Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
REVIEW PAPER
Bioterrorism potential of haemorrhagic fever viruses – occupational and environmental Implications of filoviruses and arenaviruses
1
Biohazard Prevention Centre, University of Łódź, Łódź, Poland
Ann Agric Environ Med. 2025;32(2):173-184
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
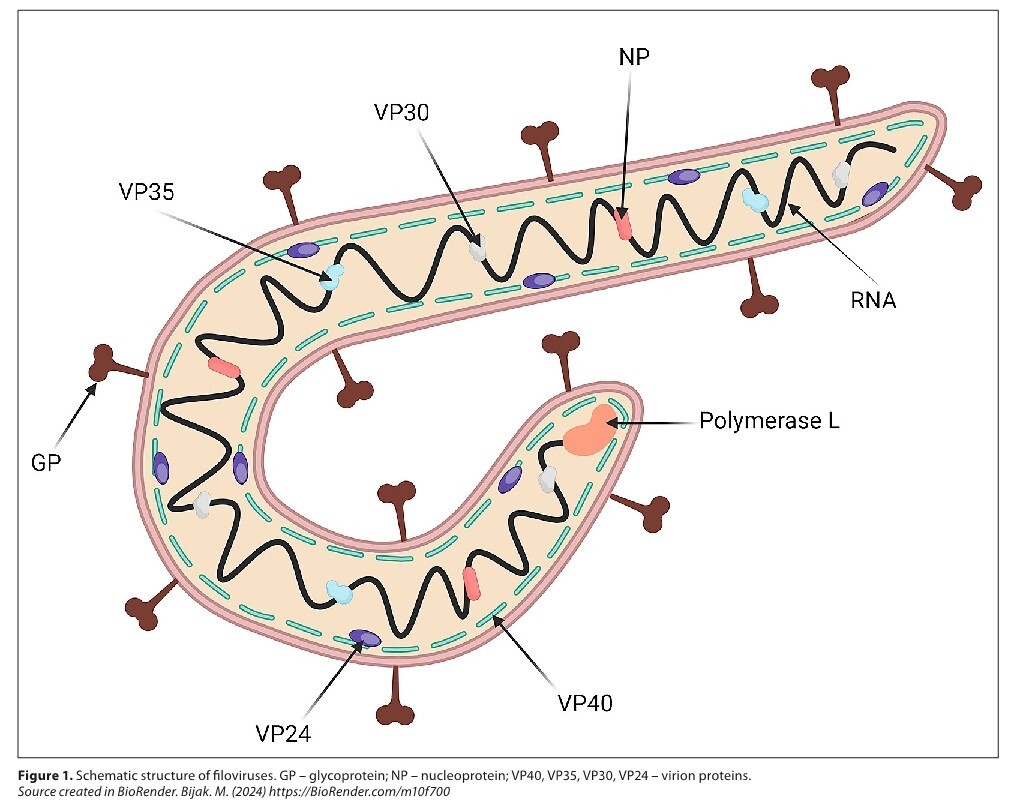
Viral haemorrhagic fevers (VHFs), caused by filoviruses (e.g., Ebola virus, Marburg virus) and arenaviruses (e.g., Lassa virus, Machupo virus), represent a significant bioterrorism threat due to their zoonotic origins, high mortality rates, and severe clinical presentations. This review examines the potential use of VHFs as biological weapons, their zoonotic transmission dynamics, and implications for rural and agricultural health.
Review methods:
A comprehensive review was conducted using electronic databases, including PubMed and Scopus, focusing on studies addressing VHFs in the context of bioterrorism and zoonotic disease transmission. Studies published between 2016 – 2024 were included, with search terms such as ‘viral haemorrhagic fevers’’, ‘bioterrorism potential’, and ‘zoonotic transmission’.
Brief description of the state of knowledge:
VHFs are zoonotic diseases transmitted to humans from animal reservoirs, primarily rodents and bats. Their pathogenicity, coupled with potential for engineered transmission, underscores their bioterrorism risk. Rural and agricultural communities face heightened exposure due to their proximity to these natural reservoirs.
Summary:
While these viruses are rare and unstable in natural settings, the prospect of their genetic manipulation or combination in order to create novel pathogens introduces new avenues for their potential use in bioterrorism. It is imperative to comprehensively understand their pathogenesis and to establish rigorous control and prevention measures to mitigate their impact on public health and safety. The ongoing vigilance and preparedness efforts are essential to counteract the potential threat posed by these agents in bioterrorism scenarios.
