Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
Assessment of microcirculation among patients with obstructive sleep apnea after CPAP treatment
1
Chair and Department of Internal Medicine, Medical University, Lublin, Poland
2
Departament of Internal Medicine, 1st Military Hospital, Lublin, Poland
3
Department of Functional Research, Institute of Rural Health, Lublin, Poland
Corresponding author
Klaudia Brożyna-Tkaczyk
Chair and Department of Internal Medicine, Medical University of Lublin, Staszica 16 St., 20-081, Lublin, Poland
Chair and Department of Internal Medicine, Medical University of Lublin, Staszica 16 St., 20-081, Lublin, Poland
Ann Agric Environ Med. 2025;32(1):98-103
KEYWORDS
TOPICS
ABSTRACT
Introduction and objective:
Obstructive sleep apnea (OSA) is distinguished by recurrent partial or complete obstruction of the upper airways during sleep. The prevalence of OSA worldwide is estimated at 3–24% of the general population. Patients with OSA are predisposed to having endothelial dysfunction due to different mechanisms. The aim of a study was to assess the impact of 3 -month CPAP treatment on microcirculation among patients with OSA, and to determine changes in blood pressure after implemented therapy.
Material and methods:
The study included 30 patients with newly-diagnosed OSA. Microcirculation assessment was performed by Laser Doppler Flowmetry before and 3 months after implementation of CPAP therapy. Patients were also asked to perform measurements of blood pressure twice, 7 days prior to the appointment.
Results:
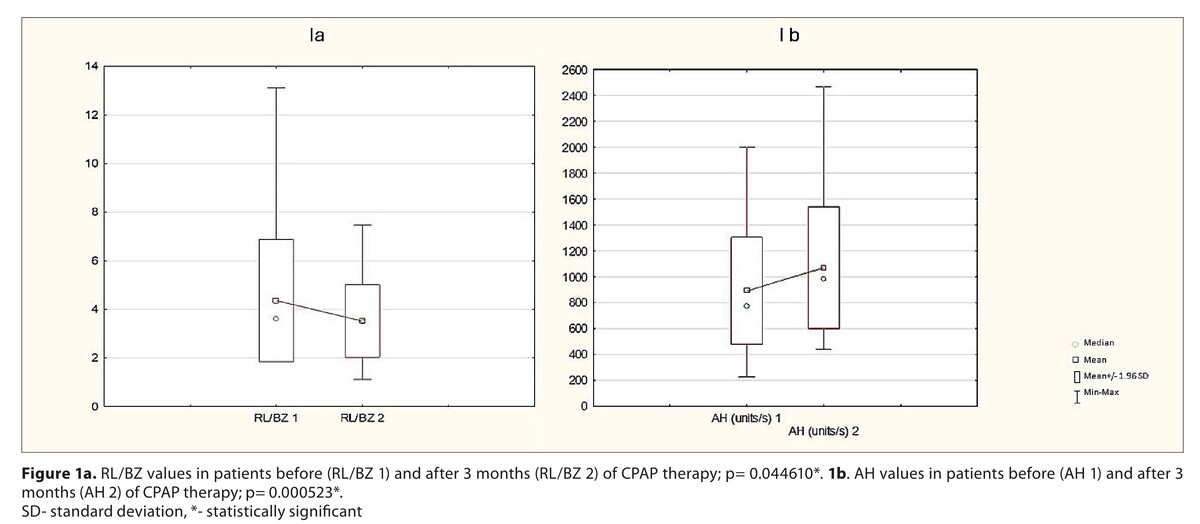
Improvement was observed in selected PORH parameters, such as AH, which was significantly increased after 3 months of treatment of CPAP (p<0.05). There was also a significant decrease in the RL/BZ parameter. Other PORH parameters did not differ significantly. Blood pressure, both diastolic and systolic, significantly decreased after therapy.
Conclusions:
Current study does not exactly explain the accurate mechanism underlying the changes of PORH after CPAP treatment among patients with OSA. However, it was demonstrated that 3 months adequate treatment improved endothelial function among the studied group. Assessment of microcirculation by LDF PORH protocol is a promising method, due to simplicity for the examinator, and non-invasive procedure. Due to the small study group, further investigation of microcirculation among patients with OSA should be performed, including the influence of co-morbidities and medications intake.
