Online first
Current issue
Archive
Special Issues
About the Journal
Publication Ethics
Anti-Plagiarism system
Instructions for Authors
Instructions for Reviewers
Editorial Board
Editorial Office
Contact
Reviewers
All Reviewers
2024
2023
2022
2021
2020
2019
2018
2017
2016
General Data Protection Regulation (RODO)
RESEARCH PAPER
A national registry-based study on uptake of the first dose of MMR vaccine in 380 administrative regions in Poland, 2013–2016–2020
1
Department of Prevention of Environmental Hazards, Allergology and Immunology, Medical University, Warsaw, Poland
2
School of Public Health, Centre of Postgraduate Medical Education, Warsaw, Poland
3
KR Consulting, Warsaw, Poland
4
State Medical University, Poltava, Ukraine
Corresponding author
Karolina Sobeczek
Department of Prevention of Environmental Hazards, Allergology and Immunology, Medical University of Warsaw, Warsaw, Poland
Department of Prevention of Environmental Hazards, Allergology and Immunology, Medical University of Warsaw, Warsaw, Poland
Ann Agric Environ Med. 2024;31(1):65-71
KEYWORDS
Polandvaccinationregional differencesvaccinesvaccine hesitancyMMR vaccine uptakevaccine coverage ratechildhood vaccination
TOPICS
ABSTRACT
Introduction and objective:
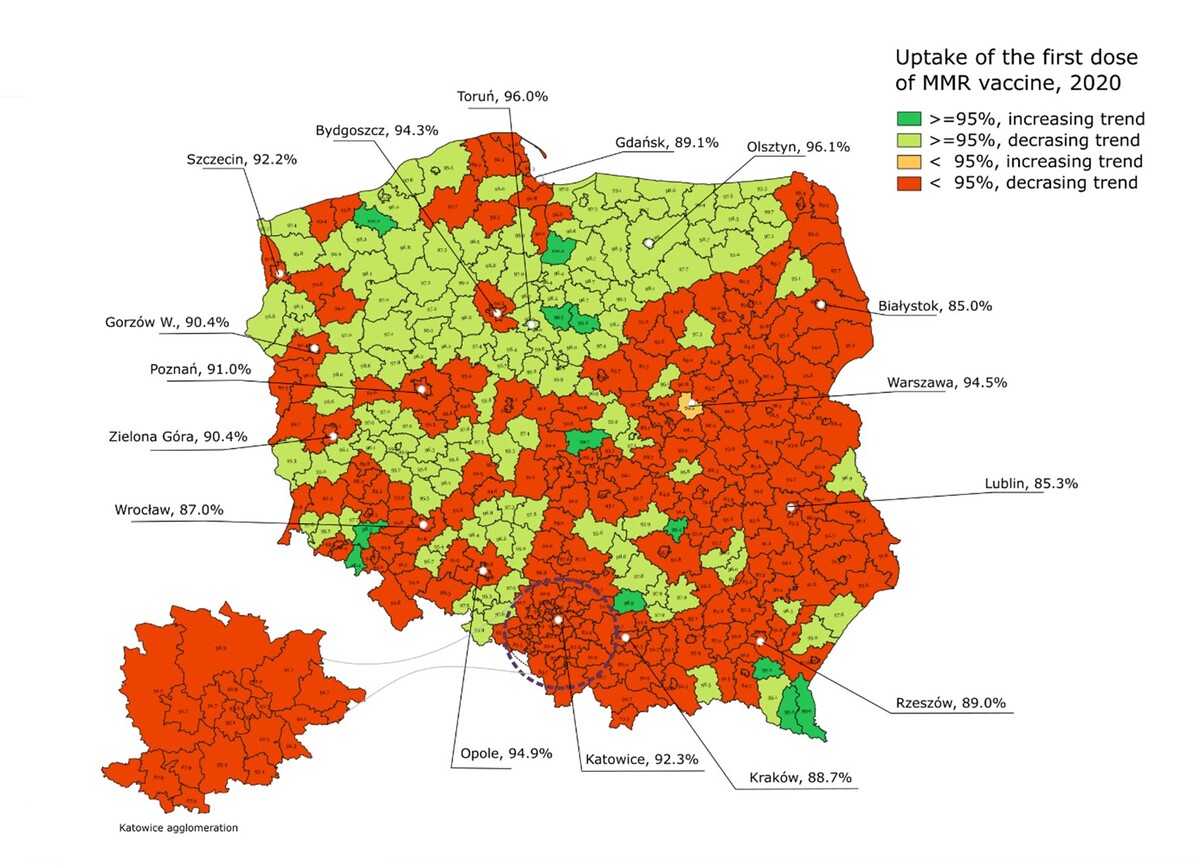
Regular monitoring of the measles, mumps, and rubella (MMR) vaccine uptake quickly exposes immunity gaps in the population. In Poland, the first dose of the MMR vaccine is mandatory for children between 13 and 15 months of life. This study aimed to assess the uptake of the first dose of MMR vaccine in 380 administrative counties in Poland in 2020, as well as to analyze the MMR vaccine uptake trends in 2013–2016–2020.
