Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
CASE REPORT
A new form of neurotherapy for a patient with anxiety disorder and anomic aphasia after
neurosurgery for a ruptured brain aneurysm post-COVID-19
1
Prof. B. Frańczuk Orthopaedic and Rehabilitation Hospital in Lesser Poland, Kraków, Poland
2
The Old Polish Academy of Applied Sciences, Kielce, Poland
3
Institute of Rural Health, Lublin, Poland
4
Chair of Neuropsychology and Neurorehabilitation, The Andrzej Frycz Modrzewski University, Kraków, Poland
Corresponding author
Maria Pąchalska
Chair of Neuropsychology and Neurorehabilitation, The Andrzej Frycz Modrzewski University, Kraków, Poland
Chair of Neuropsychology and Neurorehabilitation, The Andrzej Frycz Modrzewski University, Kraków, Poland
Ann Agric Environ Med. 2023;30(2):331-341
KEYWORDS
TOPICS
ABSTRACT
Introduction and Objective:
The aim of this study is to evaluate the effectiveness of a new, neuromarker-based form of neurotherapy for a patient with anxiety disorders and anomic aphasia after a neurosurgical operation for a ruptured brain aneurysm of the left middle cerebral artery (MCA), detected after COVID-19.
Case Report:
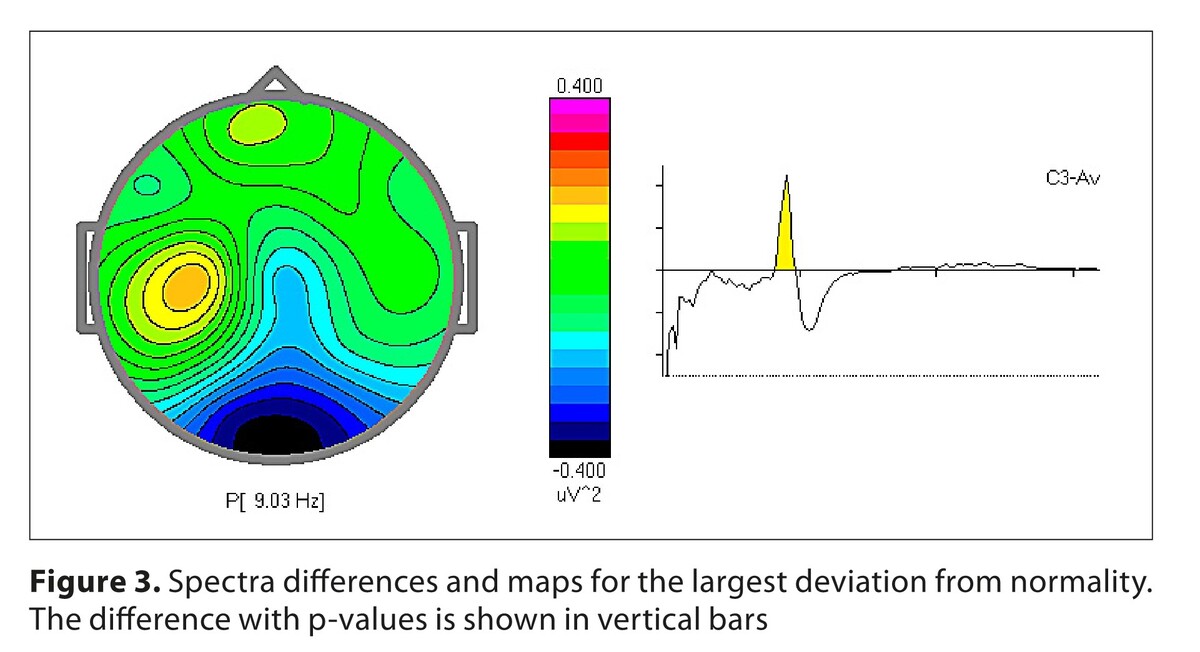
A 78-year-old right-handed patient, not previously treated for any chronic diseases except stage II hypertension, contracted COVID-19, confirmed by real time RT- PCR. He was treated on an outpatient basis. Two months later, he developed an unusually severe headache and disorientation. A ruptured brain aneurysm of the left MCA was diagnosed. The patient underwent a neurosurgical operation – clipping– very well, with no neurological or neuropsychiatric disorders, except for mild aphasia and occasional anxiety attacks. Four weeks after surgery, anxiety disorder and mild aphasia worsened. High levels of anxiety on the Hospital Anxiety and Depression (HAD) Scale, and mild anomic aphasia in the Boston Naming Test (BNT) was found. A functional neuromarker of anxiety in comparision to a normative database (Human Brain Index, HBI) was detected. The patient was offered a new, neuromarker-based form of neurotherapy, which proved effective in reducing the disorders. The patient improved in social communication and is gradually returning to social activities.