Obstructive sleep apnea (OSA) is distinguished by recurrent partial or complete obstruction of the upper airways during sleep. The prevalence of OSA worldwide is estimated at 3–24% of the general population. Patients with OSA are predisposed to having endothelial dysfunction due to different mechanisms. The aim of a study was to assess the impact of 3 -month CPAP treatment on microcirculation among patients with OSA, and to determine changes in blood pressure after implemented therapy.
Material and methods:
The study included 30 patients with newly-diagnosed OSA. Microcirculation assessment was performed by Laser Doppler Flowmetry before and 3 months after implementation of CPAP therapy. Patients were also asked to perform measurements of blood pressure twice, 7 days prior to the appointment.
Results:
Improvement was observed in selected PORH parameters, such as AH, which was significantly increased after 3 months of treatment of CPAP (p<0.05). There was also a significant decrease in the RL/BZ parameter. Other PORH parameters did not differ significantly. Blood pressure, both diastolic and systolic, significantly decreased after therapy.
Conclusions:
Current study does not exactly explain the accurate mechanism underlying the changes of PORH after CPAP treatment among patients with OSA. However, it was demonstrated that 3 months adequate treatment improved endothelial function among the studied group. Assessment of microcirculation by LDF PORH protocol is a promising method, due to simplicity for the examinator, and non-invasive procedure. Due to the small study group, further investigation of microcirculation among patients with OSA should be performed, including the influence of co-morbidities and medications intake.
REFERENCES (23)
1.
Bjork S, Jain D, Marliere MH, et al. Obstructive Sleep Apnea, Obesity Hypoventilation Syndrome, and Pulmonary Hypertension: A State-of-the-Art Review. Sleep Med Clin. 2024;19(2):307–325. doi:10.1016/j.jsmc.2024.02.009.
2.
Lv R, Liu X, Zhang Y, et al. Pathophysiological mechanisms and therapeutic approaches in obstructive sleep apnea syndrome. Signal Transduct Target Ther. 2023;8(1):218. doi:10.1038/s41392-023-01496-3.
3.
Liu L, Wang Y, Hong L, et al. Obstructive Sleep Apnea and Hypertensive Heart Disease: From Pathophysiology to Therapeutics. Rev Cardiovasc Med. 2023;24(12):342. doi:10.31083/j.rcm2412342.
4.
Chiu HY, Chen PY, Chuang LP, et al. Diagnostic Accuracy of the Berlin Questionnaire, STOP-BANG, STOP, and Epworth Sleepiness Scale in Detecting Obstructive Sleep Apnea: A Bivariate Meta-Analysis. Sleep Med Rev. 2017;36:57–70. https://doi.org/10.1016/j.smrv....
5.
Platon AL, Stelea CG, Boișteanu O, et al. An Update on Obstructive Sleep Apnea Syndrome-A Literature Review. Medicina (Kaunas). 2023;59(8):1459. doi:10.3390/medicina59081459.
6.
Yan Z, Xu Y, Li K, et al. The correlation between frailty index and incidence, mortality in obstructive sleep apnea: Evidence from NHANES. Heliyon. 2024;10(12):e32514. doi:10.1016/j.heliyon.2024.e32514.
7.
Spille J, Conrad J, Sengebusch A, et al. Preferences and experiences regarding the treatment of obstructive sleep apnea with mandibular advancement splints – a cross-sectional pilot survey. Cranio. 2024;42(3):298–304. doi:10.1080/08869634.2021.1962148.
8.
Mastino P, Rosati D, de Soccio G, et al. Oxidative Stress in Obstructive Sleep Apnea Syndrome: Putative Pathways to Hearing System Impairment. Antioxidants (Basel). 2023;12(7):1430. doi:10.3390/antiox12071430.
9.
de Lima EA, Castro SS, Viana-Júnior AB, et al. Could an increased risk of obstructive sleep apnoea be one of the determinants associated with disability in individuals with cardiovascular and cerebrovascular diseases? Sleep Breath. 2024;28(3):1187–1195. doi:10.1007/s11325-024-02989-3.
10.
