Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Association between dietary variety and anthropometric parameters in community-dwelling older adults: results of a population-based PolSenior study
1
Department of Human Nutrition, Institute of Human Nutrition Sciences, Warsaw University of Life Sciences (SGGW-WULS), Warsaw, Poland
2
‘Study on Ageing and Longevity’, International Institute of Molecular and Cell Biology, Warsaw, Poland
Corresponding author
Elżbieta Wierzbicka
Department of Human Nutrition, Institute of Human Nutrition Sciences, Warsaw University of Life Sciences (SGGW-WULS), Warsaw, Poland
Department of Human Nutrition, Institute of Human Nutrition Sciences, Warsaw University of Life Sciences (SGGW-WULS), Warsaw, Poland
Ann Agric Environ Med. 2024;31(3):460-471
KEYWORDS
anthropometric parametersnutritionbody mass indexwaist circumferenceolder adultswaist-to-hip ratiodiet qualitydietary varietyPolSenior study
TOPICS
ABSTRACT
Introduction and objective:
Dietary variety (DV) is recognized as a key indicator of diet quality. It is based on the premise that eating a wide variety of foods ensures an adequate intake of essential nutrients which, in turn, leads to better diet quality. The aim of the study is to examine the relationships between DV, diet quality and selected anthropometric parameters in older adults.
Material and methods:
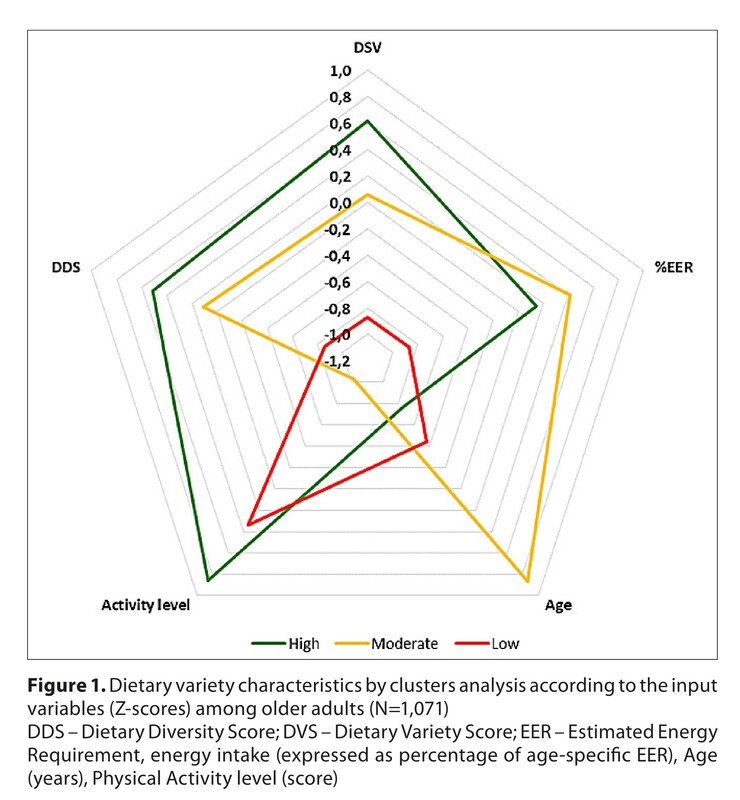
A cross-sectional analysis was conducted on 1,071 participants (average age: 72.8 years) from a population cohort of older adults living in Poland. DV was measured using the Dietary Variety Score (DVS) and Dietary Diversity Score (DDS), based on 3-day food records. The associations between DV and anthropometric parameters were examined using cluster analysis. Three clusters were identified: high DV (Cluster 1 – 33%), moderate DV (Cluster 2 – 41%) and low DV (Cluster 3 – 26%).
Results:
Moderate DV showed a positive relationship with lower BMI values, particularly in women (p<0.05). High and moderate DV was inversely associated with lower values of abdominal adiposity measures, compared to the low DV in the women group only (p<0.05). The diet quality score was greater in the high DV, compared to the low DV (12.6 vs. 7.5; p<0.001). Low DV constituted a high-risk group and had the lowest intake of energy (100% participants) and almost all nutrients, especially protein (62%) and micronutrients (>30-96%; depending on the nutrient).