Conclusion:
In patients with anxiety disorders, anomic aphasia and related difficulties in social functioning after aSAH, especially after COVID-19, multidimensional diagnosis and therapy, preferably based on functional neuromarkers, is needed. HBI methodology can be successfully used in the neurodiagnosis and implementation of individualized neurotherapy for such patients.
The aim of this study is to evaluate the effectiveness of a new, neuromarker-based form of neurotherapy for a patient with anxiety disorders and anomic aphasia after a neurosurgical operation for a ruptured brain aneurysm of the left middle cerebral artery (MCA), detected after COVID-19.
Case Report:
A 78-year-old right-handed patient, not previously treated for any chronic diseases except stage II hypertension, contracted COVID-19, confirmed by real time RT- PCR. He was treated on an outpatient basis. Two months later, he developed an unusually severe headache and disorientation. A ruptured brain aneurysm of the left MCA was diagnosed. The patient underwent a neurosurgical operation – clipping– very well, with no neurological or neuropsychiatric disorders, except for mild aphasia and occasional anxiety attacks. Four weeks after surgery, anxiety disorder and mild aphasia worsened. High levels of anxiety on the Hospital Anxiety and Depression (HAD) Scale, and mild anomic aphasia in the Boston Naming Test (BNT) was found. A functional neuromarker of anxiety in comparision to a normative database (Human Brain Index, HBI) was detected. The patient was offered a new, neuromarker-based form of neurotherapy, which proved effective in reducing the disorders. The patient improved in social communication and is gradually returning to social activities.
Conclusion:
In patients with anxiety disorders, anomic aphasia and related difficulties in social functioning after aSAH, especially after COVID-19, multidimensional diagnosis and therapy, preferably based on functional neuromarkers, is needed. HBI methodology can be successfully used in the neurodiagnosis and implementation of individualized neurotherapy for such patients.
ACKNOWLEDGEMENTS
The authors extend their thanks to the entire neuropsychology team at the Reintegrative and Teaching Center of the Polish Neuropsychological Society, where we acquired the methods in the field of neuroscience relating to diagnosis
and treatment. In particular, we would like to thank Prof. Juri D. Kropotov for his great help in the interpretation of the results, and also Prof. Bruce D. MacQueen, Dr. Elżbieta Zając and Dr. Jan Bajger for their invaluable comments during the
writing of this article.
REFERENCES (85)
1.
Sadeghi Dousari A, Taati Moghadam M, Satarzadeh N. COVID-19 (Coronavirus Disease 2019): A New Coronavirus Disease. Infect Drug Resist. 2020;13:2819–2828. https://doi:10.2147/IDR.S25927....
2.
Gorbalenya AE, Baker SC, Baric RS, et al. The species Severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol. 2020;5(4):536–544. https://doi: 10.1038/s41564-020-0695-z.
4.
Fiani B, Fowler JB, Figueras RA, et al. Ruptured cerebral aneurysms in COVID-19 patients: A review of literature with case examples. Surg Neurol Int. 2021;26(12):187. doi:10.25259/SNI_214_2021.
5.
Taquet M, Geddes JR, Husain M, et al. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. The Lancet Psychiatry 2021;8:416–27. https://doi:10.1016/S2215-0366....
6.
