and psychology. Warsaw: Psychological Testing Laboratory of the Polish Psychological Association; 2001. p. 134–138.
33.
Juczynski Z, Ogińska-Bulik N. Tools for measuring stress and coping with stress. Psychological Testing Laboratory of the Polish Psychological Association, 2009.
34.
Piórowska A, Piórowski K, Basińska M, Janicka M. Polish adaptation of The Brief Resilience Coping Scale. Pedagogical Rev. 2017;1:215–227. Online http://cejsh.icm.edu.pl/cejsh/... (access:20.01.2025).
35.
WMA Declaration of Helsinki – Ethical Principles for Medical Research Involving Human Participants. Online https://www.wma.net/policies-p... (access:2024.03.01).
36.
Q&A: Good clinical practice (GCP). Online https://www.ema.europa.eu/en/h... (access:2024.03.01).
37.
Law E, Fisher E, Eccleston C, Palermo TM. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev. 2019;3(3):CD009660. http://doi:10.1002/14651858.CD....
38.
Feudtner C, Nye RT, Boyden JY, et al. Association between children with life-threatening conditions and their parents’ and siblings’ mental and physical health. JAMA Netw Open. 2021;4(12):e2137250. http:// doi:10.1001/jamanetworkopen.2021.37250.
39.
Lin C, Xiaoyi S, Xiaoman C, et al. Development of a knowledge, attitude, and practice scale for cardiac rehabilitation for parents of children with heart disease. J Pediatr Nurs. 2023;72:161–167. http://doi:10.1016/j.pedn.2022....
40.
Superdock AK, Barfield RC, Brandon DH, Docherty SL. Exploring the vagueness of religion & spirituality in complex paediatric decision-making: a qualitative study. BMC Palliat Care. 2018;17(1):107. http://doi:10.1186/s12904-018-....
41.
Liu JF, Xie WP, Lin WH, Cao H, Chen Q. The association of positive or negative religious coping methods with psychological distress and quality of life among parents of infants with congenital heart disease. Front Pediatr. 2021;9:753032. http://doi:10.3389/fped.2021.7....
42.
Lisanti AJ, Allen LR, Kelly L, Medoff-Cooper B. Maternal stress and anxiety in the paediatric cardiac intensive care unit. Am J Crit Care. 2017;26(2):118–125. http://doi:10.4037/ajcc2017266.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.