Material and methods:
This study is an epidemiological retrospective national registry-based analysis. Data on mandatory childhood vaccinations in all 380 counties in Poland were collected from the epidemiological reports of the State Sanitary Inspectorate territorial representatives. MMR vaccine uptake was calculated as the percentage of children who received the first dose of MRR vaccine to all children subject to mandatory vaccination in the county.
Results:
The uptake of the first dose of MMR vaccine decreased from 99.4% in 2013, to 95.5% in 2016 and 91.9% in 2020. In 2013, 93.2% of countys MMR vaccine uptake level reached the herd immunity level, followed by 77.1% of counties in 2016 and only 38.3% of countys in 2020. In 2020, two counties reached complete (100%) MMR vaccine uptake, and the lowest MMR vaccine uptake was 63.88%. Of the 380 counties in Poland, in 226 (61.1%) the MMR vaccine uptake level was lower than the herd immunity level, and a downward trend was observed. MMR vaccine uptake decreased with an increased number of residents in a county (r= -0.35; p<0.001).
Conclusions:
This study revealed that in 61% of administrative regions in Poland, the MMR vaccine uptake was below the herd immunity level. Regional differences in the MMR vaccine uptake were observed. A significant decrease in MMR vaccine uptake between 2013 – 2020 poses a risk of measles outbreaks.
Regular monitoring of the measles, mumps, and rubella (MMR) vaccine uptake quickly exposes immunity gaps in the population. In Poland, the first dose of the MMR vaccine is mandatory for children between 13 and 15 months of life. This study aimed to assess the uptake of the first dose of MMR vaccine in 380 administrative counties in Poland in 2020, as well as to analyze the MMR vaccine uptake trends in 2013–2016–2020.
Material and methods:
This study is an epidemiological retrospective national registry-based analysis. Data on mandatory childhood vaccinations in all 380 counties in Poland were collected from the epidemiological reports of the State Sanitary Inspectorate territorial representatives. MMR vaccine uptake was calculated as the percentage of children who received the first dose of MRR vaccine to all children subject to mandatory vaccination in the county.
Results:
The uptake of the first dose of MMR vaccine decreased from 99.4% in 2013, to 95.5% in 2016 and 91.9% in 2020. In 2013, 93.2% of countys MMR vaccine uptake level reached the herd immunity level, followed by 77.1% of counties in 2016 and only 38.3% of countys in 2020. In 2020, two counties reached complete (100%) MMR vaccine uptake, and the lowest MMR vaccine uptake was 63.88%. Of the 380 counties in Poland, in 226 (61.1%) the MMR vaccine uptake level was lower than the herd immunity level, and a downward trend was observed. MMR vaccine uptake decreased with an increased number of residents in a county (r= -0.35; p<0.001).
Conclusions:
This study revealed that in 61% of administrative regions in Poland, the MMR vaccine uptake was below the herd immunity level. Regional differences in the MMR vaccine uptake were observed. A significant decrease in MMR vaccine uptake between 2013 – 2020 poses a risk of measles outbreaks.
ACKNOWLEDGEMENTS
This study was carried out as a part of the scientific project funded by the National Centre for Research and Development within the Strategic Program of Scientific Research and Development “Social and economic development of Poland
in the conditions of globalizing markets”, grant number GOSPOSTRATEG-II/0007/2020-00.”
The authors express their thanks to the State Sanitary Inspectorate for the data sharing.
REFERENCES (38)
1.
GBD 2020, Release 1, Vaccine Coverage Collaborators. Measuring routine childhood vaccination coverage in 204 countries and territories, 1980–2019: a systematic analysis for the Global Burden of Disease Study 2020, Release 1. Lancet. 2021;398(10299):503–521. https://doi.org/10.1016/S0140-....
