Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Congenital cytomegalovirus infections in Poland – a national hospital register-based study
1
Department of Social Medicine and Public Health, Medical University, Warsaw, Poland
2
National Institute of Public Health/National Institute of Hygiene, Warsaw, Poland
3
Department of Medical Informatics and Statistics with E-learning Laboratory, Medical University, Lublin, Poland
Corresponding author
Krzysztof Kanecki
Department of Social Medicine and Public Health, Medical University of Warsaw, Oczki 3, 02-007, Warsaw, Poland
Department of Social Medicine and Public Health, Medical University of Warsaw, Oczki 3, 02-007, Warsaw, Poland
Ann Agric Environ Med. 2020;27(4):574-578
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Congenital cytomegalovirus (cCMV) infections are common worldwide. CCMV infected newborns are mostly asymptomatic at birth. However, cCMV remains the major infectious cause of congenital abnormalities in the developing foetus and newborns. The aim of the study was to provide recent data on cCMV in Poland.
Material and methods:
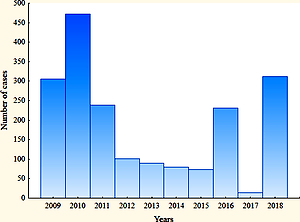
Aretrospective, population-based study was conducted using data from hospital discharge records of patients hospitalized from 2009–2018. CCMV incidence rates were estimated on the basis of data taken from a Polish hospital morbidity study, carried out by the National Institute of Public Health.
Results:
The study group consisted of 1,916 hospitalized patients with the first-time diagnosis of cCMV. Among them, 52% were patients up to 30 days of age. The median age was 28 days. The average annual incidence of cCMV was 48 per 100,000 live births (95% CI 23.5–73.4). A significantly higher cCMV incidence rate was observed in patients from more urban than rural regions of Poland (55 per 100,000 vs 39 per 100,000; P<0.001). In the study period, 9 hospital deaths (0.5 % of all patients) were reported. The coexistence of nervous system diseases was observed in 26% of cases and hearing loss in 6% of cases
Conclusions:
The significantly more cCMV cases were observed in patients from more urban than rural regions of Poland may suggest the presence of territorial factors related to the cCMV incidence in Poland. The relatively high percentage of newborns with hearing loss or neurologic diseases may require activities aimed at reducing the cCMV incidence. The epidemiological data presented may be useful for comparisons with other geographical regions.
Congenital cytomegalovirus (cCMV) infections are common worldwide. CCMV infected newborns are mostly asymptomatic at birth. However, cCMV remains the major infectious cause of congenital abnormalities in the developing foetus and newborns. The aim of the study was to provide recent data on cCMV in Poland.
Material and methods:
Aretrospective, population-based study was conducted using data from hospital discharge records of patients hospitalized from 2009–2018. CCMV incidence rates were estimated on the basis of data taken from a Polish hospital morbidity study, carried out by the National Institute of Public Health.
Results:
The study group consisted of 1,916 hospitalized patients with the first-time diagnosis of cCMV. Among them, 52% were patients up to 30 days of age. The median age was 28 days. The average annual incidence of cCMV was 48 per 100,000 live births (95% CI 23.5–73.4). A significantly higher cCMV incidence rate was observed in patients from more urban than rural regions of Poland (55 per 100,000 vs 39 per 100,000; P<0.001). In the study period, 9 hospital deaths (0.5 % of all patients) were reported. The coexistence of nervous system diseases was observed in 26% of cases and hearing loss in 6% of cases
Conclusions:
The significantly more cCMV cases were observed in patients from more urban than rural regions of Poland may suggest the presence of territorial factors related to the cCMV incidence in Poland. The relatively high percentage of newborns with hearing loss or neurologic diseases may require activities aimed at reducing the cCMV incidence. The epidemiological data presented may be useful for comparisons with other geographical regions.