Conclusions:
A higher degree of DV was associated with better anthropometric parameters in older adults. These relationships were more pronounced in women than in men. High DV improves the intake levels of energy, protein and micronutrients, and also enhances overall dietary quality. Older adults require personalized guidance and dietary support, including a high dietary variety of nutrient-dense foods/food groups.
Dietary variety (DV) is recognized as a key indicator of diet quality. It is based on the premise that eating a wide variety of foods ensures an adequate intake of essential nutrients which, in turn, leads to better diet quality. The aim of the study is to examine the relationships between DV, diet quality and selected anthropometric parameters in older adults.
Material and methods:
A cross-sectional analysis was conducted on 1,071 participants (average age: 72.8 years) from a population cohort of older adults living in Poland. DV was measured using the Dietary Variety Score (DVS) and Dietary Diversity Score (DDS), based on 3-day food records. The associations between DV and anthropometric parameters were examined using cluster analysis. Three clusters were identified: high DV (Cluster 1 – 33%), moderate DV (Cluster 2 – 41%) and low DV (Cluster 3 – 26%).
Results:
Moderate DV showed a positive relationship with lower BMI values, particularly in women (p<0.05). High and moderate DV was inversely associated with lower values of abdominal adiposity measures, compared to the low DV in the women group only (p<0.05). The diet quality score was greater in the high DV, compared to the low DV (12.6 vs. 7.5; p<0.001). Low DV constituted a high-risk group and had the lowest intake of energy (100% participants) and almost all nutrients, especially protein (62%) and micronutrients (>30-96%; depending on the nutrient).
Conclusions:
A higher degree of DV was associated with better anthropometric parameters in older adults. These relationships were more pronounced in women than in men. High DV improves the intake levels of energy, protein and micronutrients, and also enhances overall dietary quality. Older adults require personalized guidance and dietary support, including a high dietary variety of nutrient-dense foods/food groups.
ACKNOWLEDGEMENTS
The study was conducted as part of the project ‘Medical, psychological, sociological and economic aspects of aging in Poland’ – PolSenior, funded by the Ministry of Science and Higher Education (PBZMEIN-9/2/2006) in Warsaw, Poland, and supported by the Polish Ministry of Education and Science within funds of the Institute of Human Nutrition Sciences, Warsaw University of Life Sciences (WULS) for scientific research.
REFERENCES (58)
1.
Eurostat Database. Population structure and ageing. Available from: https://ec.europa.eu/eurostat/... (Accessed at: 2024.02.25).
2.
Bojang KP, Manchana V. Nutrition and healthy aging: a review. Curr Nutr Rep. 2023;12(3):369–375. https://doi.org/10.1007/s13668....
3.
Kehoe L, Walton J, Flynn A. Nutritional challenges for older adults in Europe: current status and future directions. Proc Nutr Soc. 2019;78(2):221–233. https://doi.org/10.1017/S00296....
4.
Santos AL, Sinha S. Obesity and aging: Molecular mechanisms and therapeutic approaches. Ageing Res Rev. 2021;67:101268. https://doi:10.1016/j.arr.2021....
5.
Krzysztoszek J, Laudanska-Krzeminska I, Bronikowski M. Assessment of epidemiological obesity among adults in EU countries. Ann Agric Environ Med. 2019;26(2):341–349. https://doi.org/10.26444/aaem/....
6.
Khanna D, Peltzer C, Kahar P, Parmar MS. Body Mass Index (BMI): A Screening Tool Analysis. Cureus. 2022;14(2):e22119. https://doi:10.7759/cureus.221....
7.
Tylutka A, Morawin B, Walas Ł, et al. Assessment of metabolic syndrome predictors in relation to inflammation and visceral fat tissue in older adults. Sci Rep. 2023;1389. https://doi.org/10.1038/s41598....
8.
Robinson SM. Improving nutrition to support healthy ageing: what are the opportunities for intervention? Proc Nutr Soc. 2018;77(3):257–264. https://doi:10.1017/S002966511....
9.
Zampino M, AlGhatrif M, Kuo PL, et al. Longitudinal Changes in Resting Metabolic Rates with Aging Are Accelerated by Diseases. Nutrients. 2020;12(10):3061. https://doi.org/10.3390/nu1210....