2.
Li X, Mukandavire C, Cucunubá ZM, et al. Estimating the health impact of vaccination against ten pathogens in 98 low-income and middle-income countries from 2000 to 2030: a modelling study. Lancet. 2021;397(10272):398–408. https://doi.org/10.1016/S0140-....
3.
Chang AY, Riumallo-Herl C, Perales NA, et al. The Equity Impact Vaccines May Have On Averting Deaths And Medical Impoverishment In Developing Countries. Health Aff (Millwood). 2018;37(2):316–324. https://doi.org/10.1377/hlthaf....
4.
Nandi A, Shet A. Why vaccines matter: understanding the broader health, economic, and child development benefits of routine vaccination. Hum Vaccin Immunother. 2020;16(8):1900–1904. https://doi.org/10.1080/216455....
5.
World Health Organization (WHO). Vaccines and immunization. https://www.who.int/health-top... (access: 2023.07.22).
6.
Greenwood B. The contribution of vaccination to global health: past, present and future. Philos Trans R Soc Lond B Biol Sci. 2014;369(1645):20130433. https://doi.org/10.1098/rstb.2....
7.
Gallagher KE, Kadokura E, Eckert LO, et al. Factors influencing completion of multi-dose vaccine schedules in adolescents: a systematic review. BMC Public Health. 2016;16:172. https://doi.org/10.1186/s12889....
8.
European Centre for Disease Prevention and Control (ECDC). Vaccine schedules in all countries in the EU/EEA. https://vaccine-schedule.ecdc.... (access: 2023.07.23).
9.
Singh P, Dhalaria P, Kashyap S, et al. Strategies to overcome vaccine hesitancy: a systematic review. Syst Rev. 2022;11(1):78. https://doi.org/10.1186/s13643....
10.
The Lancet Child Adolescent Health. Vaccine hesitancy: a generation at risk. Lancet Child Adolesc Health. 2019;3(5):281. https://doi.org/10.1016/S2352-....
11.
Troiano G, Nardi A. Vaccine hesitancy in the era of COVID-19. Public Health. 2021;194:245–251. https://doi.org/10.1016/j.puhe....
12.
de Figueiredo A, Simas C, Karafillakis E, et al. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020;396(10255):898–908. https://doi.org/10.1016/S0140-....
13.
Lane S, MacDonald NE, Marti M, et al. Vaccine hesitancy around the globe: Analysis of three years of WHO/UNICEF Joint Reporting Form data-2015-2017. Vaccine. 2018;36(26):3861–3867. https://doi.org/10.1016/j.vacc....
14.
Dubé E, Ward JK, Verger P, et al. Vaccine Hesitancy, Acceptance, and Anti-Vaccination: Trends and Future Prospects for Public Health. Annu Rev Public Health. 2021;42:175–191. https://doi.org/10.1146/annure....
15.
Schuster M, Eskola J, Duclos P, et al. Review of vaccine hesitancy: Rationale, remit and methods. Vaccine. 2015;33(34):4157–4160. https://doi.org/10.1016/j.vacc....
16.
Hübschen JM, Gouandjika-Vasilache I, Dina J. Measles. Lancet. 2022;399(10325):678–690. https://doi.org/10.1016/S0140-....
17.
World Health Organization (WHO). Immunization coverage. https://www.who.int/news-room/... (access: 2023.07.22).
18.
Bester JC. Measles and Measles Vaccination: A Review. JAMA Pediatr. 2016;170(12):1209–1215. https://doi.org/10.1001/jamape....
19.
Di Pietrantonj C, Rivetti A, Marchione P, et al. Vaccines for measles, mumps, rubella, and varicella in children. Cochrane Database Syst Rev. 2021;11(11):CD004407. https://doi.org/10.1002/146518....
20.
World Health Organization (WHO). Measles and rubella strategic framework: 2021–2030. https://www.who.int/publicatio... (access: 2023.07.22).
21.
Causey K, Fullman N, Sorensen RJD, et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: a modelling study. Lancet. 2021;398(10299):522–534. https://doi.org/10.1016/S0140-....
22.
European Centre for Disease Prevention and Control (ECDC). Measles. Annual Epidemiological Report for 2022. https://www.ecdc.europa.eu/sit... (access: 2023.07.24).
23.