Aknin LB, De Neve J E, Dunn EW, et al. The neurological consequences of contracting COVID-19. The Lancet’s COVID-19. Commission Mental Health Task Force. Acta Neuropsychologica, 2021;19(3):301–305. https://doi:10.5604/01.3001.00....
7.
Almeria M, Cejudo JC, Sotoca J, Deus J, Krupinski J. Cognitive profile following COVID-19 infection: Clinical predictors leading to neuropsychological impairment. Brain Behav Immun Health. 2020; 9:100163. doi:10.1016/j.bbih.2020.100163.
8.
Pąchalska M. Goal-oriented neuropsychological rehabilitation with EEG neurofeedback for a visual artist with PTSD resulting from SARS-CoV-2 infection, followed by a severe course of neuroCOVID and the sequele of long term pharmacologically induced coma. Acta Neuropsychologica. 2022;20(4):485–514. https://doi:10.5604/01.3001.00....
9.
Petridis AK, Kamp MA, Cornelius JF, Beez T, Beseoglu K, Turowski B, Steiger HJ. Aneurysmal Subarachnoid Hemorrhage. Dtsch Arztebl Int. 2017;114(13):226–236. https://doi:10.3238/arztebl.20....
10.
Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, et al. Unruptured intracranial aneurysms: Natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 2003;362:103–10.
11.
Wiebers DO, Whisnant JP, Huston J 3rd, et al. International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003;362(9378):103–10. doi:10.1016/s0140-6736(03)13860-3.
12.
Zacharia BE, Hickman ZL, Grobelny BT, et al. Epidemiology of aneurysmal subarachnoid hemorrhage. Neurosurg Clin N Am. 2010 Apr;21(2):221–33. https://doi: 10.1016/j.nec.2009.10.002.
13.
Etminan N, Chang HS, Hackenberg K, et al. Worldwide Incidence of Aneurysmal Subarachnoid Hemorrhage According to Region, Time Period, Blood Pressure, and Smoking Prevalence in the Population: A Systematic Review and Meta-analysis. JAMA Neurol. 2019; 76(5):588–597. https://doi:10.1001/jamaneurol....
14.
Taquet M, Luciano S, Geddes JR, et al. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130–40. https://doi:10.1016/S2215-0366....
15.
Roquer J, Cuadrado-Godia E, Guimaraens L, et al. Short- and long-term outcome of patients with aneurysmal subarachnoid hemorrhage. Neurology. 2020;29;95(13):e1819-e1829. doi:10.1212/WNL.0000000000010618.
16.
Morga R, Moskała M, Popiela T, et al. Recanalization of Embolized Endovascular Intracranial Aneurysms and Changes in the Blood Viscosity: A Pilot Study. Med Sci Monit. 2020;31;26:e919059. https://doi:10.12659/MSM.91905....
17.
Al-Khindi T, Macdonald RL, Schweizer TA. Cognitive and functional outcome after aneurysmal subarachnoid hemorrhage. Stroke. 2010;41:e519-e536.
18.
Raneri F, Rustemi O, Zambon G, et al. Neurosurgery in times of a pandemic: a survey of neurosurgical services during the COVID-19 outbreak in the Veneto region in Italy. Neurosurg Focus. 2020;49(6):E9. https://doi:10.3171/2020.9.FOC....
19.
MacQueen BD, MacQueen W.D. Neuro-COVID: A preliminary review. Acta Neuropsychologica. 2021;19(3): 389–402. doi: 10.5604/01.3001.0015.2692.
20.
Tang WK, Wang L, Kwok Chu Wong G, et al. Depression after Subarachnoid Hemorrhage: A Systematic Review. J Stroke. 2020;22(1):11–28. doi:10.5853/jos.2019.02103.
21.
Von Vogelsang AC, Forsberg C, Svensson M, et al. Patients experience high levels of anxiety 2 years following aneurysmal subarachnoid hemorrhage. World Neurosurg. 2015;83:1090–1097.
22.
Wong GK, Lam SW, Chan SS, et al. Neuropsychiatric disturbance after aneurysmal subarachnoid hemorrhage. J Clin Neurosci. 2014;21:1695–1698.