10.
Herforth A, Arimond M, Álvarez-Sánchez C, et al. A global review of food-based dietary guidelines. Adv Nutr. 2019;10(4):590–605. https://doi.org/10.1093/advanc....
11.
de Oliveira Otto MC, Anderson CAM, Dearborn JL, et al. Dietary Diversity: Implications for Obesity Prevention in Adult Populations: A Science Advisory From the American Heart Association. Circulation. 2018;138:e160–e168. https://doi:10.1161/CIR.000000....
12.
Mozaffari H, Hosseini Z, Lafrenière J, et al. Is eating a mixed diet better for health and survival?: A systematic review and meta-analysis of longitudinal observational studies. Crit Rev Food Sci Nutr. 2022;62(29):8120–8136. https://doi:10.1080/10408398.2....
13.
Jang W, Shin Y, Kim Y. Dietary Pattern Accompanied with a High Food Variety Score Is Negatively Associated with Frailty in Older Adults. Nutrients. 2021;13(9):3164. https://doi:10.3390/nu13093164.
14.
Lo YTC, Wahlqvist ML, Huang YC, et al. Medical costs of a low skeletal muscle mass are modulated by dietary diversity and physical activity in community-dwelling older Taiwanese: a longitudinal study. Int J Behav Nutr Phys Act. 2017;14(1):31. https://doi:10.1186/s12966-017....
15.
Zheng J, Zhou R, Li F, et al. Association between dietary diversity and cognitive impairment among the oldest-old: Findings from a nationwide cohort study. Clin Nutr. 2021;40(4):1452–1462. https://doi:10.1016/j.clnu.202....
16.
Huang X, Gao Y, Chen W, et al. Dietary variety relates to gut microbiota diversity and abundance in humans. Eur J Nutr. 2022;61:3915–3928. https://doi.org/10.1007/s00394....
17.
Torres-Collado L, García-de La Hera M, Cano-Ibañez N, et al. Association between Dietary Diversity and All-Cause Mortality: A Multivariable Model in a Mediterranean Population with 18 Years of Follow-Up. Nutrients. 2022;14(8):1583. https://doi:10.3390/nu14081583.
18.
Hsiao FY, Peng LN, Lee WJ, et al. Higher dietary diversity and better healthy aging: A 4-year study of community-dwelling middle-aged and older adults from the Taiwan Longitudinal Study of Aging. Exp Gerontol. 2022;168:111929. https://doi.org/10.1016/j.exge....
19.
Shuremu M, Abate KH, Belachew T. Effect of nutrition education intervention to improve dietary diversity practice and nutritional status of the older people: A cluster randomized controlled trial. Food Sci Nutr. 2023;11(11):7383–7395. https://doi:10.1002/fsn3.3667.
20.
Cano-Ibáñez N, Gea A, Martínez-González MA, et al. Dietary diversity and nutritional adequacy among an older Spanish population with metabolic syndrome in the PREDIMED-plus study: A cross-sectional analysis. Nutrients, 2019;11(5):958. https://doi:10.3390/nu11050958.
21.
Guan ST, Lai HY, Chen LK, et al. Advancing nutrition risk assessment in middle-aged and older individuals with diverse food cultures: A data-driven personalized approach to predict incident hypertension, diabetes and mortality. J Nutr Health Aging. 2024;28(2):100025. https://doi.org/10.1016/j.jnha....
22.
Jacquemot AF, Prat R, Gazan R, et al. Development and validation of an occurrence-based healthy dietary diversity (ORCHID) score easy to operationalise in dietary prevention interventions in older adults: a French study. Br J Nutr. 2023;131(6):1053–1063. https://doi.org/10.1017/S00071....
23.
Verger EO, Le Port A, Borderon A, et al. Dietary Diversity Indicators and Their Associations with Dietary Adequacy and Health Outcomes: A Systematic Scoping Review. Adv Nutr. 2021;12(5):1659–1672. https://doi:10.1093/advances/n....
24.