Reczulska A, Tomaszewska A, Raciborski F. Level of Acceptance of Mandatory Vaccination and Legal Sanctions for Refusing Mandatory Vaccination of Children. Vaccines (Basel). 2022;10(5):811. https://doi.org/10.3390/vaccin....
24.
Włodarska A, Raciborski F. Characterisation of the online public debate od MMR vaccine against measles, mumps and rubella on the Polish Internet. Przegl Epidemiol. 2021;75(3):390–401. https://doi.org/10.32394/pe.75....
25.
National Insitute of Public Health, Warsaw, Poland. Waht is the number of vaccination refusal? https://szczepienia.pzh.gov.pl... (access: 2023.07.23).
26.
Furman FM, Zgliczyński WS, Jankowski M, et al. The State of Vaccine Confidence in Poland: A 2019 Nationwide Cross-Sectional Survey. Int J Environ Res Public Health. 2020;17(12):4565. https://doi.org/10.3390/ijerph....
27.
Spencer CN, Delamater PL. Examining vaccination coverage in Germany: spatiotemporal clustering of MMR coverage, 2008–14. Eur J Public Health. 2020;30(5):993–995. https://doi.org/10.1093/eurpub....
28.
Bocquier A, Ward J, Raude J, et al. Socioeconomic differences in childhood vaccination in developed countries: a systematic review of quantitative studies. Expert Rev Vaccines. 2017;16(11):1107–1118. https://doi.org/10.1080/147605....
29.
Tabacchi G, Costantino C, Napoli G, et al. Determinants of European parents’ decision on the vaccination of their children against measles, mumps and rubella: A systematic review and meta-analysis. Hum Vaccin Immunother. 2016;12(7):1909–1923. https://doi.org/10.1080/216455....
30.
Braczkowska B, Kowalska M, Braczkowski R, et al. Determinants of vaccine hesitancy. Przegl Epidemiol. 2017;71(2):227–236.
31.
Statistics of Poland. Administrative division of Poland. https://stat.gov.pl/en/regiona... (access: 2023.07.23).
32.
Chaabane S, Doraiswamy S, Chaabna K, Mamtani R, Cheema S. The Impact of COVID-19 School Closure on Child and Adolescent Health: A Rapid Systematic Review. Children (Basel). 2021;8(5):415. https://doi.org/10.3390/childr....
33.
Jankowski M, Lazarus JV, Kuchyn I, et al. One Year On: Poland’s Public Health Initiatives and National Response to Millions of Refugees from Ukraine. Med Sci Monit. 2023;29:e940223. https://doi.org/10.12659/MSM.9....
34.
Raciborski F, Samel-Kowalik P, Gujski M, et al. Factors Associated with a Lack of Willingness to Vaccinate against COVID-19 in Poland: A 2021 Nationwide Cross-Sectional Survey. Vaccines (Basel). 2021;9(9):1000. https://doi.org/10.3390/vaccin....
35.
Raciborski F, Tomaszewska A, Rakocy K, et al. The multidimensional nature of attitudes towards preventive vaccinations – a cross-sectional survey among Poles aged 15–39 years. Int J Occup Med Environ Health. 2023;36(2):214–228. https://doi.org/10.13075/ijome....
36.
Szczupak M, Augustyniak T, Sikorska K. The avoidance of vaccinations among people aged 0–18 years in pomorskie voivodeship in 2000–2017. Przegl Epidemiol. 2020;74(1):109–118. https://doi.org/10.32394/pe.74....
37.
Jędrzejek MJ, Mastalerz-Migas A. Influenza Vaccination Coverage, Motivators for, and Barriers to Influenza Vaccination among Healthcare Workers in Wroclaw, Poland. Int J Environ Res Public Health. 2022;19(3):1586. https://doi.org/10.3390/ijerph....
38.
Ganczak M, Gil K, Korzeń M, Bażydło M. Coverage and Influencing Determinants of Influenza Vaccination in Elderly Patients in a Country with a Poor Vaccination Implementation. Int J Environ Res Public Health. 2017;14(6):665. https://doi.org/10.3390/ijerph....
Share
RELATED ARTICLE
We process personal data collected when visiting the website. The function of obtaining information about users and their behavior is carried out by voluntarily entered information in forms and saving cookies in end devices. Data, including cookies, are used to provide services, improve the user experience and to analyze the traffic in accordance with the Privacy policy. Data are also collected and processed by Google Analytics tool (more).
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.
You can change cookies settings in your browser. Restricted use of cookies in the browser configuration may affect some functionalities of the website.