23.
Ackermark PY, Schepers VP, Post MW, et al. Longitudinal course of depressive symptoms and anxiety after aneurysmal subarachnoid hemorrhage. Eur J Phys Rehabil Med. 2017;53(1):98–104. https://doi: 10.23736/S1973-9087.16.04202-7.
24.
Pąchalska M, Kaczmarek BLJ, Kropotov JD. Ja utracone i odzyskane. [ang. Lost and foud Self] Kraków: AW IMPULS; 2021. ISBN 978-83-8095-933-0.
25.
Kropotov JD. Functional neuromarkers for psychiatry. San Diego: Academic Press, Elsevier; 2016.
26.
Thompson M, Thompson L. Neurofeedback. Wprowadzenie do podstawowych koncepcjipsychofizjologii stosowanej [ang. Neurofeedback. An introduction to the basic concepts of appliedpsychophysiology]. Wrocław: Biomed Neurotechnologie; 2012.
27.
Helm-Estabrooks N, Albert ML. Manual of aphasia therapy. Austin, TX: PRO-ED. 1991.
28.
Pąchalska M, Kaczmarek BLJ, Kropotov JD. Neuropsychologia kliniczna: od teorii do praktyki.[ang. Clinical neuropsychology: from theory to practice] Warszawa: WN PWN; 2014. ISBN 978-83-01-17841-3.
29.
Pąchalska M. Polska Wersja Bostońskiej Baterii Nazywania [Polish Version of the Boston Naming Battery]. Kraków: Fundacja na Rzecz Osób z Dysfunkcjami Mózgu; 1994.
30.
Kaplan E, Goodglass, H, Weintraub S. Boston Naming Test. Philadelphia: Lea & Febiger; 1983.
31.
del Toro ChM, Bislick LP, Comer M, et al. Development of a Short Form of the Boston Naming Test for Individuals with Aphasia. JSLHR. 2010;54(4):1089–100. https://doi:10.1044/1092-4388(...).
32.
Nicholas LE, Brookshire, R H, MacLennan DL, et al. The Boston Naming Test: Revised Administration and Scoring Procedures and Normative Information for Non-Brain-Damaged Adults. Clinical Aphasiology. Boston: College-Hill Press; 1988. pp. 103–15. ISBN 0-316-71779-7.
33.
Goodglass H, Kaplan E, Barresi B. Boston Diagnostic Aphasia Examination, 3rd edition. Austin: TX, Pro-Ed Inc.; 2001.
34.
Pąchalska M. Polska wersja Szpitalnej Skali Lęku i Depresji [Polish version of the Hospital Anxiety and Depression Scale, HADS). Kraków: Fundacja na Rzecz Osób z Dysfunkcjami Mózgu; 2006.
35.
Zigmond A, Snaith R. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983;67:361–70.
36.
Spinhoven PH, Ormel J, Sloekers PPA, Kempen GIJM, Speckens AEM, van Hemert AM. A validation study of the hospital anxiety and depression scale (HADS) in different groups of Dutch subjects. Psych Med. 1997;27:363–70. 23.
37.
Crawford JR, Henry JD, Crombie C, et al. Normative data for the HADS from a large non-clinical sample. Br J Clin Psychol. 2001;40:429–34.
38.
Onur OA, Fink GR, Kuramatsu JB, et al. Aneurysmatic subarachnoid haemorrhage. Neurol Res Pract. 2019;1:15. https://doi.org/10.1186/s42466....
39.
Ghosh R, Roy D, Ray A, Mandal A, Das S, Pal SK, Benito-León J. Non-Aneurysmal Subarachnoid Hemorrhage in COVID-19: A Case Report and Review of Literature. Med Res Arch. 2022 Jan;10(1):2673. https://doi:10.18103/mra.v10i1....
40.
Dodd WS, Jabbour PM, Sweid A, et al. Aneurysmal Subarachnoid Hemorrhage in Patients with Coronavirus Disease 2019 (COVID-19): A Case Series. World Neurosurg. 2021;153:e259-e264. https://doi: 10.1016/j.wneu.2021.06.092.