Viral haemorrhagic fevers (VHFs), caused by filoviruses (e.g., Ebola virus, Marburg virus) and arenaviruses (e.g., Lassa virus, Machupo virus), represent a significant bioterrorism threat due to their zoonotic origins, high mortality rates, and severe clinical presentations. This review examines the potential use of VHFs as biological weapons, their zoonotic transmission dynamics, and implications for rural and agricultural health.
Review methods:
A comprehensive review was conducted using electronic databases, including PubMed and Scopus, focusing on studies addressing VHFs in the context of bioterrorism and zoonotic disease transmission. Studies published between 2016 – 2024 were included, with search terms such as ‘viral haemorrhagic fevers’’, ‘bioterrorism potential’, and ‘zoonotic transmission’.
Brief description of the state of knowledge:
VHFs are zoonotic diseases transmitted to humans from animal reservoirs, primarily rodents and bats. Their pathogenicity, coupled with potential for engineered transmission, underscores their bioterrorism risk. Rural and agricultural communities face heightened exposure due to their proximity to these natural reservoirs.
Summary:
While these viruses are rare and unstable in natural settings, the prospect of their genetic manipulation or combination in order to create novel pathogens introduces new avenues for their potential use in bioterrorism. It is imperative to comprehensively understand their pathogenesis and to establish rigorous control and prevention measures to mitigate their impact on public health and safety. The ongoing vigilance and preparedness efforts are essential to counteract the potential threat posed by these agents in bioterrorism scenarios.
FUNDING
The research was supported by The National Centre for Research and Development, Warsaw, Poland (Grant No. DOB-SZAFIR/12/A/029/01/2021).
REFERENCES (60)
1.
Chakraborty P, et al. Poxviruses as Agents of Biological Warfare: The Importance of Ensuring Ethical Standards for Research with Viruses. Adv Exp Med Biol. 2024;1451:399–412.
2.
Oliveira M, et al. Biowarfare, bioterrorism and biocrime: A historical overview on microbial harmful applications. Forensic Sci Int. 2020;314:110366.
3.
Berger T, et al. Toxins as biological weapons for terror-characteristics, challenges and medical countermeasures: a mini-review. Disaster Mil Med. 2016;2:7.
4.
Flórez-Álvarez L, et al. Hemorrhagic fever viruses: Pathogenesis, therapeutics, and emerging and re-emerging potential. Front Microbiol. 2022;13:1040093.
5.
Aloke C, et al. Combating Lassa Fever in West African Sub-Region: Progress, Challenges, and Future Perspectives. Virus. 2023;15(1).
6.
Silva-Ramos CR, et al. Bolivian hemorrhagic fever: A narrative review. Travel Med Infect Dis. 2021;40:102001.
7.
Lendino A, et al. A review of emerging health threats from zoonotic New World mammarenaviruses. BMC Microbiol. 2024;24(1):115.
8.
Dembek Z, et al. Ebola Virus Disease Outbreaks: Lessons Learned From Past and Facing Future Challenges. Mil Med. 2024.
9.
Mitu RA, Islam MR. The Current Pathogenicity and Potential Risk Evaluation of Marburg Virus to Cause Mysterious “Disease X”—An Update on Recent Evidences. Environmental Health Insights, 2024. 18:11786302241235809.
10.
Kuno G. Mechanisms of Yellow Fever Transmission: Gleaning the Overlooked Records of Importance and Identifying Problems, Puzzles, Serious Issues, Surprises and Research Questions. Viruses. 2024;16. doi:10.3390/v16010084.
11.
Baak-Baak CM, et al. Entomological and virological surveillance for dengue virus in churches in Merida, Mexico. Rev Inst Med Trop Sao Paulo. 2019;61:e9.
12.
Lapa D, et al. Rift Valley Fever Virus: An Overview of the Current Status of Diagnostics. Biomedicines. 2024;12. doi:10.3390/biomedicines12030540.
13.
Messina JP, Wint GRW. The Spatial Distribution of Crimean–Congo Haemorrhagic Fever and Its Potential Vectors in Europe and Beyond. Insects. 2023;14, doi:10.3390/insects14090771.
14.
