Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2025
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Comparative analysis of venous thromboembolic complications in diverse groups of orthopaedic patients
1
Hospital of the Ministry of Interior and Administration, Lublin, Poland
2
Department of Clinical and Radiological Anatomy, Medical University, Lublin, Poland
3
University of Physical Education in Warsaw, branch in Biała Podlaska, Poland
4
Scientific Research Group of the Chair and Department of Epidemiology and Clinical Research Methodology, Medical University, Lublin, Poland
Corresponding author
Piotr Piech
Department of Clinical and Radiological Anatomy Medical University of Lublin, Chodźki 4 (CSM), 20-093, Lublin, Poland
Department of Clinical and Radiological Anatomy Medical University of Lublin, Chodźki 4 (CSM), 20-093, Lublin, Poland
Ann Agric Environ Med. 2024;31(1):119-124
KEYWORDS
orthopaedic surgerytraumatologyvenous thromboembolismtrauma complicationspulmonary embolismpelvis fracturespine fracturelower limb fracture
TOPICS
ABSTRACT
Introduction and objective:
Venous thromboembolism (VTE) is one of the most important and life-threatening complications in orthopaedic surgery. According to current scientific reports, there are several variables that can affect the severity of CVD, including the site of the pathology or the type of treatment implemented. The aim of the study was to analyze the risk of VTE depending on the location of the pathology, as well as to evaluate the impact of surgical treatment compared to conservative management.
Material and methods:
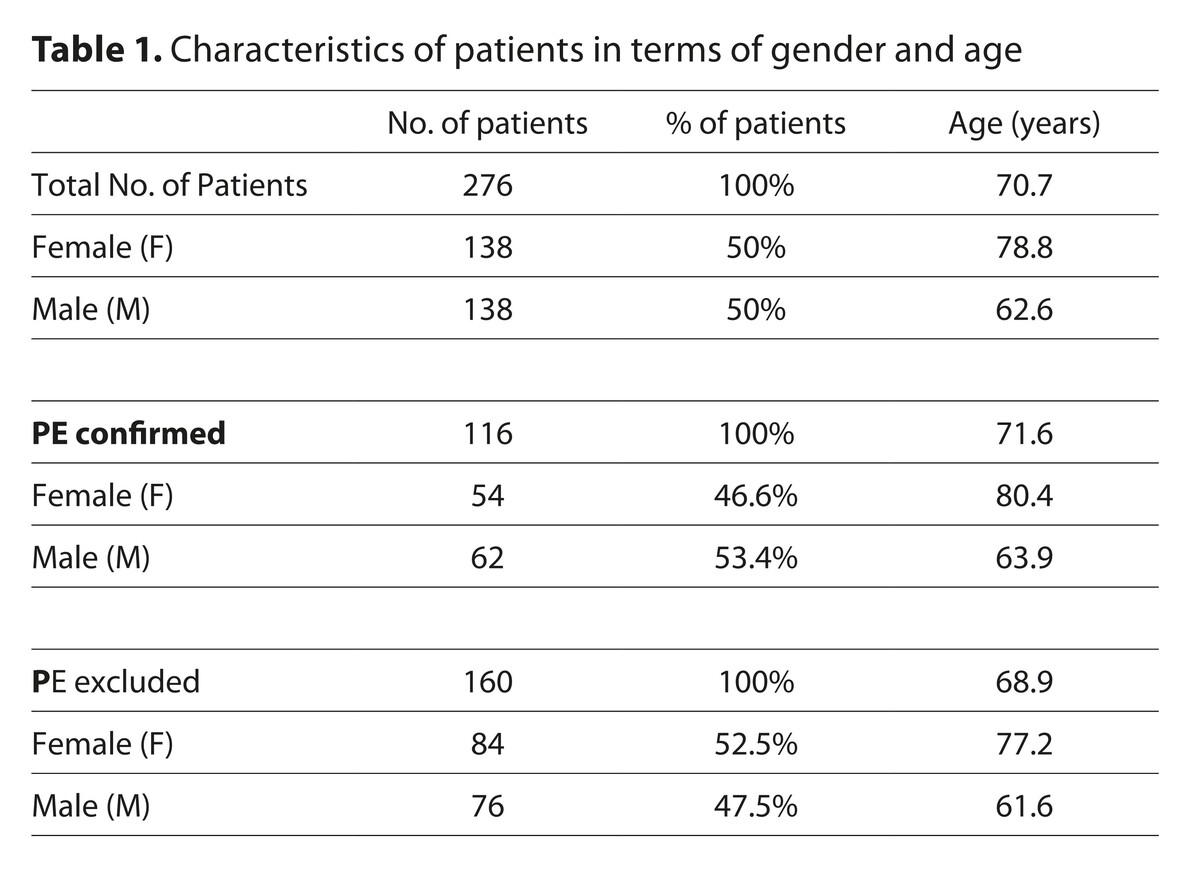
Analysis of laboratory results and clinical picture of 276 patients hospitalized for orthopaedic reasons, admitted between January 2008 – December 2019, with suspected pulmonary embolism (PE).