41.
Goldberg DL, Anenberg SC, Griffin D, McLinden, CA, Lu Z, Streets, D.G. Disentangling the impact of the COVID-19 lockdowns on urban NO2 from natural variability. Geophysical Research Letters. 2020; 47(17). https://doi.10.1029/2020GL0892....
42.
Krasemann S, Haferkamp U, Pfefferle S, et al. The blood-brain barrier is dysregulated in COVID-19 and serves as a CNS entry route for SARS-CoV-2. Stem Cell Reports. 2022;8;17(2):307–320. https://doi: 10.1016/j.stemcr.2021.12.011.
43.
Pąchalska M, Góral-Półrola J, Jarosz P. Neurotherapy in Parkinson’s Disease: the path forward after SARS-COV-2 infection and contracting COVID-19, and long COVID? Acta Neuropsychologica 2022;2(3): 275–290. https://doi:10.5604/01.3001.00....
44.
Luther E, McCarthy DJ, Brunet MC, Sur S, Chen SH, Sheinberg D, Hasan D, Jabbour P, Yavagal DR, Peterson EC, Starke RM. Treatment and diagnosis of cerebral aneurysms in the post-International Subarachnoid Aneurysm Trial (ISAT) era: trends and outcomes. J Neurointerv Surg. 2020;12(7):682–687. https://doi:10.1136/neurintsur.... Epub 2020 Jan 20. PMID: 31959634.
45.
Law SP, Kong AP, Lai LW, Lai C. Effects of context and word class on lexical retrieval in Chinese speakers with anomic aphasia. Aphasiology. 2015 Jan;29(1):81–100. https://doi:10.1080/02687038.2....
46.
Ryu H, Park CH. Structural Characteristic of the Arcuate Fasciculus in Patients with Fluent Aphasia Following Intracranial Hemorrhage: A Diffusion Tensor Tractography Study. Brain Sci. 2020;6;10(5):280. https://doi:10.3390/brainsci10....
47.
Budd MA, Kortte K, Cloutman L, Newhart M, Gottesman RF, Davis C, Heidler-Gary J, Seay MW, Hillis AE. The nature of naming errors in primary progressive aphasia versus acute post-stroke aphasia. Neuropsychology. 2010;24(5):581–9. https://doi:10.1037/a0020287.
48.
Fridriksson J, Guo D, Fillmore P, Holland A, Rorden C. Damage to the anterior arcuate fasciculus predicts non-fluent speech production in aphasia. Brain. 2013;136(Pt 11):3451–60. https://doi: 10.1093/brain/awt267.
49.
Foundas AL, Daniels SK, Vasterling JJ. Anomia: Case studies with lesion localization. Neurocase. 1998;4:35–43. https://doi:10.1080/1355479980....
50.
Binder JR. The Wernicke area: Modern evidence and a reinter -pretation. Neurology. 2015; 15;85(24):2170–5 https://doi:10.1212/WNL.000000....
51.
Jang S.H. Diffusion tensor imaging studies on arcuate fasciculus in stroke patients: A review. Front Hum Neurosci. 2013;7:1–7. https://doi: 10.3389/fnhum.2013.00749.
52.
Klaser K, Thompson EJ, Nguyen LH, et al. Anxiety and depression symptoms after COVID-19 infection: results from the COVID Symptom Study app. medRxiv. J Neurol Neurosurg Psychiatry. 2021;8: https://doi:10.1101/2021.07.07....
53.
Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. https://doi: 10.1016/S2215-0366(20)30168-1.
54.
Vindegaard N, Benros ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. 2020;89:531–42. https://doi:10.1016/j.bbi.2020....
55.
Klaser K, Thompson EJ, Nguyen LH, et al. Anxiety and depression symptoms after COVID-19 infection: results from the COVID Symptom Study app J Neurol Neurosurg Psychiatry. 2021;92(12):1254–1258. doi:10.1136/jnnp-2021-327565.