Kanecki K, Nitsch-Osuch A, Goryński P, Bogdan M, Barańska A, Tyszko P. Congenital cytomegalovirus infections in Poland – a national hospital
register-based study. Ann Agric Environ Med. 2020; 27(4): 574–578. doi: 10.26444/aaem/128635
REFERENCES (43)
1.
Rawlinson WD, Boppana SB, Fowler KB, et al. Congenital cyto-megalo virus infection in pregnancy and the neonate: consensus recommendations for prevention, diagnosis, and therapy. Lancet Infect Dis. 2017; 17(6): e177–188. https://doi.org/10.1016/S1473-....
2.
Manicklal S, Emery VC, Lazzarotto T, et al. The “silent” global burden of congenital cytomegalovirus. Clin Microbiol Rev. 2013; 26(1): 86–102. https://doi.org/10.1128/CMR.00....
3.
Bristow BN, O’Keefe KA, Shafir SC, et al. Congenital cytomegalovirus mortality in the United States, 1990–2006. PLoS Negl Trop Dis. 2011; 5(4): e1140. https://doi.org/10.1371/journa....
4.
Pereira L. Congenital Viral Infection: Traversing the Uterine-Placental Interface. Annu Rev Virol. 2018 29; 5(1): 273–99. https://doi.org/10.1146/annure....
5.
Picone O, Vauloup-Fellous C, Cordier AG, et al. A series of 238 cytomegalovirus primary infections during pregnancy: description and outcome. Prenat Diagn. 2013; 33(8): 751–758. https://doi.org/10.1002/pd.411....
6.
Kobas M, Bickle Graz M, Truttmann AC, et al. Clinical characteristics, audiological and neurodevelopmental outcomes of newborns with congenital cytomegalovirus infection. Swiss Med Wkly. 2018; 148: w14 62 ht t ps://doi.org /10.4 414/smw.2018.14 627
7.
Leruez-Ville M, Guilleminot T, Stirnemann J, et al. Quantifying the burden of congenital CMV infection (cCMV) with long-term sequelae in subsequent pregnancies of women seronegative at their first pregnancy. Clin Infect Dis, ciz1067. https://doi.org/10.1093/cid/ci....
8.
Leruez-Ville M, Magny J-F, Couderc S, et al. Risk Factors for Congenital Cytomegalovirus Infection Following Primary and Nonprimary Maternal Infection: A Prospective Neonatal Screening Study Using Polymerase Chain Reaction in Saliva. Clin Infect Dis. 2017; 65(3): 398– 404. ht tps://doi.org /10.1093/cid/ci x 337.
9.
Mestas E. Congenital Cytomegalovirus. Adv Neonatal Care. 2016; 16(1): 60–65. https://doi.org/10.1097/ANC.00...
10.
Goderis J, De Leenheer E, Smets K, et al. Hearing loss and congenital CMV infection: a systematic review. Pediatrics. 2014; 134(5): 972–982. https://doi.org/10.1542/peds.2....
11.
Lopez AS, Ortega-Sanchez IR, Bialek SR. Congenital cytomegalovirus-related hospitalizations in infants <1 year of age, United States, 1997–2009. Pediatr Infect Dis J. 2014; 33(11): 1119–23. https://doi.org/10.1097/INF.00...
12.
Leung J, Kennedy JL, Haberling DL, et al. Congenital CMV-Coded Diagnosis Among American Indian and Alaska Native Infants in the United States, 2000–2017. J Immigr Minor Health. 2020; 22(5): 1101–1104. https://doi.org/10.1007/s10903....
13.
Lanzieri TM, Dollard SC, Bialek SR, et al. Systematic review of the birth prevalence of congenital cytomegalovirus infection in developing countries. Int J Infect Dis. 2014; 22: 44–48. https://doi.org/10.1016/j.ijid....
14.