Results:
Among patients diagnosed with PE, the most common location of the disease was in the lower limb 59/116 (50.9%), followed by the pelvis location – 22/116 (19.0%), the spine – 19/116 (16.4%), disseminated lesions in oncological patients – 12/116 (10.3%), and a group of pathologies in the upper limb – 4/116 (3.5%). Significant statistical differences were found between the incidence of PE and the diagnosis of pathology in the lower limb and the pelvis. In the group of patients, there was no statistically significant relationship between the incidence of PE associated with surgical treatment, compared to conservative management.
Conclusions:
The group with the highest risk of VTE were lower limb and pelvic pathologies. The results are largely consistent with numerous reports treating the risk of CVD among orthopaedic patient populations.
Venous thromboembolism (VTE) is one of the most important and life-threatening complications in orthopaedic surgery. According to current scientific reports, there are several variables that can affect the severity of CVD, including the site of the pathology or the type of treatment implemented. The aim of the study was to analyze the risk of VTE depending on the location of the pathology, as well as to evaluate the impact of surgical treatment compared to conservative management.
Material and methods:
Analysis of laboratory results and clinical picture of 276 patients hospitalized for orthopaedic reasons, admitted between January 2008 – December 2019, with suspected pulmonary embolism (PE).
Results:
Among patients diagnosed with PE, the most common location of the disease was in the lower limb 59/116 (50.9%), followed by the pelvis location – 22/116 (19.0%), the spine – 19/116 (16.4%), disseminated lesions in oncological patients – 12/116 (10.3%), and a group of pathologies in the upper limb – 4/116 (3.5%). Significant statistical differences were found between the incidence of PE and the diagnosis of pathology in the lower limb and the pelvis. In the group of patients, there was no statistically significant relationship between the incidence of PE associated with surgical treatment, compared to conservative management.
Conclusions:
The group with the highest risk of VTE were lower limb and pelvic pathologies. The results are largely consistent with numerous reports treating the risk of CVD among orthopaedic patient populations.
REFERENCES (22)
1.
Kahn SR, Shivakumar S. What’s new in VTE risk and prevention in orthopaedic surgery. Res Pract Thromb Haemost. 2020;4(3):366–376. Published 2020 Mar 9. doi:10.1002/rth2.12323.
2.
Gade IL, Kold S, Severinsen MT, et al. Venous thromboembolism after lower extremity orthopaedic surgery: A population-based nationwide cohort study. Res Pract Thromb Haemost. 2020;5(1):148–158. Published 2020 Nov 30. doi:10.1002/rth2.12449.
3.
Majima T, Oshima Y. Venous Thromboembolism in Major Orthopaedic Surgery. J Nippon Med Sch. 2021;88(4):268–272. doi:10.1272/jnms.JNMS.2021_88-418.
4.
Muscatelli SR, Charters MA, Hallstrom BR. Time for an Update? A Look at Current Guidelines for Venous Thromboembolism Prophylaxis After Hip and Knee Arthroplasty and Hip Fracture. Arthroplast Today. 2021;10:105–107. Published 2021 Jul 15. doi:10.1016/j.artd.2021.06.015.
5.
Melman WP, Ettema HB, Verheyen CC. Symptomatic venous thromboembolism after trauma surgery: a study on 56.884 procedures. Acta Orthop Belg. 2020;86(3):363–368.
6.
Mula V, Parikh S, Suresh S, Bottle A, Loeffler M, Alam M. Venous thromboembolism rates after hip and knee arthroplasty and hip fractures. BMC Musculoskelet Disord. 2020;21(1):95. Published 2020 Feb 12. doi:10.1186/s12891-020-3100-4.
7.