56.
Morris PG, Wilson JT, Dunn L. Anxiety and depression after spontaneous subarachnoid hemorrhage. Neurosurgery. 2004;54(1):47–54. https://doi:10.1227/01.neu.000....
57.
Hesdorffer D. Comorbidity between neurological illness and psychiatric disorders. CNS Spectrums 2016;21(3):230–238. https://doi:10.1017/S109285291....
58.
Pąchalska M. Rehabilitacja neuropsychologiczna. [ang. Neuro-psychological rehabilitation]. Lublin: Wydawnictwo UMCS; 2008. ISBN 978-83-227-2741-6.
59.
Halls G, Cooper PJ, Creswell C. Social communication deficits: Specific associations with Social Anxiety Disorder. J Affect Disord. 2015; 1;172:38–42. https://doi:10.1016/j.jad.2014....
60.
Rapee RM, Spence SH. The etiology of social phobia: empirical evidence and an initial model. Clin Psychol Rev. 2004;24(7):737–67. https://doi:10.1016/j.cpr.2004.... PMID: 15501555.
61.
Pickard H, Rijsdijk F, Happé F, Mandy W. Are Social and Communication Difficulties a Risk Factor for the Development of Social Anxiety? J Am Acad Child Adolesc Psychiatry. 2017;56(4):344–351.e3. https://doi:10.1016/j.jaac.201....
62.
Brown AS, Nix LA. Age related changes in the tip-of-the-tongue experience. Am J Psychol. 1996;1:79–91. https://doi.org/10.2307/142292....
63.
Schwartz BL. Sparkling at the end of the tongue: the etiology of tip-of-the-tongue phenomenology. Psychon Bull Rev. 1999;6(3):379–93. https://doi.10.3758/bf03210827.
64.
Mason C, Nickels L. Are single-word picture naming assessments a valid measure of word retrieval in connected speech? Int J Speech Lang Pathol. 2022;24(1):97–109. https://doi: 10.1080/17549507.2021.1966098.
65.
Dodd WS, Laurent D, Dumont AS, Hasan DM, Jabbour PM, Starke RM, Hosaka K, Polifka AJ, Hoh BL, Chalouhi N. Pathophysiology of Delayed Cerebral Ischemia After Subarachnoid Hemorrhage: A Review. J Am Heart Assoc. 2021;3;10(15):e021845. doi:10.1161/JAHA.121.021845.
66.
Velat GJ, Kimball MM, Mocco JD, Hoh BL. Vasospasm after aneurysmal subarachnoid hemorrhage: review of randomized controlled trials and meta-analyses in the literature. World Neurosurg. 2011;76:446–454. https://doi:10.1016/j.wneu.201....
67.
Pachalska M, Łukowicz M, Kropotov JD, et al. Evaluation of differentiated neurotherapy programs for a patient after severe TBI and long term coma using event-related potentials. Med Sci Monit. 2011;17(10):CS120–8. https://doi: 10.12659/msm.881970.
68.
Pąchalska M, Kropotov ID, Mańko G, Lipowska M, Rasmus A, Łukaszewska B, Bogdanowicz M, Mirski A. Evaluation of a neurotherapy program for a child with ADHD with Benign Partial Epilepsy with Rolandic Spikes (BPERS) using event-related potentials. Med Sci Monit. 2012;18(11):CS94–104. doi:10.12659/msm.883531.
69.
Graczyk M, Pąchalska M, Ziółkowski A, et al. Neurofeedback training for peak performance. Ann Agric Environ Med. 2014;21(4):871–5. https://doi:10.5604/12321966.1....
70.
Chrapusta A, Pąchalska M, Wilk-Frańczuk M, et al. Evaluation of the effectiveness of neurofeedback in the reduction of Posttraumatic stress disorder (PTSD) in a patient following high-voltage electric shock with the use of ERPs. Ann Agric Environ Med. 2015;22(3):556–63. https://doi:10.5604/12321966.1....
71.
