Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
Editor's Choice
CASE REPORT
A rare case of spinal dural arteriovenous fistula in a 22-year-old farmer
1
Department of Neurosurgery, Functional and Stereotactic Neurosurgery, Collegium Medicum, Nicolaus Copernicus University, Bydgoszcz, Poland
2
Department of Neurosurgery and Neurology, Jan Biziel University Hospital No 2, Collegium Medicum, Nicolaus Copernicus University, Bydgoszcz, Poland
3
Students’ Scientific Circle, Department of Neurosurgery and Neurology, Jan Biziel University Hospital No 2, Collegium
Medicum, Nicolaus Copernicus University, Bydgoszcz, Poland
4
Department of Radiology, Jan Biziel University Hospital No. 2, Collegium Medicum Nicolaus Copernicus University, Bydgoszcz, Poland
5
Department of Neurology and Clinical Neurophysiology, Collegium Medicum, Nicolaus Copernicus University, Bydgoszcz, Poland
Corresponding author
Sara Kierońska-Siwak
Department of Neurosurgery, Functional and Stereotactic Neurosurgery, Collegium Medicum, Nicolaus Copernicus University, Bydgoszcz, Poland
Department of Neurosurgery, Functional and Stereotactic Neurosurgery, Collegium Medicum, Nicolaus Copernicus University, Bydgoszcz, Poland
KEYWORDS
TOPICS
ABSTRACT
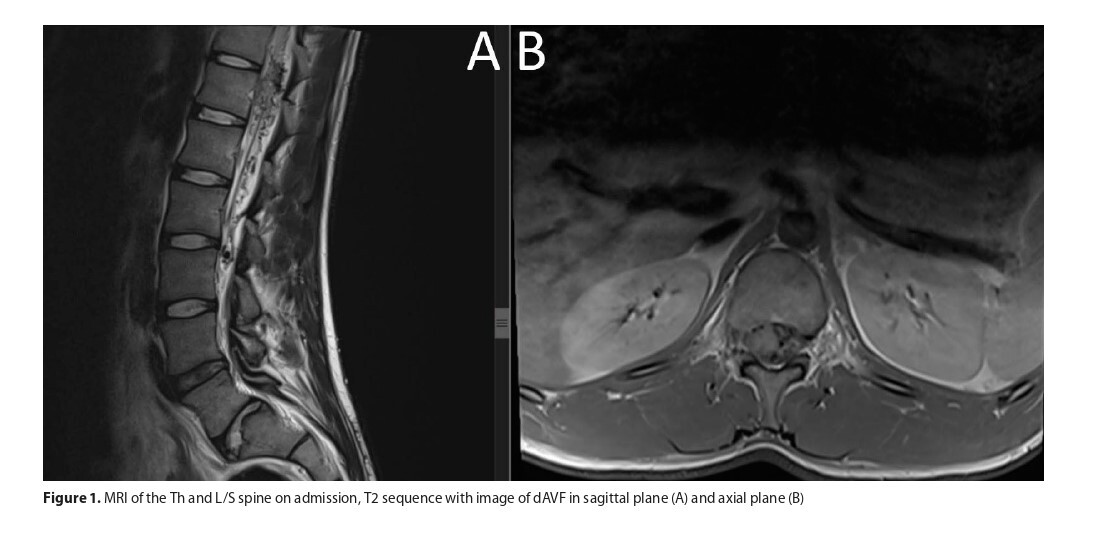
Spinal Dural Arteriovenous Fistulas (DAVFs) are rare vascular malformations characterized by abnormal connections betweena spinal artery and venous plexus. Though uncommon, DAVFs can be misdiagnosed due to their presentation with nonspecific symptoms, leading to potential treatment delays or incorrect procedures. This case report presents a 22-year-old male farmer admitted with gradual lower limb muscle weakness and urinary retention. Despite no trauma history, his recent exposure to chemicals raised concerns. Neurological examination revealed significant mobility impairment, particularly in the left leg, alongside sensory deficits. MRI findings demonstrated spinal cord oedema and venous dilatation, suggesting DAVF. The patient underwent successful endovascular embolization, with a post-operative course free of complications. This case highlights the challenges in diagnosing DAVF and underscores the importance of timely intervention.
REFERENCES (19)
1.
Alkhaibary A, Alharbi A, Alnefaie N, et al. Spinal dural arteriovenous fistula: a comprehensive review of the history, classification systems, management, and prognosis. Chin Neurosurg J. 2024;10(1). doi:10.1186/s41016-023-00355-y.
2.
Kiyosue H, Matsumaru Y, Niimi Y, et al. Angiographic and clinical characteristics of thoracolumbar spinal epidural and dural arteriovenous fistulas. Stroke. 2017;48(12):3215–3222. doi:10.1161/STROKEAHA.117.019131.