Emanuel J, Marzi A, Feldmann H. Filoviruses: Ecology, Molecular Biology, and Evolution. Adv Virus Res. 2018;100:189–221.
15.
Peng R, et al. Structural insight into arenavirus replication machinery. Nature. 2020;579(7800):615–619.
16.
Levine CB, Mire CE, Geisbert TW. Comparison of Zaire and Bundibugyo Ebolavirus Polymerase Complexes and Susceptibility to Antivirals through a Newly Developed Bundibugyo Minigenome System. J Virol. 2021;95(20):e0064321.
17.
Woolsey C, et al. Natural history of Sudan ebolavirus infection in rhesus and cynomolgus macaques. Emerg Microbes Infect. 2022;11(1):1635–1646.
18.
Abaatyo J, et al. Psychological distress among healthcare professionals in Mbarara, following the 2022 Ebola Virus Disease outbreak in Uganda: a mixed methods study. BMC Psychiatry. 2024;24(1):469.
19.
Jalloh MB, Round JA. The 2014 West Africa Ebola crisis: lessons from UK Defence Healthcare Engagement in Sierra Leone. BMJ Mil Health, 2024.
20.
Mandizadza OO, Phebeni RT, Ji C. Prevalence of somatic symptoms among Ebola Virus Disease (EVD) survivors in Africa: a systematic review and meta-analysis. BMC Public Health. 2024;24(1):1511.
21.
Hussein HA. Brief review on ebola virus disease and one health approach. Heliyon. 2023;9(8):e19036.
22.
Leendertz SA, et al. Assessing the Evidence Supporting Fruit Bats as the Primary Reservoirs for Ebola Viruses. Ecohealth. 2016;13(1):18–25.
23.
Akoi Boré J, et al. Serological evidence of zoonotic filovirus exposure among bushmeat hunters in Guinea. Nat Commun. 2024;15(1):4171.
24.
Kiiza P, et al. Treatment of Ebola-related critical illness. Intensive Care Med. 2020;46(2):285–297.
25.
Tshiani Mbaya O, Mukumbayi P, Mulangu S. Review: Insights on Current FDA-Approved Monoclonal Antibodies Against Ebola Virus Infection. Front Immunol. 2021;12:721328.
26.
Iversen PL, et al. Recent successes in therapeutics for Ebola virus disease: no time for complacency. Lancet Infect Dis. 2020;20(9):e231–e237.
27.
Malik S, et al. Ebola Virus Disease Vaccines: Development, Current Perspectives & Challenges. Vaccines (Basel), 2023;11(2).
28.
Agnandji ST, et al. Readiness in preventing filovirus epidemics by use of the marketed vaccines against Zaire Ebola virus disease as prototypes. Lancet Infect Dis. 2024;24(7):671–673.
29.
Senga M, et al. Contact tracing performance during the Ebola virus disease outbreak in Kenema district, Sierra Leone. Philos Trans R Soc Lond B Biol Sci. 2017;372(1721).
30.
Sibomana O, Kubwimana E. First-ever Marburg virus disease outbreak in Equatorial Guinea and Tanzania: An imminent crisis in West and East Africa. Immun Inflamm Dis. 2023;11(8):e980.
31.
Kinyenje E, et al. Infection prevention and control of highly infectious pathogens in resource-limited countries: an experience from Marburg viral disease outbreak in Kagera Region – Tanzania. BMC Infect Dis. 2024;24(1):628.
32.
Srivastava S, et al. Emergence of Marburg virus: a global perspective on fatal outbreaks and clinical challenges. Front Microbiol. 2023;14:1239079.
33.
Lyu Y, et al. Mapping knowledge landscapes and emerging trends of Marburg virus: A text-mining study. Heliyon. 2024;10(8):e29691.
34.
Geldenhuys M, et al. Host-Associated Distribution of Two Novel Mammarenaviruses in Rodents from Southern Africa. Viruses. 2022;15(1).
35.
Fénéant L, et al. Generation of Reporter-Expressing New World Arenaviruses: A Systematic Comparison. Viruses. 2022; 4(7).
36.
Kim YJ, Venturini V, de la Torre JC. Progress in Anti-Mammarenavirus Drug Development. Viruses. 2021;13(7).
37.
Islam MR, Akash S, Rahman MM. Epidemiology, symptoms, transmission, prevention, treatment, and future prospects of the Lassa fever outbreak: a potential study. Int J Surg. 2023;109(3):531–533.