Di Lorenzo B, Scala C, Mangoni AA, et al. A Systematic Review and Meta-Analysis of Mean Platelet Volume and Platelet Distribution Width in Patients with Obstructive Sleep Apnoea Syndrome. Biomedicines. 2024;12(2):270. doi:10.3390/biomedicines12020270.
11.
Zhang Y, Wang H, Yang J, et al. Obstructive Sleep Apnea Syndrome and Obesity Indicators, Circulating Blood Lipid Levels, and Adipokines Levels: A Bidirectional Two-Sample Mendelian Randomization Study. Nat Sci Sleep. 2024;16:573–583. doi:10.2147/NSS.S460989.
12.
Lin PW, Lin HC, Chang CT, et al. Decreased Peripapillary and Macular Vascular Densities in Patients with Moderate/Severe Obstructive Sleep Apnea/Hypopnea Syndrome. Nat Sci Sleep. 2023;15:1–12. doi:10.2147/NSS.S384372.
13.
Pinilla L, Benítez ID, Gracia-Lavedan E, et al. Metabolipidomic Analysis in Patients with Obstructive Sleep Apnea Discloses a Circulating Metabotype of Non-Dipping Blood Pressure. Antioxidants (Basel). 2023;12(12):2047. doi:10.3390/antiox12122047.
14.
Cracowski JL, Roustit M. Current Methods to Assess Human Cutaneous Blood Flow: An Updated Focus on Laser-Based-Techniques. Microcirculation. 2016;23(5):337–344. https://doi.org/10.1111/micc.1....
15.
Tessema B, Sack U, König B, et al. Effects of Intermittent Hypoxia in Training Regimes and in Obstructive Sleep Apnea on Aging Biomarkers and Age-Related Diseases: A Systematic Review. Front Aging Neurosci. 2022;14:878278. doi:10.3389/fnagi.2022.878278.
16.
Iredahl F, Löfberg A, Sjöberg F, et al. Non-Invasive Measurement of Skin Microvascular Response during Pharmacological and Physiological Provocations. PLoS One. 2015;10(8):e0133760. doi:10.1371/journal.pone.0133760.
17.
Balasubramanian G, Chockalingam N, Naemi R. A systematic evaluation of cutaneous microcirculation in the foot using post-occlusive reactive hyperemia. Microcirculation. 2021;28(5):e12692. doi:10.1111/micc.12692.
18.
Shirazi BR, Valentine RJ, Lang JA. Reproducibility and normalization of reactive hyperemia using laser speckle contrast imaging. PLoS One. 2021;16(1):e0244795. doi:10.1371/journal.pone.0244795.
19.
Caballero-Eraso C, Muñoz-Hernández R, Asensio Cruz MI, et al. Relationship between the endothelial dysfunction and the expression of the β1-subunit of BK channels in a non-hypertensive sleep apnea group. PLoS One. 2019;14(6):e0217138. doi:10.1371/journal.pone.0217138.
20.
Muñoz-Hernandez R, Vallejo-Vaz AJ, Sanchez Armengol A, et al. Obstructive sleep apnoea syndrome, endothelial function and markers of endothelialization. Changes after CPAP. PLoS One. 2015;10(3):e012209. doi:10.1371/journal.pone.0122091.
21.
Gryglewska B, Głuszewska A, Zarzycki B, et al. Post-occlusive reactive hyperemic response of skin microcirculation among extremely obese patients in the short and long term after bariatric surgery. Microcirculation. 2020;27(3):e12600. doi:10.1111/micc.126001.
22.
Lavalle S, Masiello E, Iannella G, et al. Unraveling the Complexities of Oxidative Stress and Inflammation Biomarkers in Obstructive Sleep Apnea Syndrome: A Comprehensive Review. Life (Basel). 2024;14(4):425. doi: 10.3390/life14040425.
23.
Bakker JP, Baltzis D, Tecilazich F, et al. The Effect of Continuous Positive Airway Pressure on Vascular Function and Cardiac Structure in Diabetes and Sleep Apnea. A Randomized Controlled Trial. Ann Am Thorac Soc. 2020;17(4):474–483. doi:10.1513/AnnalsATS.201905-378OC.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.