Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Cardiovascular Magnetic Resonance Imaging in Physically Fit Young Patients Sans Comorbidities Who Recently Recovered from Coronavirus Disease 2019 (COVID-19)
1
Central Clinical Hospital of the Ministry of the Interior and Administration, Warsaw, Poland
2
Mossakowski Medical Research Centre, Polish Academy of Sciences, Warsaw, Poland
3
Centre of Postgraduate Medical Education, Warsaw, Poland
4
The Ohio State University Division of Cardiovascular Medicine, Columbus, United States of America
Corresponding author
Agnieszka Pawlak
Central Clinical Hospital of the Ministry of the Interior and Administration, Warsaw, Poland.
Central Clinical Hospital of the Ministry of the Interior and Administration, Warsaw, Poland.
Ann Agric Environ Med. 2024;31(3):357-361
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Multiple studies showed that patients with a severe course of COVID-19 may develop cardiovascular complications. Assessment of the incidence of myocardial injury in young, physically fit male patients with no comorbidities, and asymptomatic/mild course of the disease who recovered from COVID-19.
Material and methods:
A prospective, single-center, observational cohort study of 75 young (median[IQR] age 22 years) physically fit male patients, without comorbidities and smoking who recently recovered from COVID-19. Results were compared with a control group of age-matched, physically fit men with no comorbidities who tested negative for SARS-CoV-2.
Results:
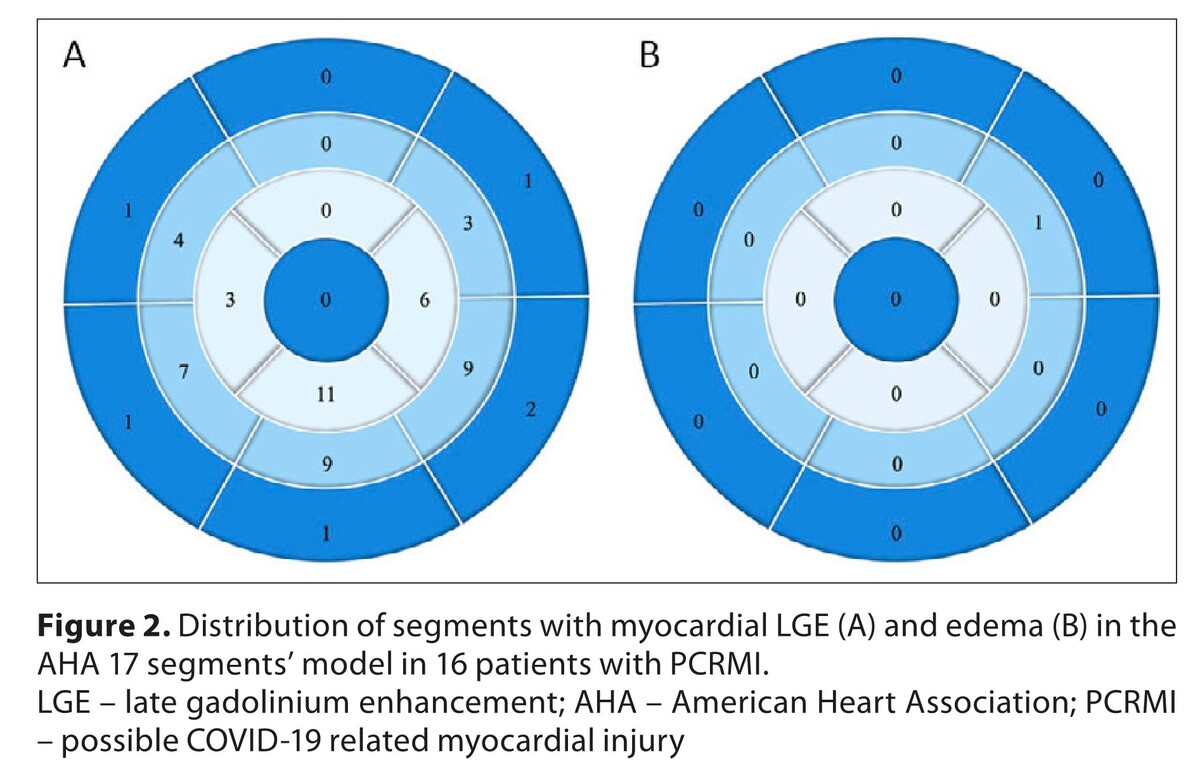
19(25%) patients had possible COVID-19 related myocardial injury[PCRMI] on cardiovascular magnetic resonance [CMR] including definitive myocarditis (n=1;1.3%) and possible myocarditis (n=3;4%). Other abnormalities: mildly decreased (<50%) left ventricular(LV) ejection fraction (n=4;5%), increased LV end-diastolic volume index (n=8;11%) and LV mass index (n=9;12%). Patients with PCRMI had higher NT-pro-BNP level (29 vs 20pg/mL respectively, P=0.02) and lower LV ejection fraction (55% vs 59% respectively, P=0.03). PCRMI was demonstrated in 3(27%) volunteers from the control group based on the presence of LGE (2/18%) and decreased LV ejection fraction (1/9%). No volunteer from the control group was diagnosed with definitive or possible myocarditis.
Conclusions:
PCRMI was a frequent finding in young, asymptomatic, physically-fit patients sans comorbidities relatively late after recovery from COVID-19. Whereas no definitive or possible myocarditis was found in the control group, LGE was relatively frequent suggesting that our findings might not be COVID-19 specific. This warrants a need for further investigation into the long-term cardiovascular consequences of COVID-19.