Dello Russo M, Formisano A, Lauria F, et al. Dietary Diversity and Its Association with Diet Quality and Health Status of European Children, Adolescents, and Adults: Results from the I. Family Study. Foods. 2023;12(24):4458. https://doi.org/10.3390/foods1....
25.
Salehi-Abargouei A, Akbari F, Bellissimo N, et al. Dietary diversity score and obesity: a systematic review and meta-analysis of observational studies. Eur J Clin Nutr. 2016;70(1):1–9. https://doi:10.1038/ejcn.2015.....
26.
Blędowski P, Mossakowska M, Chudek J, et al. Medical, psychological and socioeconomic aspects of aging in Poland. Exp Geronol. 2011;46(12):1003–1009. https://doi:10.1016/j.exger.20....
27.
Wajszczyk B, Chwojnowska Z, Nasiadko D, Charzewska J. Instructions for the Use of the 5.0 Diet Program for Planning and Ongoing Evaluation of Individual and Collective Nutrition in Methodical Guide of Dietary Research [in Polish]. National Food and Nutrition Institute; Warsaw, 2015.
28.
Jarosz M, Rychlik E, Stoś K, Charzewska J. Dietary Reference Values for the Polish population and their application [in Polish]. Warsaw, Poland; 2020.
29.
Drewnowski A, Renderson SA, Driscoll A, et al. The Dietary Variety Score. J Am Diet Assoc. 1997;97(3):266–271. https://doi:10.1016/S0002-8223....
30.
Rathnayake KM, Madushani P, Silva K. Use of dietary diversity score as a proxy indicator of nutrient adequacy of rural elderly people in Sri Lanka. BMC Res Notes. 2012;5(1):469. https://doi:10.1186/1756-0500-....
31.
World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. Geneva: WHO Technical Report Series No. 894; 2000. p. 1–253.
32.
World Health Organization. Waist circumference and waist-hip ratio: report of a WHO expert consultation. Geneva. 8–11 December 2008. Available online: https://apps.who.int/iris/hand... (access: 2024.02.25).
33.
Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the Metabolic Syndrome: A Joint Interim Statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. https://doi:10.1161/circulatio....
34.
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis: Waist-to-height ratio as a screening tool. Obes Rev. 2012;13(3):275–286. https://doi:10.1111/j.1467–789....
35.
Ashwell M, Gibson S. Waist-to-height ratio as an indicator of ‘early health risk’: simpler and more predictive than using a ‘matrix ’based on BMI and waist circumference. BMJ Open. 2016;6(3):e010159. https://doi.org/10.1136/bmjope....
36.
Borda MG, Samuelsson J, Cederholm T, et al. Nutrient Intake and Its Association with Appendicular Total Lean Mass and Muscle Function and Strength in Older Adults: A Population-Based Study. Nutrients. 2024;16(4):568. https://doi.org/10.3390/nu1604....
37.
Padilla, CJ, Ferreyro FA, Arnold WD. Anthropometry as a readily accessible health assessment of older adults. Exp Gerontol. 2021;153:111464. https://doi.org/10.1016/j.exge....
38.
Ishikawa M, Moriya S, Yokoyama T. Relationship between diet-related indicators and overweight and obesity in older adults in rural Japan. J Nutr Health Aging. 2017;21(7):759–765. https://doi:10.1007/s12603-016....
39.
Gajda R, Raczkowska E, Sobieszczańska M, et al. Diet Quality Variation among Polish Older Adults: Association with Selected Metabolic Diseases, Demographic Characteristics and Socioeconomic Status. IJERPH. 2023;20(4):2878. https://doi:10.3390/ijerph2004....
40.
Geigl C, Loss J, Leitzmann M, et al. Social Factors of Dietary Risk Behavior in Older German Adults: Results of a Multivariable Analysis. Nutrients. 2022;14(5):1057. https://doi:10.3390/nu14051057.
41.
Puzianowska-Kuznicka M, Kuryłowicz A, Walkiewicz D, et al. Obesity Paradox in Caucasian Seniors: Results of the PolSenior Study. J Nutr Health Aging. 2019;23(9):796–804. https://doi:10.1007/s12603-019....
42.