Putri ND, Wiyatno A, Dhenni R, et al. Birth prevalence and characteristics of congenital cytomegalovirus infection in an urban birth cohort, Jakarta, Indonesia. Int J Infect Dis. 2019; 86: 31–39. https://doi.org/10.1016/j.ijid....
15.
Wang S, Wang T, Zhang W, et al. Cohort study on maternal cytomegalovirus seroprevalence and prevalence and clinical manifestations of congenital infection in China. Medicine (Baltimore). 2017; 96(5): e6007. https://doi.org/10.1097/MD.000...
16.
Rütten H, Rissmann A, Brett B, et al. Congenital cytomegalovirus infection in Central Germany: an underestimated risk. Arch Gynecol Obstet. 2017; 296(2): 231–240. https://doi.org/10.1007/s00404....
17.
Townsend CL, Forsgren M, Ahlfors K, et al. Long-term outcomes of congenital cytomegalovirus infection in Sweden and the United Kingdom. Clin Infect Dis. 2013; 56(9): 1232–1239. https://doi.org/10.1093/cid/ci....
18.
Siennicka J, Dunal-Szcepaniak M, Trzcińska A, et al. High Seroprevalence of CMV Among Women of Childbearing Age Implicates High Burden of Congenital Cytomegalovirus Infection in Poland. Pol J Microbiol. 2017; 65(4): 425–432. https://doi.org/10.5604/173313....
19.
Rycel M, Wujcicka W, Zawilińska B, et al. Mixed infections with distinct cytomegalovirus glycoprotein B genotypes in Polish pregnant women, fetuses, and newborns. Eur J Clin Microbiol Infect Dis. 2015; 34(3): 585–591. https://doi.org/10.1007/s10096....
20.
Paradowska E, Jabłońska A, Studzińska M, et al. Distribution of the CMV glycoprotein gH/gL/gO and gH/gL/pUL128/pUL130/pUL131A complex variants and associated clinical manifestations in infants infected congenitally or postnatally. Sci Rep. 2019 08; 9(1): 16352. https://doi.org/10.1038/s41598....
21.
Kasztelewicz B, Czech-Kowalska J, Lipka B, et al. Cytokine gene polymorphism associations with congenital cytomegalovirus infection and sensorineural hearing loss. Eur J Clin Microbiol Infect Dis. 2017; 36(10): 1811–1818. https://doi.org/10.1007/s10096....
22.
Sobolewska-Pilarczyk M, Pawlak-Osinska K, Drewa S, et al. Intra-ventricular haemorrhage as the first manifestation of congenital Cytomegalovirus infection. Indian J Med Microbiol. 2018; 36(2): 279–281. https://doi.org/10.4103/ijmm.I....
24.
TIBCO Software Inc. (2017). Statistica (data analysis software system), version 13. http://statistica.io.
25.
Abramson JH. WINPEPI updated: computer programs for epidemio-logists, and their teaching potential. Epidemiol Perspect Innov. 2011; 8: 1. https://doi.org/10.1186/1742-5....
26.
Pokorska-Śpiewak M, Niezgoda A, Gołkowska M, et al. Recommenda-tions for the diagnosis and treatment of CMV infections. Polish Society of Epidemiology and Infectious Diseases. Przegl Epidemiol. 2016; 70(2): 297–310.
27.
Bartlett AW, Hall BM, Palasanthiran P, et al. Recognition, treatment, and sequelae of congenital cytomegalovirus in Australia: An observational study. J Clin Virol. 2018; 108: 121–125. https://doi.org/10.1016/j.jcv.....
28.
Dollard SC, Grosse SD, Ross DS. New estimates of the prevalence of neurological and sensory sequelae and mortality associated with congenital cytomegalovirus infection. Rev Med Virol. 2007; 17(5): 355–363. https://doi.org/10.1002/rmv.54....
29.
Lazzarotto T, Guerra B, Lanari M, et al. New advances in the diagnosis of congenital cytomegalovirus infection. J Clin Virol. 2008; 41(3): 192–197. https://doi.org/10.1016/j.jcv.....