Multiple studies showed that patients with a severe course of COVID-19 may develop cardiovascular complications. Assessment of the incidence of myocardial injury in young, physically fit male patients with no comorbidities, and asymptomatic/mild course of the disease who recovered from COVID-19.
Material and methods:
A prospective, single-center, observational cohort study of 75 young (median[IQR] age 22 years) physically fit male patients, without comorbidities and smoking who recently recovered from COVID-19. Results were compared with a control group of age-matched, physically fit men with no comorbidities who tested negative for SARS-CoV-2.
Results:
19(25%) patients had possible COVID-19 related myocardial injury[PCRMI] on cardiovascular magnetic resonance [CMR] including definitive myocarditis (n=1;1.3%) and possible myocarditis (n=3;4%). Other abnormalities: mildly decreased (<50%) left ventricular(LV) ejection fraction (n=4;5%), increased LV end-diastolic volume index (n=8;11%) and LV mass index (n=9;12%). Patients with PCRMI had higher NT-pro-BNP level (29 vs 20pg/mL respectively, P=0.02) and lower LV ejection fraction (55% vs 59% respectively, P=0.03). PCRMI was demonstrated in 3(27%) volunteers from the control group based on the presence of LGE (2/18%) and decreased LV ejection fraction (1/9%). No volunteer from the control group was diagnosed with definitive or possible myocarditis.
Conclusions:
PCRMI was a frequent finding in young, asymptomatic, physically-fit patients sans comorbidities relatively late after recovery from COVID-19. Whereas no definitive or possible myocarditis was found in the control group, LGE was relatively frequent suggesting that our findings might not be COVID-19 specific. This warrants a need for further investigation into the long-term cardiovascular consequences of COVID-19.
REFERENCES (16)
1.
Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5.
2.
Long B, Brady WJ, Koyfman A, et al. Cardiovascular complications in COVID-19. Am J Emerg Med. 2020;38(7):1504–1507. doi:10.1016/j.ajem.2020.04.048.
3.
Shi S, Qin M, Cai Y, et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020;41(22):2070–2079. doi:10.1093/eurheartj/ehaa408.
4.
Pillai A, Lawson B. Coronavirus disease 2019 and cardiovascular diseases: collateral damage? Curr Opin Anaesthesiol. 2022;35(1):5–11. doi:10.1097/ACO.0000000000001076.
5.
Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265–1273. doi:10.1001/jamacardio.2020.3557. Erratum in: JAMA Cardiol. 2020 Nov 1;5(11):1308.
6.
Friedrich MG, Sechtem U, Schulz-Menger J, et al. International Consensus Group on Cardiovascular Magnetic Resonance in Myocarditis. Cardiovascular magnetic resonance in myocarditis: A JACC White Paper. J Am Coll Cardiol. 2009;53(17):1475–87. doi:10.1016/j.jacc.2009.02.007.
7.
Huang L, Zhao P, Tang D, et al. Cardiac Involvement in Patients Recovered From COVID-2019 Identified Using Magnetic Resonance Imaging. JACC Cardiovasc Imaging. 2020;13(11):2330–2339. doi:10.1016/j.jcmg.2020.05.004.
8.
Rajpal S, Tong MS, Borchers J, et al. Cardiovascular Magnetic Resonance Findings in Competitive Athletes Recovering From COVID-19 Infection. JAMA Cardiol. 2021 Jan 1;6(1):116–118. doi:10.1001/jamacardio.2020.4916. Erratum in: JAMA Cardiol. 2021;6(1):123.
9.
Tanacli R, Doeblin P, Götze C, et al. COVID-19 vs. Classical Myocarditis Associated Myocardial Injury Evaluated by Cardiac Magnetic Resonance and Endomyocardial Biopsy. Front Cardiovasc Med. 2021;8:737257. doi:10.3389/fcvm.2021.737257.
10.
Wiesmueller M, Wuest W, Heiss R, et al. Cardiac T2 mapping: robustness and homogeneity of standardized in-line analysis. J Cardiovasc Magn Reson. 2020;22(1):39. doi:10.1186/s12968-020-00619-x.
11.
Nakamura M, Kido T, Hirai K, et al. What is the mid-wall linear high intensity “lesion” on cardiovascular magnetic resonance late gadolinium enhancement? J Cardiovasc Magn Reson. 2020;22(1):66. doi:10.1186/s12968-020-00665-5.
12.
Mahrholdt H, Goedecke C, Wagner A, et al. Cardiovascular magnetic resonance assessment of human myocarditis: a comparison to histology and molecular pathology. Circulation. 2004;109(10):1250–8. doi:10.1161/01.CIR.0000118493.13323.81.
13.
Eiros R, Barreiro-Pérez M, Martín-García A, et al. Afección pericárdica y miocárdica tras infección por SARS-CoV-2: estudio descriptivo transversal en trabajadores sanitarios [Pericardial and myocardial involvement after SARS-CoV-2 infection: a cross-sectional descriptive study in healthcare workers]. Rev Esp Cardiol. 2022;75(9):735–747. doi:10.1016/j.recesp.2021.10.021.
14.
Inciardi RM, Lupi L, Zaccone G, et al. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5(7):819–824. doi:10.1001/jamacardio.2020.1096.
15.
Li H, Liu L, Zhang D, et al. SARS-CoV-2 and viral sepsis: observations and hypotheses. Lancet. 2020;395(10235):1517–1520. doi: 10.1016/S0140-6736(20)30920-X.
16.
Ferreira VM, Schulz-Menger J, Holmvang G, et al. Cardiovascular Magnetic Resonance in Nonischemic Myocardial Inflammation: Expert Recommendations. J Am Coll Cardiol. 2018;72(24):3158–3176. doi:10.1016/j.jacc.2018.09.072.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.