Ćwirlej-Sozańska A, Wiśniowska-Szurlej A, Wilmowska-Pietruszyńska A, et al. Effect of body weight on disability and chronic disease rates in the elderly in south-eastern Poland. Ann Agric Environ Med. 2020;27(2):240–247. https://doi:10.26444/aaem/1085....
43.
Dramé M, Godaert L. The Obesity Paradox and Mortality in Older Adults: A Systematic Review. Nutrients. 2023;15(7):1780. https://doi:10.3390/nu15071780.
44.
Bosello O, Vanzo A. Obesity paradox and aging. Eat Weight Disord. 2021;26(1):27–35. https://doi:10.1007/s40519-019....
45.
Puzianowska-Kuznicka M, Kurylowicz A, Wierucki L, et al. Obesity in Caucasian Seniors on the Rise: Is It Truly Harmful? Results of the PolSenior2 Study. Nutrients. 2022;14(21):4621. https://doi:10.3390/nu14214621.
46.
Guo J, Shang Y, Fratiglioni L, et al. Individual changes in anthropometric measures after age 60 years: a 15-year longitudinal population-based study. Age and Ageing. 2021;50(5):1666–1674. https://doi:10.1093/ageing/afa....
47.
Lin S, Huang M, Yang L, et al. Dietary diversity and overweight are associated with high intrinsic capacity among Chinese urban older adults (2020–2021). Exp Gerontol. 2023;177:112194. https://doi:10.1016/j.exger.20....
48.
Norman K, Haß U, Pirlich M. Malnutrition in Older Adults-Recent Advances and Remaining Challenges. Nutrients. 2021;13(8):2764. https://doi:10.3390/nu13082764.
49.
Tucker E, Luscombe-Marsh N, Ambrosi C, et al. Nutritional status and quality-of-life of older adults in aged care: A systematic review and meta-analysis. Exp Gerontol. 2022;162:111764. https://doi:10.1016/j.exger.20....
50.
Niedźwiedzka E, Wądołowska L. A mini-nutritional assessment of older Poles in relation to the food intake model and food intake variety. Adv Med Sci. 2010;55(2):172–178. https://doi:10.2478/v10039-010....
51.
Vega-Cabello V, Struijk EA, Caballero FF, et al. Dietary Micronutrient Adequacy and Risk of Multimorbidity in Community-dwelling Older Adults. Am J Clin Nutr. 2023;118(1):34–40. https://doi:10.1016/j.ajcnut.2....
52.
van Dronkelaar C, Fultinga M, Hummel M, et al. Minerals and Sarcopenia in Older Adults: An Updated Systematic Review. J Am Med Dir Assoc. 2023;24(8):1163–1172. https://doi.org/10.1016/j.jamd....
53.
Embling R, Pink AE, Gatzemeier J, Price M, D Lee M, Wilkinson LL. Effect of food variety on intake of a meal: a systematic review and meta-analysis. Am J Clin Nutr. 2021;113(3):716–741. https://doi:10.1093/ajcn/nqaa3....
54.
Cristina NM, Lucia D. Nutrition and Healthy Aging: Prevention and Treatment of Gastrointestinal Diseases. Nutrients. 2021. 30;13(12):4337. https://doi: 10.3390/nu13124337.
55.
Kaur D, Rasane P, Singh J, et al. Nutritional Interventions for Elderly and Considerations for the Development of Geriatric Foods. Curr Aging Sci. 2019;12(1):15–27. https://doi: 10.2174/1874609812666190521110548.
56.
Sun C, Zhang WS, Jiang CQ, et al. Quantity and Variety in Fruit and Vegetable Consumption and Mortality in Older Chinese: A 15-year Follow-Up of a Prospective Cohort Study. J Nutr. 2023;153(7):2061–2072. https://doi: 10.1016/j.tjnut.2023.03.021.
57.
Delerue Matos A, Barbosa F, Cunha C, et al. Social isolation, physical inactivity and inadequate diet among European middle-aged and older adults. BMC Public Health 2021;21(1):924. https://doi.org/10.1186/s12889....
58.
Domper J, Gayoso L, Goni L, de la O V, Etxeberria U, Ruiz-Canela M. Culinary medicine and healthy ageing: a comprehensive review. Nutrition Res Rev. 2023;11:1–15. https://doi:10.1017/S095442242....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.