30.
L’Huillier AG, Crisinel PA. Toxoplasmose et cytomégalovirus con-génitaux en Suisse en 2019 [Congenital Toxoplasmosis and CMV in Switzerland in 2019]. Rev Med Suisse. 2020; 16(682): 361–364. [Abstract in English, French]. https://pubmed.ncbi.nlm.nih.go... (access: 2020.09.27).
31.
Seale H, Booy R, MacIntyre CR. Trends in hospitalizations for diagnosed congenital cytomegalovirus in infants and children in Australia. BMC Pediatr 2009; 9: 1. https://doi.org/10.1186/1471-2....
32.
Ohyama S, Fujioka K, Fukushima S, et al. Diagnostic Value of Cyto-megalovirus IgM Antibodies at Birth in PCR-Confirmed Congenital Cytomegalovirus Infection. Int J Mol Sci. 2019; 20(13): 3239. https://doi.org/10.3390/ijms20....
33.
Fowler KB. Congenital cytomegalovirus infection: audiologic outcome. Clin Infect Dis. 2013; 57 Suppl 4: S182–184. https://doi.org/10.1093/cid/ci....
34.
Faure-Bardon V, Magny J-F, Parodi M, et al. Sequelae of Congenital Cytomegalovirus Following Maternal Primary Infections Are Limited to Those Acquired in the First Trimester of Pregnancy. Clin Infect Dis. 2019; 69(9): 1526–1532. https://doi.org/10.1093/cid/ci....
35.
McMullan BJ, Palasanthiran P, Jones CA, et al. Congenital cyto-megalovirus — time to diagnosis, management and clinical sequelae in Australia: opportunities for earlier identification. Medical Journal of Australia. 2011; 194(12): 625–629. https://doi.org/10.5694/j.1326....
36.
Naing ZW, Scott GM, Shand A, et al. Congenital cytomegalovirus infection in pregnancy: a review of prevalence, clinical features, diagnosis and prevention. Aust N Z J Obstet Gynaecol. 2016; 56(1): 9–18. ht t ps://doi.org /10.1111/ajo.12408.
37.
Inagaki K, Blackshear C, Palmer A, et al. Risk Factors, Geographic Distribution, and Healthcare Burden of Symptomatic Congenital Cytomegalovirus Infection in the United States: Analysis of a Nationally Representative Database, 2000–2012. J Pediatr. 2018; 199: 118–123.e1. https://doi.org/10.1016/j.jped....
38.
Cannon MJ, Schmid DS, Hyde TB. Review of cytomegalovirus seroprevalence and demographic characteristics associated with infection. Rev Med Virol. 2010; 20(4): 202–213. https://doi.org/10.1002/r mv.655.
39.
Korndewal MJ, Mollema L, Tcherniaeva I, et al. Cytomegalovirus infection in the Netherlands: seroprevalence, risk factors, and implications. J Clin Virol. 2015; 63: 53–58. https://doi.org/10.1016/j.jc v.2014.11.033.
40.
Lamarre V, Gilbert NL, Rousseau C, et al. Seroconversion for cyto-megalovirus infection in a cohort of pregnant women in Québec, 2010–2013. Epidemiol Infect. 2016; 144(8): 1701–1709. https://doi.org/10.1017/S09502....
41.
Bate SL, Dollard SC, Cannon MJ. Cytomegalovirus seroprevalence in the United States: the national health and nutrition examination surveys, 1988–2004. Clin Infect Dis. 2010; 50(11): 1439–1447. https://doi.org/10.1086/652438.
42.
Smithers-Sheedy H, Raynes-Greenow C, Badawi N, et al. Cytomegalo-virus-related childhood mortality in Australia 1999–2011. J Paediatr Child Health. 2015; 51(9): 901–905. https://doi.org/10.1111/jpc.12....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.