38.
Ilesanmi O, et al. Pulmonary involvement in lassa fever: a scoping review. Disaster Emerg Med J. 2023;8(2):97–109.
39.
Happi AN, et al. Increased Prevalence of Lassa Fever Virus-Positive Rodents and Diversity of Infected Species Found during Human Lassa Fever Epidemics in Nigeria. Microbiol Spectr. 2022;10(4):e0036622.
40.
Salam AP, et al. Ribavirin for treating Lassa fever: A systematic review of pre-clinical studies and implications for human dosing. PLoS Negl Trop Dis. 2022;16(3):e0010289.
41.
Cross RW, et al. A human monoclonal antibody combination rescues nonhuman primates from advanced disease caused by the major lineages of Lassa virus. Proceed National Academy Sci. 2023;120(34):e2304876120.
42.
Asogun DA, et al. Lassa Fever: Epidemiology, Clinical Features, Diagnosis, Management and Prevention. Infect Dis Clin North Am. 2019;33(4):933–951.
43.
Toledo J, et al. Public health implications of a new world arenavirus outbreak that occurred in Bolivia, 2019. Travel Med Infect Dis. 2021;43:102124.
44.
Williams EP, et al. Common Themes in Zoonotic Spillover and Disease Emergence: Lessons Learned from Bat- and Rodent-Borne RNA Viruses. Viruses. 2021;13(8).
45.
Frank MG, et al. South American Hemorrhagic Fevers: A summary for clinicians. Inter J Infect Dis. 2021;105:505–515.
46.
Koma T, et al. Machupo Virus Expressing GPC of the Candid#1 Vaccine Strain of Junin Virus Is Highly Attenuated and Immunogenic. J Virol. 2016;90(3):1290–7.
47.
Wang CC, et al. Airborne transmission of respiratory viruses. Science. 2021;373(6558).
48.
Panghal A, Flora SJS. Chapter 4 – Viral agents including threat from emerging viral infections. In: Handbook on Biological Warfare Preparedness. Flora SJS, Pachauri V, editors. 2020, Academic Press. p. 65–81. https://doi.org/10.1016/B978-0....
49.
Dean NE, et al. Transmissibility and Pathogenicity of Ebola Virus: A Systematic Review and Meta-analysis of Household Secondary Attack Rate and Asymptomatic Infection. Clin Infect Dis. 2016;62(10):1277–1286.
50.
Choi Y, Kim Y. Application of multiplex realtime PCR detection for hemorrhagic fever syndrome viruses. J Infect Public Health. 2023;16(12):1933–1941.
51.
Hewson R. Understanding Viral Haemorrhagic Fevers: Virus Diversity, Vector Ecology, and Public Health Strategies. Pathogens. 2024;13(10).
52.
Ftika L, Maltezou HC. Viral haemorrhagic fevers in healthcare settings. J Hosp Infect. 2013;83(3):185–92.
53.
Tarantola A, Abiteboul D, Rachline A. Infection risks following accidental exposure to blood or body fluids in health care workers: a review of pathogens transmitted in published cases. Am J Infect Control. 2006;34(6):367–75.
54.
Commision E. European Guidelines for the clinical management of haemorrhagic fever viruses and bioterrorism-related haemorrhagic fever viruses 2004 [cited 2025 13/02/25]; Available from: https://health.ec.europa.eu/pu....
55.
WHO. Clinical management of patients with viral haemorrhagic fever: A pocket guide for front-line health workers. 2016 [cited 2025 13/02/25]; Available from: https://www.who.int/publicatio....
56.
Gonzalez JP, Souris M, Valdivia-Granda W. Global Spread of Hemorrhagic Fever Viruses: Predicting Pandemics. Methods Mol Biol. 2018;1604:3–31.
57.
Horefti E. The Importance of the One Health Concept in Combating Zoonoses. Pathogens. 2023;12(8).
58.
Calistri P, et al. 2021 EFSA/IZSAM Animal Health Crisis Preparedness Exercise with Mediterranean Countries. EFSA Supporting Publications, 2021.18.
60.
Duah JK, et al. Points of entry dynamics: understanding the cross-border threats for Ebola virus disease and COVID-19 in Ghana using a logic model approach. J Public Health Afr. 2023;14(4):2264.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.