Mirski A, Pąchalska M, Moskała M, et al. Neuromarkers of anxiety and depression in a patient after neuro-ophthalmic surgery of the meningioma – the effect of individually-tailored tDCS and neurofeedback. Ann Agric Environ Med. 2015;22(4):718–23. https://doi:10.5604/12321966.1....
72.
Chrapusta A, Kropotov JD, Pąchalska M. Neuromarkers of Post-Traumatic Stress Disorder (PTSD) in a patient after bilateral hand amputation – ERP case study. Ann Agric Environ Med. 2017;24(2):265–270.
73.
Pąchalska M, Nowaczyk N. Event-related potentials studies of PTSD after infection of SARS-CoV-2 and NeuroCOVID-19. Acta Neuropsychologica 2021;19(3):347–360; https://doi:10.5604/01.3001.00....
74.
Pąchalska M, Góral-Półrola J, Chojnowska-Cwiąkała I. Effect of individually-tailored tDCS and symbolic art therapy for chronic associative prosopagnosia after infection by sars-cov-2, neurocovid-19 and ischemic stroke. Acta Neuropsychologica. 2022;19(3):329–345. https://doi:10.5604/01.3001.00....
75.
Kropotov JD. Quantitative EEG, event related potentials and neurotherapy. San Diego: Academic Press, Elsevier; 2009.
76.
Moore NC. A review of EEG biofeedback treatment of anxiety disorders. Clin Electroencephalogr. 2000 Jan;31(1):1–6. https://doi:10.1177/1550059400....
77.
Heller W, Etienne MA, Miller GA. Patterns of perceptual asymmetry in depression and anxiety: implications for neuropsychological models of emotion and psychopathology. J Abnorm Psychol. 1995;104(2):327–33. https://doi:10.1037//0021-843x....
78.
Heller W, Nitschke JB, Etienne MA, et al. Patterns of regional brain activity differentiate types of anxiety. J Abnorm Psychol. 1997;106(3):376–85. https://doi:10.1037//0021-843x....
79.
Wiedemann G, Pauli P, Dengler W, et al. Frontal brain asymmetry as a biological substrate of emotions in patients with panic disorders. Arch Gen Psychiatry. 1999;56(1):78–84. https://doi:10.1001/archpsyc.5....
80.
Ehlers A. Understanding and Treating Unwanted Trauma Memories in Posttraumatic Stress Disorder. Z Psychol. 2010;218(2):141–145. https://doi:10.1027/0044-3409/....
81.
Roy NA, Bak JH; International Brain Laboratory; Akrami A, Brody CD, Pillow JW. Extracting the dynamics of behavior in sensory decision-making experiments. Neuron. 2021;109(4):597–610.e6. https://doi:10.1016/j.neuron.2....
82.
Cadilhac DA, Andrew NE, Lannin NA, et al. Australian Stroke Clinical Registry Consortium. Quality of Acute Care and Long-Term Quality of Life and Survival: The Australian Stroke Clinical Registry. Stroke. 2017;48(4):1026–1032. https://doi:10.1161/STROKEAHA.....
83.
El Harchaoui I, Regragui W, Driss T, Mammad K, Ziri R, Ahami AOT. A study into the relationship between anxiety-depression and self-esteem disorder in patients with multiple sclerosis at the Rabat IBN Sina Hospital, Morocco. Acta Neuropsychologica. 2023;21(1):53–63. https://doi:10.5604/01.3001.00....
84.
Trystuła M, Pąchalska M. Comorbidities and Health-Related Quality of Life Following Revascularization for Asymptomatic Critical Internal Carotid Artery Stenosis Treated with Carotid Endarterectomy or Angioplasty with Stenting. Med Sci Monit 2019;25:4734–4743. https://doi:10.12659/MSM.91640....
85.
Trystuła M, Tomaszewski T, Pąchalska M. Health-related quality of life in ischaemic stroke survivors after carotid endarterectomy (CEA) and carotid artery stenting (CAS): confounder-controlled analysis. Advances in Interventional Cardiology. 2019;15(2):226–233. https://doi: 10.5114/aic.2019.84441.2019.
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.