Hu C, Liu C, Wang Y, Ding T, Sun K, Tian S. The Timing of Symptomatic Pulmonary Embolism in Patients With Nonwarfarin Anticoagulants Following Elective Primary Total Joint Arthroplasty. J Arthroplasty. 2020;35(6):1703–1707. doi:10.1016/j.arth.2020.01.024.
8.
Samama CM, Rosencher N, Laporte S, Girard P. Preventing venous thrombo-embolism after nonmajor orthopaedic surgery. Trends Cardiovasc Med. 2021;31(8):507–511. doi:10.1016/j.tcm.2020.10.013.
9.
Haque A, Patel MS, Siddiqui B, Wildin CJ, Dias JJ. Venous thromboembolic events in hand surgery. J Plast Surg Hand Surg. 2021;55(3):190–194. doi:10.1080/2000656X.2020.1856671.
10.
Galsklint J, Kold S, Kristensen SR, Severinsen MT, Gade IL. Validation of Postsurgical Venous Thromboembolism Diagnoses of Patients Undergoing Lower Limb Orthopaedic Surgery in the Danish National Patient Registry. Clin Epidemiol. 2022;14:191–199. Published 2022 Feb 17. doi:10.2147/CLEP.S345293.
11.
Aggarwal S, Patel S, Vashisht S, et al. Guidelines for the prevention of venous thromboembolism in hospitalized patients with pelvi-acetabular trauma. J Clin Orthop Trauma. 2020;11(6):1002–1008. doi:10.1016/j.jcot.2020.09.011.
12.
Lim PK, Ahn J, Scolaro JA. Venous Thromboembolism Prophylaxis After Pelvic and Acetabular Fractures: A Survey of Orthopaedic Surgeons’ Current Practices. J Am Acad Orthop Surg. 2020;28(18):750–755. doi:10.5435/JAAOS-D-19-00409.
13.
Kirchner T, Lefering R, Sandkamp R, et al. Thromboembolic complications among multiple injured patients with pelvic injuries: identifying risk factors for possible patient-tailored prophylaxis. World J Emerg Surg. 2021;16(1):42. Published 2021 Aug 26. doi:10.1186/s13017-021-00388-7.
14.
Lowe JA, Mitchell SM, Agarwal S, Jones CB. The Incidence of Venous Thromboembolism Following Pelvic and Lower Extremity Trauma Despite Adherence to Modern Prophylactic Protocols. J Orthop Trauma. 2020;34(8):418–421. doi:10.1097/BOT.0000000000001790.
15.
Pirkle S, Cook DJ, Kaskovich S, et al. Comparing Bleeding and Thrombotic Rates in Spine Surgery: An Analysis of 119 888 Patients. Global Spine J. 2021;11(2):161–166. doi:10.1177/2192568219896295.
16.
Alvarado AM, Porto GBF, Wessell J, Buchholz AL, Arnold PM. Venous Thromboprophylaxis in Spine Surgery. Global Spine J. 2020;10(1 Suppl):65S-70S. doi:10.1177/2192568219858307.
17.
Solaru S, Alluri RK, Wang JC, Hah RJ. Venous Thromboembolism Prophylaxis in Elective Spine Surgery. Global Spine J. 2021;11(7):1148–1155. doi:10.1177/2192568220962439.
18.
Zhang L, Cao H, Chen Y, Jiao G. Risk factors for venous thromboembolism following spinal surgery: A meta-analysis. Medicine (Baltimore). 2020;99(29):e20954. doi:10.1097/MD.0000000000020954.
19.
Lex JR, Evans S, Cool P, et al. Venous thromboembolism in orthopaedic oncology. Bone Joint J. 2020;102-B(12):1743–1751. doi:10.1302/0301-620X.102B12.BJJ-2019-1136.R3.
20.
Donahue A. Sobol KR. Abraham JA. Venous thromboembolism in musculoskeletal oncology surgery. Ann Joint. 2022;7:39. doi:10.21037/aoj-20-107.
21.
You DZ, Krzyzaniak H, Viner B, et al. Thromboembolic complications after surgical fixation of bone metastases: A systematic review. J Surg Oncol. 2021;124(7):1182–1191. doi:10.1002/jso.26601.
22.
Mancini MR, LeVasseur MR, Hawthorne BC, Marrero DE, Mazzocca AD. Venous thromboembolism complications in shoulder surgery: current concepts. J ISAKOS. 2021;6(5):283–289. doi:10.1136/jisakos-2020-000538.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.