3.
Takai K. Spinal arteriovenous shunts: Angioarchitecture and historical changes in classification. Neurol Med Chir (Tokyo). 2017;57(7):356–365. doi:10.2176/nmc.ra.2016-0316.
4.
Jia DT, Jacobs CS, Tang M, Shaibani A, Lukas R V. The Spinal Dural Arteriovenous Fistula in a Patient With Metastatic Renal Cell Carcinoma. Cureus. Published online May 28, 2021. doi:10.7759/cureus.15303.
5.
Naga Shravan Kumar K, Visvanathan K, Swamiyappan SS, Dhanasekaran J, Joseph S, Krishnamurthy G. Surgical management of spinal dural arteriovenous fistula – A single centre experience. Interdiscip Neurosurg. 2022;28. doi:10.1016/j.inat.2022.101500.
6.
SucuoÄa&lu H, Aktürk A. Spinal dural arteriovenous fistula: A rare cause of progressive myelopathy and bladder and bowel dysfunction. Turk J Phys Med Rehabil. 2020;66(2):219–222. doi:10.5606/TFTRD.2020.3732.
7.
Ramón JF, Garcia Rairan L, Araque Y, Fuentes S, Useche N. Rupture of a Spinal Dural Arteriovenous Fistula as a Differential Diagnosis of a Coronary Syndrome: Case Report. Neurosurgery Practice. 2023;4(3). doi:10.1227/neuprac.0000000000000050.
8.
Mizutani K, Consoli A, Di Maria F, et al. Intradural spinal cord arteriovenous shunts in a personal series of 210 patients: novel classification with emphasis on anatomical disposition and angioarchitectonic distribution, related to spinal cord histogenetic units. J Neurosurg Spine. 2021;34(6):920–930. doi:10.3171/2020.9.SPINE201258.
9.
Yu JX, Hong T, Krings T, et al. Natural history of spinal cord arteriovenous shunts: An observational study. Brain. 2019;142(8):2265–2275. doi:10.1093/brain/awz153.
10.
Bretonnier M, Hénaux PL, Gaberel T, et al. Spinal Dural Arteriovenous Fistulas: Clinical Outcome after Surgery versus Embolization: A Retrospective Study Running Title: SDAVF: Clinical Outcome after Surgery versus Embolization; 2019.
11.
Wang P, Zhang L, Zhang W, et al. Dural arteriovenous fistula with spinal dural arteriovenous fistula: a case report and review of the literature. J Med Case Rep. 2023;17(1). doi:10.1186/s13256-023-04170-y.
12.
Msheik A, Al Mokdad Z, Gerges T, Aoude A. Spinal Dural Arteriovenous Fistula: Insights Into Operative Management. Cureus. Published online May 2, 2023. doi:10.7759/cureus.38448.
13.
Cenzato M, Debernardi A, Stefini R, et al. Spinal dural arteriovenous fistulas: Outcome and prognostic factors. Neurosurg Focus. 2012;32(5). doi:10.3171/2012.2.FOCUS1218.
14.
Vercelli GG, Minardi M, Bergui M, Zenga F, Garbossa D, Cofano F. Spinal dural and epidural arteriovenous fistula: Recurrence rate after surgical and endovascular treatment. Front Surg. 2023;10. doi:10.3389/fsurg.2023.1148968.
15.
Tanaka T, Yamane F, Sashida R, et al. Delayed Diagnosis of Spinal Dural Arteriovenous Fistula: A Case Report and Scoping Review. J Clin Med. 2024;13(3). doi:10.3390/jcm13030711.
16.
Fox S, Hnenny L, Ahmed U, Meguro K, Kelly ME. Spinal dural arteriovenous fistula: a case series and review of imaging findings. Spinal Cord Ser Cases. 2017;3(1). doi:10.1038/scsandc.2017.24.
17.
Zanin L, Di Bonaventura R, Agosti E, et al. Surgery versus endovascular treatment for spinal dural arteriovenous fistulas: a multicenter experience and systematic literature review. Neurosurg Rev. 2024;47(1). doi:10.1007/s10143-024-02443-8.
18.
Rodriguez J, Nagornaya N, Margolesky J, Saigal G. Unmasking of a spinal dural AV fistula on MRI following steroid administration. Egypt J Radiol Nuclear Med. 2022;53(1). doi:10.1186/s43055-022-00863-4.
19.
Szmygin P, Szmygin M, Roman T, Jargiełło T, Rola R. Endovascular embolisation as minimally-invasive treatment for spinal dural arteriovenous fistulas — evaluation of long-term results. Neurol Neurochir Pol. 2023;57(3):305–309. doi:10.5603/PJNNS.a2023.0027.
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.